Transcription
YukonFirst NationMentalWellnessWor kbookAHTF 2010
Funding for this project was provided by Health Canada through the AboriginalHealth Transition Fund.The opinions expressed in this publication are those of the authors/researchersand do not necessarily reflect the official views of Health Canada or the Council ofYukon First Nations.The information in this toolkit can be used for non-commercial purposes only.
AcknowledgmentsThe Yukon First Nation Mental WellnessWorkbook is the work of many individualswho were involved in its research, reviewand compilation.In 2008, the Yukon First Nations Health andSocial Development Commission identifiedsix initiatives to be funded under theAboriginal Health Transition Fund (AHTF) –a fund established to assist the collaborationof federal, territorial and Aboriginalgovernments to help close gaps in Aboriginalhealth.Further acknowledgment includes the AHTF2009-2010 Mental Wellness Advisory Groupwhich provided direction and feedbackthroughout the process. They are: Sandy Washburn - Community WellnessCoordinator, First Nation of Na-cho NyakDun Rachel Byers - Director of Health andSocial, Little Salmon/Carmacks First Nation Lawrie Crawford - Director of Health andSocial, Carcross/Tagish First NationOne of these initiatives was to addressthe mental wellness of Yukon First Nationsand create a toolkit of resources for YukonFirst Nation front line workers, Yukon FirstNations Health and Social Directors andstaff. Margaret Smith/Reanna Sutton - Director/Acting Director of Health & Social, VuntutGwichin First NationThis workbook references the researchdocument - Mental Wellness Toolkit forFront Line Workers - created by Duu ChuuManagement (2010) for the AHTF. Gratitudegoes to this group for providing a roadmap for this document. A copy of theirfinal report, as presented to the Councilof Yukon First Nations (CYFN) Health andSocial Development Department, is availablethrough CYFN. Marie Fast - Clinical Manager, MentalHealth Services, Yukon GovernmentThis section acknowledges all those whocreated and contributed to this workbookincluding Duu Chuu Management, MarilynVan Bibber, Tandi Brown and HeatherHolland.Yukon First Nation Mental Wellness Workbook Lori Duncan - Health and SocialDevelopment Director, Council of Yukon FirstNations Leslie Knight - Community Member Michelle Tochacek - Manager for NonInsured Health Benefits in Yukon, IndianResidential Schools CoordinatorLori Duncan and Helen Stappers providedfact checking and editing support; AmandaLeslie assisted with production and editing,Tanya Handley was the layout artist and JenJones created the workbook.Funding for this publication was provided byHealth Canada.3
Over viewIn 2008, the Yukon First Nations Health andSocial Development Commission identifiedsix initiatives to be funded under theAboriginal Health Transition Fund (AHTF).This fund was established to assist thecollaboration of federal, territorial andAboriginal governments to identify andhelp close gaps in Aboriginal health. Oneof the initiatives was to address the issuesof mental wellness in Yukon First Nationcommunities.The focus of the mental wellness initiativewas to create a toolkit of resources forYukon First Nation front line workers, YukonFirst Nation Health and Social directors andstaff.The key deliverables for this initiativeincluded: A list of the mental health services inYukon. A definition of mental wellness from aYukon First Nation perspective. A list of promising practices. The development of a strategy and/orframework for a community action plan.GOALThe aim of this workbook is to takethe findings from the Mental WellnessToolkit for Front Line Workers document,along with other additional resources,to create a “hands on” tool thatYukon First Nation Health and SocialDepartments can draw informationfrom, use in planning and supportstrategic planning within their homeFirst Nation and amongst all YukonFirst Nations.In addition to the report and this workbook,the AHTF office designed a mental wellnessresource guide that outlines availableservices, their cultural safety componentsand questions that could be asked whencontacting the services or individuals.Another tool lists community wellnessagencies, services and programs in theform of a day book and includes contactinformation and available resources.These tools are available from the Councilof Yukon First Nations Health and SocialDevelopment Department at 393.9200.This workbook is a result of workcompleted by the consultants as well asthose acknowledged in the previous pages.4Yukon First Nation Mental Wellness Workbook
