Transcription
Delivering Dementia Capable Care WithinHealth Plans: Why And How?Credit Information§ If you are a social worker in a National Association of Social Workers(NASW) state and would like to receive CE credits through NASW for this eventor a nurse looking to obtain CNE credits through the California Board ofRegistered Nursing, please complete the pre-test posted here:https://www.surveymonkey.com/r/dementia1 PreTest§Youwill also be required to complete a post-test; a link to this test will appear at the end of thepresentation.§Please note: Live CME and CE credits through CMS may not be available forthis live event. Please check the RIC website in a few weeks’ time to determineenduring credit availability.Audio and Platform Information§The audio portion of the presentation will automatically stream through yourcomputer speakers. If you experience challenges with the audio, please click thephone icon at the bottom of the screen for dial-in information.§If you are experiencing any technical difficulties with this platform, please use theQ&A feature for assistance or click the help button for additional e.com
June 19, 2019Delivering Dementia Capable Care WithinHealth Plans: Why And How?https://www.ResourcesForIntegratedCare.com
Overview§ This session will be interactive (e.g., polls and interactivechat functions), with 60 minutes of presenter-led discussion,followed by 30 minutes of presenter and participantdiscussions.§ Video replay and slide presentation are available after eachsession at: //www.ResourcesForIntegratedCare.com
Accreditation§ Individuals are strongly encouraged to check with their specificregulatory boards or other agencies to confirm that courses takenfrom these accrediting bodies will be accepted by that entity.§ The American Geriatrics Society has been approved by the CaliforniaBoard of Registered Nursing to provide continuing education.§ The American Geriatrics Society is accredited by the NationalAssociation of Social Workers (NASW) to provide continuing educationfor social m
Disclosure StatementAs an accredited provider of Continuing Medical Education, the American Geriatrics Society continuously strives to ensure tha tthe education activities planned and conducted by our faculty meet generally accepted ethical standards as codified by theACCME, the Food and Drug Administration, and the American Medical Association's Guide for Gifts to Physicians. To this end,we have implemented a process wherein everyone who is in a position to control the content of an education activity hasdisclosed to us all relevant financial relationships with any commercial interests as related to the content of their present ationsand under which we work to resolve any real or apparent conflicts of interest. The existence of commercial or financial inter estsof speakers related to the subject matter of their presentations should not be construed as implying bias or decreasing thevalue of their presentations. However, disclosure should help participants form their own judgments. Those speakers whodisclosed affiliations or financial interests with commercial interests involved with the products or services to which they mayrefer are listed below. We have also noted if a speaker has indicated that s/he will be discussing a commercial product or anoff-label or investigational use.The following planners/faculty have returned disclosure forms indicating that they (and/or their spouses/partners)have no affiliation with, or financial interest in, any commercial interest that may have direct interest in the subjectmatter of their presentation(s):4§Gregg Warshaw, MDNo relevant financial interests or affiliations§Nancy Wilson, MA, MSWNo relevant financial interests or affiliations§Christopher Callahan, MD, MACPNo relevant financial interests or affiliations§Megan Dankmyer, MSGNo relevant financial interests or affiliations§Katie Scott, MPHNo relevant financial interests or affiliations Debra Cherry, PhDNo relevant financial interests or .com
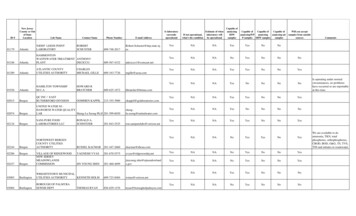
Continuing Education InformationIf You Are A:Credit OptionsRequirementsAmerican Geriatrics SocietyPlease note: other health care professionals can receive certificate of participation from AGSThe American Geriatrics Society designates this webinar for amaximum of 1 Continuing Education (CE) credit hour throughNASW1. Complete the pre-test at thebeginning of the webinarSocial WorkerPlease note: New York, Michigan, and West Virginia do not accept 2. Complete the post-test with aNational CE Approval Programs for Social Work. New Jersey,score of 80% or higherIdaho, and Oregon do not recognize NASW National ApprovalNurse5The American Geriatrics Society designates this program eligiblefor 1 nursing contact hour through the California Board ofRegistered Nursing1. Complete the pre-test at thebeginning of the webinar2. Complete the post-test with ascore of 70% or higherhttps://www.ResourcesForIntegratedCare.com
