Transcription
Brigham ComprehensiveOpioid Response andEducation (B-CORE)Program2020 Report
Table of ContentsIntroduction to the Program page 2Director’s Message .page 4Opioid Prescribing at Brigham Health . page 5Bridge to Recovery Clinic . page 7Interaction with Partners (Mass General Brigham) . . page 8Program in Opioid and Pain Innovation (POPI) .page 12Recovery Month page 13Discover Brigham . page 15Boston/Cambridge Opioid Consortium page 16The HRT Pathway for Cardiac Surgery Patients . page 17Pharmacy Interventions . page 19The Brigham Inpatient Opioid Stewardship Initiative (BIOSI) .page 20Philanthropy . . page 21Research Excellence . page 23Looking to the Future . page 24Cover image copyright by Dr. Hanni Stoklosa, executive director of HEAL Trafficking, aninterdisciplinary group of professionals leading the public health response to human trafficking.Photographs are available for sale with all proceeds supporting the initiative sa.html
The Brigham Comprehensive OpioidResponse and Education (B-CORE)ProgramMission Statement: Develop a comprehensive program that measurably demonstratesimplementation of Brigham-wide guidelines for opioid prevention, opioid prescribing, managingchronic pain, and managing opioid addiction through technology, data, outreach, clinical support, andtraining.Leadership:Executive CommitteeKey StakeholdersSalah Alrakawi, BWH Primary CareGloria Brand, Program Director, Program in Opioidand Pain InnovationKathryn Britton, BWH Associate CMOJames Bryant, BWH ComplianceDarin Correll, BWH AnesthesiologySonali Desai, BWH Medical Director of AmbulatoryPatient SafetyMatthew Fishman, Partners VP Community HealthMichael Hession, Harbor Medical Associates CMOHenrietta Menco, Partners Employee AssistanceProgramLisa Morrissey, BWH Associate CNOChristine Murphy, BWH Psychiatric NursingResource ServiceRajesh Patel, BWH CMIOClaudia Rodriguez, BWFH Addiction Faulkner BCORE DirectorAndrew Seger, BWH PharmacyRushdia Yusuf, DFCIScott Weiner, DirectorShelly Anderson, BH Chief Strategy OfficerCraig Bunnell, DFCI CMOJohn Co, Partners GMEPeggy Duggan, BWFH CMOSunny Eappen, BWH CMOJohn Fanikos, BWH PharmacyChris Gilligan, BWH Pain MedicineRichard Gitomer, Director, BWH Primary CareMichael Healey, BWPO eCare Ambulatory CMIOJessica Logsdon, BWH PA DirectorWanda McClain, BWH VP Community HealthMaddy Pearson, BWH CNOJames Rathmell, Chair BWH AnesthesiaAndrew Resnick, BWH CQODavid Silbersweig, Chair BWH PsychiatryJoji Suzuki, Director, BWH Addiction Psychiatry2
Goals 2018-2019:Established Substance Use Disorder Bridge ClinicContinued decline in overall opioid prescriptionsMet internal performance framework (IPF) metric for opioid educationReleased opioid toolkit for providers and opioid education sheet for patientsCompleted PDMP integration with Epic and implemented comprehensive opioidrelated clinical decision support releasedGoals 2019-2020:Focus on high morphine milligram equivalent opioid prescriptions, with a goal ofreducing prescriptions for 90 morphine milligram equivalents by 20% (7/18-6/19compared with 7/19-6/20)Establish resources for clinicians managing patients with high dose opioidsIncrease documented naloxone co-prescriptions for primary care patients on 90 MMEfrom 1% to 5%Conduct quarterly case conference “pain board”Launch Program in Opioid and Pain Innovation (POPI) initiativeSponsor awards, such as the Pain and Opioid Shark Tank, in collaboration with theBrigham Research InstituteLaunch cardiac surgery/IV drug use-related infection clinical pathwayLaunch Partners-wide opioid metrics dashboardMeet Boston/Cambridge Consortium commitments3
Director’s MessageScott G. Weiner, MD, MPHAs I write this, we’re in the midst of the COVID pandemic. It is an all-hands-on-deckmoment in which we are working together towards a common goal of helping eachother be safe. The scariest part about the COVID epidemic is its rapidity – but that isalso what sparked society to ask so quickly.The opioid epidemic, which has claimed hundredsof thousands of lives in our country over the pastdecade, is more like the fable of the frog in hotwater: a frog put suddenly into boiling water willjump out, but a frog put in tepid water which isthen slowly brought to a boil will not perceive thedanger and will be cooked to death. What wouldthe opioid epidemic have looked like if we had aparallel response ten years ago, when the opioid epidemic was first recognized?It’s a battle, and one that Governor Charlie Baker said necessitates us to be“relentless.” I am proud that we have stepped up at Brigham Health. In fact, it’s takenyears, but we have finally appeared to “flatten the curve” of the opioid epidemic inMassachusetts.Herein you will learn about incredible progress made over the past four years as westrive to deliver the best care possible to our patients in pain or struggling withaddiction.4