How to use this wor kbookThis workbook was developed to supportYukon First Nation Health and SocialDepartments in: program planning project evaluation proposal writing client supportThe focus is mental wellness, however, thetools provided can be used for a variety ofissues. Information found in each section isalso on the disk provided at the back of thisworkbook.The workbook is divided into eight sections.Each section has tools that you can printout and use for case management, clientassessment, planning programs, and/or writingproposals. The work sheets are designed to becopied or modified to best suit the needs ofindividual First Nations and clients.Section 1 describes the underlying causesof mental illness and their relationship to thedeterminants of health. Use this section as ateaching tool or in discussion about Yukon FirstNation mental wellness issues. Cut and pastethis information into a strategic action plan orproposal.Section 2 presents five pillars for a YukonFirst Nation Mental Wellness Strategy. Thissection draws on information gathered throughseveral Aboriginal Health Transition Fund andAboriginal Health Human Resources Initiative(AHHRI) projects. Cut and paste key findingsinto reports, presentations or proposals.Yukon First Nation Mental Wellness WorkbookSection 3 provides tools to help planning,proposal writing and working with clients andgroups. Print out the wellness indicators andshare them with community members or cutand paste them into a proposal.Section 4 provides step-by-step instructionson how to develop a mental wellness strategy.A template is also provided.Section 5 provides information on vicarioustrauma that may be experienced in theworkplace. It also provides a strategy on howto address this issue.Section 6 is a resource directory identifying“good ideas”, toolkits and materials developedby other jurisdictions. Internet addresses areprovided for most of the resources.The CD attached at theback of this book containsall the documents containedwithin this workbook as wellas three documents that maybe of use to your department.The documents are: Alianait Inuit Mental Wellness Action Plan,Toward Recovery & Well-Being The Community is Medicine Suicide PreventionTrauma Response and Community ResponseTeam Development Micro Manual Mental Health First Aid – Aboriginal and TorresStrait Islander Mental Health First Aid ManualReferences were provided in part by DuuChuu Management. Additional referenceswere included with the development of thisworkbook. References can also be used forfurther research for other projects.5
Mental Health, Substance Abuse and IndianResidential Schools – T he links“We tend to view mental illness and substanceuse disorders as two distinctly separate illnessesand in many cases they are,” says Dr. Franco J.Vaccarino. “Yet when the two disorders co-occurand are intertwined, treating just one disorderor treating the two disorders independentlyis insufficient and yet this is often commonpractice.” (Canadian Centre on SubstanceAbuse, November 17, 2009)A report from the March 2008 MentalWellness Focus Group Workshop declaredthat the mental health of First Nationpeople is in decline as a result of causessuch as drug and alcohol addictions andIndian Residential School trauma (CYFNHealth & Social Dept., 2008). It was alsoidentified that addictions are a symptomof mental health problems and there mustbe a link in the support services thataddress addictions and mental wellness.More recently, a 2009 report put out bythe Canadian Centre on Substance Abuse(CCSA) spotlights the co-occurrence ofmental health and substance use disorders,furthering the link between substance abuse,trauma and mental illness.The co-occurrence of substance use andmental wellness is not new within a FirstNation view. “First Nations, Inuit andMétis cultures, although diverse, broadlyunderstand well being or wellness tocome from a balance of body, mind, andspirit, closely tied to cultural identity, selfdetermination, community and family, andthe land.” (Mental Health Commission ofCanada, 2009, p.5).In other words, a holistic approach isrequired when looking at health and mentalwellness to ensure balance. The CCSA6report also validates the connection theYukon First Nations Health and SocialDevelopment Commission members havebeen making: the need for services thataddress mental wellness and addictionsconcurrently.When tasked with the job to support frontline workers in the area of mental healthand wellness, identifying definitions ofmental health was thought to be a startingpoint. The Kirby Report (Kirby and Keon,2004) defined mental health as more thanthe absence of illness - rather, it is aboutone’s ability to enjoy life and experiencewellness.“Mental health is the capacity to feel, thinkand act in ways that enhance one’s ability toenjoy life and deal with challenges. Expresseddifferently, mental health refers to variouscapacities including the ability to understandoneself and one’s life, relate to other peopleand respond to one’s environment, experiencepleasure and enjoyment, handle stress andwithstand discomfort, evaluate challengesand problems, pursue goals and interests,and explore choices and make decisions.”(Kirby and Keon, 2004 p.67).The Kirby Commission focused on wellnessrather than illness and reflects a FirstNations’ holistic perspective as well as apromotional approach to mental health.Mental health promotion focuses on buildingresiliency by supporting the development ofsocial skills, support from peers and family,a positive school climate and a sense ofbelonging (Wortzman, 2009).Yukon First Nation Mental Wellness Workbook
Effective mental health promotionemphasizes community-wide approaches,the tackling of root causes of mental healthissues, recognition of culture as a protectivefactor, and the integration of diverse formsof knowledge. At the same time however,mental health promotion programs areoften limited by not including spirituality andby emphasizing Western ways of thinkingabout health (Wortzman, 2009). 1While the AHTF project was unable topinpoint a definition of mental wellness,it did identify that a Yukon First Nationsapproach to mental wellness is holistic andseeks to integrate culture and spirituality inits approach.Research from across Canada showsthat trauma, racism and the alienation ofchildren from their families and communityis a part of the Indian Residential Schoolexperience.For many Yukon First Nations, the legacy ofcolonization continues and the impacts areboth real and present. The underlying mentalillness experienced by many First Nations isa normal human response to very abnormalconditions brought on by intergenerationalimpacts of colonization (Duu Chuu, 2010 p.6).At the AHTF Round Table on Health in May2009, Chris Lalonde, Associate Professorof Psychology at the University of Victoria,made links between cultural resiliency andthe health of a community, equating the lossof culture to the loss of wellness.At the AHTF Round Table on Health,discussions and presentations supportedthe links between Indian ResidentialSchool trauma, substance abuse andmental wellness.Colonization of lands and resourcessystematically removed the traditionalterritories of Yukon First Nations. The policyof assimilation furthered the burden on thehealth of First Nations people. This policyprovided the platform for the establishmentof residential schools and the forcedremoval of hundreds of children in theYukon. While these schools are now closed,the intergenerational impact continues infamilies, homes and communities across theterritory. 21,2 This information has been retrieved from Duu Chuu Management (March 2010). Mental Wellness Toolkit for Front Line Workers.Yukon First Nation Mental Wellness Workbook7
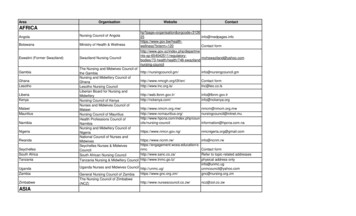
Infor mation behind the wor kbookThe report by the CCSA report makes linksbetween trauma and substance abuse. This isimportant as it put into the mainstream thelinks between the lived experience of FirstNations and the outcomes of that trauma.Information for this workbook draws fromfindings from the AHTF report MentalWellness Toolkit for Front Line Workers (DuuChuu, 2010). Input and direction was alsoreceived from the AHTF Mental WellnessAdvisory Group.“People and groups who experiencematerial deprivation, poverty, violence,rapid social change, diskriminationand other marginalizing conditionsare more vulnerable to mental illness”(World Health Organization, 2004). 3Information is based on a material scancompleted in the Mental Wellness Toolkit forFront Line Workers. A range of materials wasused including published and unpublisheddocuments.Yukon First Nations have been stating thatto address the mental wellness of theircitizens, services are required to address theco-occurrence of mental health, addictionsand trauma. Recent national publicationsnow support this thinking.To conduct a material scan for yourdepartment, the following list is provided asa starting point. Council of Yukon First Nations (CYFN) Yukon Government (YG) National Aboriginal Health Organization(NAHO) Assembly of First Nations (AFN) Aboriginal Healing Foundation (AHF) Health Canada (HC)Checkout thierwebsitesKey word searches also providedinformation for this report. To conduct keyword searches in your department, useweb browsers such as Google or InternetExplorer. For example, you can use anycombination of the following words to findresults on mental wellness:mental health sdroWinto ato putbox:searchmental health holistic wellnessmental health colonizationmental health Yukonmental health best practicesmental health community strategies3 Cited from http://www.naho.ca/firstnations/english/public mentalHealth.php8Yukon First Nation Mental Wellness Workbook
Section 1:Under standingMental HealthIssuesYukon First Nation Mental Wellness Workbook9
10Yukon First Nation Mental Wellness Workbook