Opioid Prescribing at Brigham HealthAfter an initial decline upon the start ofB-CORE, opioid prescribing at BrighamHealth has stabilized. We prescribearound 8,000 opioid prescriptions permonth to our patients, which is downsignificantly from the start of ourprogram in 2016. Some opioidprescribing, such as after acute surgeryor trauma, is a part of standard practice.The most common opioids prescribed atBrigham Health (Jan, 2019 to Mar, 2020)are oxycodone, tramadol andhydromorphone.We are, however, cognizant of significantly increased risks associated with chronicopioid use for noncancer pain. As medical knowledge advances, our practice atBrigham Health constantly evolves. For over a decade, opioid pain medications wereconsidered to be a primary treatment modality for patients with chronic, non-cancerpain. With advancing knowledge, we now know that chronic opioid therapy isassociated with minimal benefits to function, and markedly increases a person’s risk ofoverdose and death.The 2016 Centers for Disease Control and Prevention Guideline for Prescribing Opioidsfor Chronic Pain states that providers “should avoid increasing dosage to 90 morphinemilligram equivalents (MMEs) or more per day or carefully justify a decision to titratedosage to 90 MME or more per day.” Understanding that this guideline was releasedafter many patients with chronic pain were already on doses greater than 905
MME/day, we aim to transition those patients currently taking 90 MME/day to saferdoses in a compassionate and careful way. Our recommendation is to decrease dosesgreater than 90 MME/day by 10% per month until the patient is below the 90 MEE/daydose or lower if the patient continues to tolerate the wean. This advice is based on thedata confirming the limited efficacy of doses greater than 90 MME/day along with the10-fold increase of diversion or overdose in patients with non-cancer pain.Historically, there have been around 1,100 highdose opioid prescriptions per month, but thatnumber is now decreasing. We have committed towork with prescribers who frequently prescribehigh-dose opioids to achieve this goal. Amultidisciplinary and multispecialty group reviewscases for high-frequency prescribers and providestapering guidance. We recognize that there maybe patients who are unable to taper below 90MME, but we expect this to be an infrequent exception.For all patients on chronic opioids, we encourage all of our prescribers to commit toensuring safe practices including a) review of MassPAT prior to every prescription, b)avoidance of opioids and benzodiazepines in combination, c) an active medicationmanagement agreement, d) random toxicology screening at least once per year and e)co-prescription of naloxone.6
Bridge to Recovery ClinicThe Brigham Health Bridge to Recovery clinic is a centerpiece of our response to thesubstance use disorder epidemic. This low barrier to access program has served over500 patients since its inception in April, 2018. Theclinic is designed to provide rapid access toinpatients, emergency department patients andoutpatients in the crucial stage of care betweenactively using drugs or alcohol and a connection to along-term care program, such as Faulkner’sAddiction Recovery Program.The clinic is staffed by addiction medicine/psychiatryphysicians, primary care physicians, infectiousdisease specialist, nurse practitioner, clinical resource specialist, and peer recoverycoaches, all working towards embracing patients, “meeting them where they are at”,and stewarding them towards their recovery. The clinic now offers evening hours,peer-led recovery groups, as well as the ability to provide all injectable medicationssuch as Sublocade and Vivitrol.During the past year, the Bridge Clinic worked closely with the inpatientmedical/nursing teams to pilot a program to offer outpatient parenteral antimicrobialtherapy (OPAT) to patients who require long-term antibiotic treatment for seriousbacterial infections. All pilot patients successfully completed their antibiotic treatment,and as a result avoiding hundreds of inpatient/rehab days.7
Interaction with Partners (Mass GeneralBrigham)Interaction with the overall health system is essential as we can learn from ourcolleagues at our affiliated hospitals and work together to create clinical guidance,clinical decision support tools and system-wide metrics. The B-CORE director is the cochair of the Partners Substance Use Disorder Steering Committee.As an example of clinical guidance, we havecreated a buprenorphine start guide for patientspresenting to any of the hospital emergencydepartments in the system. Research hasdemonstrated that starting buprenorphine (alsocalled Suboxone) to patients who present to theemergency department with opioid withdrawalare much more likely to be retained intreatment if the medication is startedimmediately. This involves not only a protocol,but also special training. Nearly all of theemergency physicians at Brigham Health havecompleted this training.We have created a guidance forproviders who are attemptingto taper patients with chronicnon-cancer pain to safer opioiddoses. The guideline is specificabout how to do this safely andcompassionately.8