Under standing Mental Health IssuesSection Objective: To identify key mental health issues of Yukon FirstNations to suppor t an action plan.“Fifty percent of those seeking help foraddictions also have a mental illness,and 15 to 20 percent of those seekinghelp from mental health servicesare also living with an addiction. “(CCSA 2009, p.9)In the report written by Duu ChuuManagement (2010), key mental healthissues were identified as well as underlyingcauses through two questions asked ofsurvey participants. The questions were: What are the key mental health issuesfor Yukon First Nations, their familiesand communities? What are the key underlying causes ofpoor mental health conditions amongstYukon Aboriginal people?Yukon First Nation Mental Wellness WorkbookThis section will explain each key issue,followed by a definition of the determinantsof health which mirror the underlyingcauses identified in the surveys.How to use this infor mationThe information on the following pagescan be used to support the developmentof a mental health strategic framework.Cut and paste this information into aproposal or work plan.The current medical approach to treatingmental health/wellness fails to addressmental health holistically, which in turnfails to address the root causes of mentalhealth, further compromising the wellness ofindividuals.11
TraumaThe surveys conducted by Duu ChuuManagement identified trauma as a commonmental health issue among Yukon FirstNation clients. Dr. Darien Thira, a wellknown British Columbia psychologist whohas worked with Aboriginal people andcommunities for many years, defines traumaas “the inability to release a painful experiencefrom one’s body, emotions, mind, and spirit sothat one lives each moment as if it were thattraumatic event” (Thira, 2009).Trauma can be experienced at both anindividual level and a collective level andresponses to traumatic events are notnecessarily the same (Bombay, Matheson,Anisman, 2009).The result of past and ongoing colonialpolicies and processes have impactedthe economic, political, cultural and socialfactors affecting the mental health statusof Yukon First Nations and in turn theirmental health status. Mental distressmay more accurately describe the mentalhealth conditions of First Nations. Mentaldistress is a normal human response toabnormal conditions. For First Nations, thoseconditions are brought on by dislocation andmarginalization from their own homelandand the impacts of residential school.The intergenerational trauma experiencedby Yukon First Nations is a collectiveresponse to the trauma that occurredthrough contact and colonialism.Through the survey work conducted byDuu Chuu Management (2010), a frequenttheme that emerged is the ongoing impactof residential schools on First Nationsindividuals, families and communities.The use/abuse of alcohol and other drugshave been a means of coping with the painas a result of trauma. Research shows a linkbetween stress, traumatic events and theuse of alcohol and drugs. Unfortunately, theuse of alcohol and drugs carries with it amultitude of issues itself, thus perpetuatingthe trauma to be visited on each newgeneration (Duu Chuu, 2010).Resources for dealing with trauma canbe found in Sections 5 and 6 and on thedisk supplied with this workbook.12Yukon First Nation Mental Wellness Workbook
Wor ds to describe and related to trauma include: past trauma suffer all kinds of abuse violence susceptible to predators anxiety undiagnosed mental conditionsrelated to trauma almost every day is crisismanagement abusive relationships lots of tragedies diagnosed with trauma without theservices self harming behaviours community and family violence grieving suicide victims of abuse become victims ofsystem family violence post traumatic stress disorder safety issues harassment and discrimination lots of trauma dealing with affects of trauma andgrief; stress and anxiety amongstchildren complex life of carrying posttraumatic stress, and coping throughalcohol and drugsYukon First Nation Mental Wellness Workbook most alcohol and drug clients arevictims of trauma13
Substance Use and AbuseDealing with addiction issues, especiallyalcohol and drugs, has been a long-standingpriority for Yukon First Nations. Alcoholand drug use are major challenges to thepromotion of good health and well beingamongst Yukon First Nation people.Wor ds to describe andrelated to substance abuseinclude: alcohol bingesSubstance use disorders co-occurring withmental health disorders represent a majorhealth problem in Canada (Duu Chuu, 2010).New work through the CCSA calls for theneed to provide more effective treatmentand approaches that recognize the linkbetween substance abuse and mentalwellness. As well, effective interventionrequires a better understanding of theunderlying mental health conditions and thepatterns of substance use (CCSA, 2009).Through the survey conducted by DuuChuu Management (2010), communitycare workers felt that clients were selfmedicating with the use of alcohol and drugsto address their mental distress. This copingstrategy perpetuates the cycle of substanceabuse and creates further stress leading totrauma, in turn, affecting mental wellness.14 addiction to prescription drugs new drugs coming into thecommunity drugs and drug overdoses drug-induced brain injury drugs on the increase ecstasy, crack, and easy access tomarijuana fetal alcohol spectrum disorder marijuana may be laced with harddrugs psychosis caused by drug useYukon First Nation Mental Wellness Workbook
Depression 1The Consensus Statement (October 17,2008), reported on the Mental HealthCommission website, describes depressionas being extremely common and worldwide.It has impacts that stretch to familymembers, co-workers and communities.Wor ds used to describeand related to depressioninclude: anxiety inability to “flourish” grievingSymptoms of depressioninclude feelings of: wanting change but don’t know howto change long-lasting sadness hopelessness anxiety helplessness grief related to chronic illnessdiagnosis emptiness worthlessness pessimism irritability guilt feelings of shame suicidal depression/anxiety Elders and isolation anger issuesPeople with depression may also experiencean inability to feel pleasure, a loss of interestin sex, a lack of energy and enthusiasm,disturbed sleep, changes in appetite and/orthoughts of suicide.Depression is a condition that varies inseverity. It may be mild, moderate, orsevere and it can happen once or can bereoccurring.More women than men experiencedepression. Depression often goes alongwith other medical illnesses. For somepeople, depression may be accompanied byharmful drug or alcohol use. 2 emotional distress people dealing with cancer – lotsof cancer, and dealing with chronicillnesses like diabetesThe mental health survey conducted byDuu Chuu Management revealed thatthe symptoms of depression amongstYukon First Nations people appear acrossall age groups from children sufferinganxiety, to youth and adults facing issuesof alcohol and drug abuse to reports ofElders feeling isolated and lonely.1 Information in this section is cited from Mental Wellness Toolkit for Front Line Workers, Duu Chuu Management 20102 Information cited from the Consensus Statement document found on line. port%20English%20(LR).pdfYukon First Nation Mental Wellness Workbook15
Concur rent Disorder sYukon First Nations Health and SocialDepartments have long spoken of theconnection between mental health andsubstance use. The December 2009Canadian Centre on Substance Abuse reportidentifies that the occurrence of thesetwo disorders – concurrent disorders - is asignificant health issue in Canada. It alsogoes on to state that individuals seekingtreatment for addictions often have a mentalillness (CCSA, 2010).Concurrent disorders occur when two ormore illnesses co-occur in the same person.Co-occurring substance abuse disordersand mental health conditions can becomeeven more complex when the person is alsoliving with Fetal Alcohol Spectrum Disorder(FASD) or another brain-based disability.The effect on family members and thecommunity is often significant.Many of the front line agencies in Yukonthat advocate for the needs of their clientsreport that mental health services do notco-treat the concurrent disorders butrather focus on either substance abuseservices or mental health services.16The CCSA reports the following on theissue of concurrent disorders (news releaseon Issues of Substance Abuse conference 2009): It is estimated that up to 50 percent ofthose with substance abuse issues willalso have a mental illness. Problems with impulse-control havebeen found to be the single strongestpredictor of future substance abuse. People with anxiety disorders are at atwo to five times greater risk of having aproblem with drugs or alcohol. Risk of substance abuse is at leastdouble for those with major depressivedisorders. Over 50 percent of adolescent patientsseen in psychiatric clinics use substances. People with schizophrenia are almostfive times more likely to have substanceabuse problems than people withoutmental disorders. The risk of schizophrenia in high usersof Cannabis (marijuana) is six timeshigher than in non-users.Yukon First Nation Mental Wellness Workbook
Fetal Alcohol Spectr um Disor der(FASD) 3Fetal Alcohol Spectrum Disorder (FASD)describes a range of disabilities that mayaffect people whose mothers drank alcoholwhile they were pregnant. FASD can affectseveral domains of brain function includingexecutive functions, memory, motor,sensory, language, social communicationand adaptation that manifest themselvesas learning and/or behavioral difficultiesthroughout the childhood and adult life ofa person with FASD (Chutley et al, 2005).This impact on brain function can affect theway a person is able to cope with home life,friends, school and community.Streissguth et al (1996) described thesecondary disabilities associated with FASDin their groundbreaking study of 1996. Themost common secondary disabilities weremental health conditions (Streissguth et al,1996). These resulted in disrupted schoolexperiences, trouble with the law, andconfinement in prison as an inpatient inmental health facilities or as an inpatient inan alcohol and drug treatment program.Streissguth et al also identifiedenvironmental protective factors thatinclude a stable nurturing home, consistencyin the household, not being a victim ofviolence, access to development disabilitiesservices and having a diagnosis before sixyears of age.Protective Factors Living in a nurturing home Having consistency in the household Not being a victim of violence Having access to developmentdisabilities services Being diagnosed before six years ofageSecondary conditions also manifest asinappropriate sexual behaviour and alcoholand drug problems. The urgency of earlyinterventions and treatment services isfurther supported in the recent researchshowing mental health as both a primaryand secondary disability of FASD (Astley,2009; Weinberg, 2009).3 This section is cited from Mental Wellness Toolkit for Front Line Workers, Duu Chuu Management 2010Yukon First Nation Mental Wellness Workbook17