A significant project is being undertaken to create a system-wide opioid metricsplatform. The first iteration was recently released and allows quality directors theability to easily analyze and compare the opioid prescriptions of their providers. Thefirst modules are for ambulatory care clinics, the emergency department, and aftersurgery.This report allows us to compare thepercentage of patients prescribedopioids at the hospital, clinic andindividual provider level.This report allows us to determine thenumber of pills prescribed to patientsafter the same surgical procedure. Ifthere are outlier prescribers, we workwith their department leadership toensure they are concordant withguidelines and their peers.This report allows us to compare opioidprescribing patterns by emergencyphysicians.9
Since the system uses one single Electronic Health Record, working with Partners hasallowed us to introduce innovative clinical decision support tools for our providers.We have created a standardized menu of“pain treatment agreements” for patientstaking chronic opioids. The agreementshave a special symbol at the top, so whenscanned into the computer, the systemknows if it exists. If not present, it willremind the provider to have the patientsign a document. This improves ourcompliance with a state law mandatingthese agreements.We were the first system in Massachusetts to integrate our state’s prescription drugmonitoring program (MassPAT) into our electronic health record. This integrationallows providers to do a single mouse click to access the data, which used to be acumbersome process.10
Other tools remind clinicians about safe prescribing practices, such as to checkMassPAT before writing a prescription, to perform a toxicology test at least once ayear, to have a clinic visit at least everyfour months, and to avoid prescribingmore than 7 days of opioids to an opioidnaïve patient. Other tools remindproviders to co-prescribe naloxone topatients on high dose opioids, foremergency department providers to referpatients to our Bridge Clinic, and forobstetricians to remind women whodelivered to dispose of any prescribedopioids at the time of their follow-up visit.Also, we adopted electronic prescribing of controlled substances. Now, all prescriberscan send opioid prescriptions electronically to a patient’s pharmacy of choice insteadof relying on paper prescriptions. This action allows refills to be sent without a patientneeding to come to the clinic and may also reduce falsified prescriptions and diversion.We have introduced several “dot phrases” which help clinicians accurately documentopioid related care.We have also created several guides for patients ranging from safe use of opioids(automatically provided if an opioid is provided) to harm reduction techniques forpeople who inject drugs.11
POPI: Program in Opioid and PainInnovationEven with all of the work done clinically, we know that at Brigham Health we areuniquely positioned to take a strategic systems approach to the opioid and painproblem and drive change in how we treat acute pain and chronic pain, use opioids,and treat addiction. We wish to apply Brigham’s brainpower, clinical expertise,technology resources and research capabilities to create transformative solutions tothe opioid epidemic.To this end, we have created the BrighamProgram in Opioid and Pain Innovation (POPI)Program. The goal is to break down the silostraditionally found in research and encouragecross-departmental collaboration andinnovation in the pain and opioid space. Weare delighted that Gloria Brand, seniorprogram manager, has joined us to organizethis nascent initiative.12
Recovery MonthWe are honored to celebrate NationalRecovery Month each September. Thisevent, sponsored by the SubstanceAbuse and Mental Health ServicesAdministration (SAMHSA), increasesawareness and understanding of mental and substance use disorders and celebratesthose in recovery.In 2019, we held a grand rounds panel discussinginnovative solutions to the opioid epidemic,including Safe Injection Facilities and dischargingpatients who need long-term antibiotics with IV linesonce they are stable on medication to also treat theiropioid use disorder.We host the project Resilient: Narratives of Hopefrom Boston’s Opioid Crisis, a photojournalismproject spearheaded by Harvard Medical Schoolstudents to increase knowledge around stigmaand recovery.We host informational booths to inform patients andproviders about recovery resources available to them,and to teach use of naloxone, the opioid overdoseantidote.13
We have hosted movie nights, bringing patients who shared stories of their ownrecovery and then screened the films relating to recovery.Most importantly, we recognize that stigma is the frequently the largest barrierpatients have to getting help for their addiction. We have created an anti-stigmapledge for all hospital staff to sign and keep.14
Discover BrighamIn the annual Discover Brigham program, in which community members are invited tolearn about innovations in the hospital, B-CORE has been delighted to present themultiple times. In 2018, we highlighted our “No Wrong Door” approach, which meansthat anywhere a patient presents to the Brigham, we will find a way to help addresstheir opioid use disorder. In 2019, we highlighted interventions in infectious disease forpatients with opioid use disorder and work being done in our nursery for babies withneonatal opioid withdrawal syndrome.15
Boston/Cambridge Opioid ConsortiumIn 2019, Brigham Health joined a consortium of hospitals in Boston and Cambridgewith the goal ofresolving the opioidepidemic on a city-widescale. The initiative,spearheaded by Dr.Betsy Nabel and KateWalsh (from BostonMedical Center, hascommitted to severalspecific steps:Brigham Health is wellrepresented in thisconsortium, and wecontributed to both thecontent of this commitment and the steps to meet it.We also conducted an opioid grand roundssession, led by Dr. Claudia Rodriguez,covering the mandatory training. We aremaking this training available online to allproviders on the HealthStream platform.16
The HRT Pathway: Improving Care forCardiac Surgery Patients with OpioidUse DisorderHistorically, one of our most challenging patient populations have been those who aresuffering from cardiac complications of injection drug use and require cardiac surgery,such as heart valve replacement. Imagine the scenario: a patient who is actively usingdrugs comes into the hospital, has an acutely painful procedure and then must be onIV antibiotics,sometimes for 6weeks or longer.Withoutaddressing theunderlyingaddiction, relapseis an expectedoutcome.At Brigham Health, we wish to change this paradigm. Treating an infected heart valvewithout addressing the underlying substance use disorder that led to the infection isakin to treating complications of diabetes but not actually providing insulin.Several key stakeholders, including those in the Divisionof Cardiac Surgery, Cardiac ICU and Intermediate CareNursing and the BWH Psychiatric Nursing ResourceService have joined forces to create a new pathway – TheHeart Recovery Treatment (HRT) pathway – to improvecare by standardizing the approach we take to patientswith opioid use disorder, and working to decrease stigmaamongst our staff.17
A key component of the initiative is the intensive training of all staff who care for thesepatients on the cardiac unit. The BWH Psychiatric Nursing Resource Service hasorganized interprofessional education and simulation training program at our STRATUSsimulation center to allow role-playing and practice new techniques.The program builds on successes we have hadwith starting patients with injection drug userelated infections on medication for opioid usedisorder (like buprenorphine) in the hospital andallowing them to go home with a long-term IV linefor their antibiotics. In the past, providers wouldnot trust patients to go home with these lines forfear that they would inject drugs in them.However, we have discovered that patients whoengage in treatment in our clinic and take amedication for their addiction (likebuprenorphine) do very well. For our first 20 patients, we estimate saving over 500days of inpatient or rehab stays by starting this program, which has been featured innational media.18
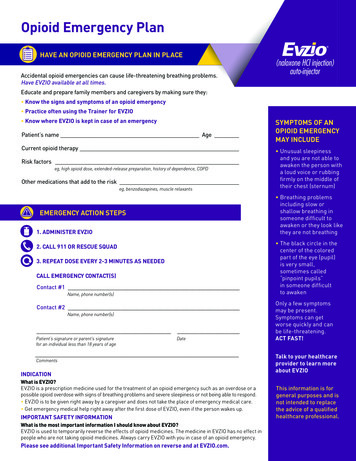
Pharmacy InterventionsThe Brigham and Women’s Pharmacy is deeplycommitted to improving opioid-related care. As part ofnational drug take-back day, we routinely host tableswhere staff and patients can discard unused or expiredmedications.Patients and staff can also drop off thesemedications at any time at a bin in ourpharmacies at Brigham and Women’sHospital and at the 850 Boylston Streetlocation.Pharmacists and pharmacy fellows are working closely with clinics that provide highdose opioid prescriptions in order to ensure that safe practices are being followed andto assist in tapering down patients to safer doses when appropriate.The pharmacy also stocks Narcan (naloxone),the opioid overdose antidote. This can bepurchased by any individual without aprescription. For hospital employees who usetheir insurance, there is no co-pay. Thepharmacies at Brigham and Women’s Hospitaland Brigham and Women’s Faulkner Hospitalalso distribute this life-saving medication toindividuals at high risk in both of ouremergency departments. Of note, our policeand security force also carry Narcan so that they can quickly reverse overdose victimsd
Program Lisa Morrissey, BWH Associate CNO Christine Murphy, BWH Psychiatric Nursing Resource Service Rajesh Patel, BWH CMIO Claudia Rodriguez, BWFH Addiction Faulkner B-COR