Psychiatric conditions found mostfrequently in children with FASDinclude: Attention Deficit HyperactiveDisorder (ADHD) Conduct Disorder Oppositional Defiant Disorder depressive disorders anxiety disorders panic disorders increased suicide rates specific phobias substance abuse disordersConditions that occur less frequentlyinclude schizophrenia, autism and bipolardisorder (Freyer et al, 2007; O’Connor, 2006;Nash et al, 2006). Mental health disordersarise from complex interactions of factorsincluding biological, genetic, socio-economic,environmental, and psychological factors(Mental Health Commission, 2009). Thesefactors interact with the underlyingneurodevelopment deficits of individualswith FASD to create a complex comorbidity of disability and mental healthconditions.The enormity of FASD and mental healthconditions often results in overlooking thewhole child who has strengths and gifts aswell as challenges. Focusing on the negativecan contribute to increased feelings of lowself-esteem and isolation.The following is a positive list of FASDbehaviors, as seen from a nurturing familyperspective: willingness and wanting to please easily letting go of hard feelings towardssomeone ability to pay attention when distractionsare removed and environments areproperly structured ability to focus better at certain times ofthe day or under certain conditions suchas being fed or after exercise (whichmeans that attention problems maycome and go) often excelling in the kinds of hands-onor kinesthetic learning that takes placein traditional communal activities andwhere communication is less based onlanguage (Warner, K, White Crow Villagepersonal communication, March 2009).Further information on FASD can be found atthe website: http://www.phac-aspc.gc.ca/fasdetcaf/faq-eng.php or call FASSY at 867-393-4948for local support and resources.18Yukon First Nation Mental Wellness Workbook
Children’s Mental HealthIn the survey conducted by Duu ChuuManagement in 2009, Whitehorse agencyworkers reported mental health issuesspecific to Yukon First Nation children (fiveyears and under) included: anxiety attachment disorders behavioral problems complex problems attention difficulties.Yukon First Nation front line workersreported the following issues for childrenand youth (all ages): FASD unresolved childhood traumaThe importance of health and developmentin this age group has also been recognizedin the wisdom of Elders. First Nation Elderstalk of how families and communitiestraditionally came together to meet theneeds of their children. Each member ofthe family has a role to play in raising thechildren. Within the community, the rolesand responsibilities of family membersextend to all the children in the community.Elders teach that “it takes a community toraise a child.”Scientific research has also made clearsthis saying, stating that children needgood nutrition, nurturing and a safe andconsistent environment, sleep, daily routine,stimulation and play for the development ofa healthy brain and the foundation for goodmental wellness. child mental health conditions “lost” children who wander aroundafter school appearing that they don’twant to go home; emotionally lostThese findings are significant in showingthat many First Nation young childrenare stressed from living very complicatedlives. The need for early intervention isdemonstrated in the report Out of theShadows (Kirby & Keon, 2006) whichrecognized that most mental healthdisorders amongst adults began inchildhood. Unfortunately, services are oftenfragmented and underfunded.Yukon First Nation Mental Wellness Workbook19
Under lying Causes and the Deter minants of HealthA mental health and wellness approach recognizes that many social and health factors(determinants) contribute to a person’s mental health and that issues like violence or addictionscannot be separated and seen as distinct or be dealt with in isolation. In a mental wellness approachthey are seen as symptoms. Determinants of health (e.g. housing, social s
Yukon First Nation Mental Wellness Workbook 5 How to use this workbook Section 1 describes the underlying causes of mental illness and their relationship to the determinants of health. Use this section as a teaching tool or in discussion about Yukon First Nation mental wellness issues. Cut a