Support Statement§ This webinar is supported through the Medicare -Medicaid CoordinationOffice (MMCO) in the Centers for Medicare & Medicaid Services (CMS)to help beneficiaries dually eligible for Medicare and Medicaid haveaccess to seamless, high-quality health care that includes the full rangeof covered services in both programs. To support providers in their effortsto deliver more integrated, coordinated care to dually eligiblebeneficiaries, MMCO is developing technical assistance and actionabletools based on successful innovations and care models, such as thiswebinar.§ To learn more about current efforts and resources, visit Resources forIntegrated Care at: //www.ResourcesForIntegratedCare.com
Introductions§ Christopher M. Callahan, MD, MACPChief Research and Development Officer, Eskenazi HealthProfessor, Indiana University School of MedicineScientist, Indiana University Center for Aging ResearchResearch Scientist, Regenstrief Institute, Inc.§ Debra Cherry, PhDExecutive Vice President, Alzheimer’s Los Angeles§ Megan Dankmyer, MSGAssociate Vice President of Case Management, Molina California§ Katie Scott, MPHSr. Director of Dementia and Caregiver Support Services, BakerRipleySenior Services m
Learning Objectives1. Recognize how cognitive impairment and dementia impactthe well-being of older adults and family caregivers2. Identify opportunities to reduce the high health care andsocietal costs of dementia3. Recognize key features of dementia capable healthsystems and quality dementia care coordination4. Identify key approaches for health plan collaboration withpatients, family caregivers, and community re.com
Webinar Outline/Agenda§ Poll Questions§ Dementia Capable Care Overview§ Strategies and Tools to Improve Dementia Care in theFinancial Alignment Initiative§ Implementing the Texas Takes on Dementia Program§ Q&A§ com
Dementia Capable CareChristopher M. Callahan, MD, MACPChief Research and Development Officer, EskenaziHealth Professor, Indiana University School of MedicineScientist, Indiana University Center for Aging ResearchResearch Scientist, Regenstrief Institute, Inc.10https://www.ResourcesForIntegratedCare.com
Millions of People Will DevelopAlzheimer’s Disease§ The number of people aged 65 and older in the U.S. with Alzheimer’sdisease (AD), the most common type of dementia, is projected to risedramatically1. Alzheimer’s Association. (2019). Alzheimer’s Disease Facts and Figures. Retrieved from: rIntegratedCare.com
We Have No Disease-ModifyingTreatments for Dementia§ There are no known medications toprevent, cure, delay the onset, or slowthe progression of AD and otherdementias1§ Since 2000, more than 100 AD drugsfailed in clinical trials2,31. Alzheimer’s Association, 20192. Sloane, P. D., Zimmerman, S., & Boustani, M. (2018). The Unmet Promise of a Miracle Drug for Alzheimer's Disease: Implications for Practice, Policy, and Research.3. E Becker, R., & H Greig, N. (2010). Why so few drugs for Alzheimer's disease? Are methods failing drugs?. Current Alzheimer Research, 7(7), om
People Often Live with Dementia for10 YearsMini-Mental State Exam Score4. Larson, E. B., Shadlen, M. F., Wang, L., McCormick, W. C., Bowen, J. D., Teri, L., & Kukull, W. A. (2004). Survival after initial diagnosis of Alzheimer disease. Annals of internal medicine, dCare.com
Dementia is Among the CostliestConditions in the U.S.§ In 2019, Medicare and Medicaid will spend an estimated 195billion caring for those with Alzheimer’s and other dementias—67percent of total costs5§ 27% of people with dementia who are receiving Medicare benefitsare dually eligible for Medicaid1§§§Home- and community-based services represent 57% of Medicaidspending on long-term services and supports while institutional carerepresents 43%150% of nursing home residents have AD or other dementias 1Medicaid costs associated with AD were 70% higher for women thanmen1§ Comorbid conditions associated with dementia (such as falls, hipfracture and replacement, and urinary tract infection) are thestrongest drivers of health care costs6,71. Alzheimer’s Association, 20195. Alzheimer’s Association. (2019). Cost of Alzheimer’s to Medicare and Medicaid. Retrieved from: http://act.alz.org/site/DocServer/2012 Costs Fact Sheet version 2.pdf?docID 71616. Alzheimer’s Research UK (2019). Comorbidities. Retrieved from: rbidities/7. Zhu, C. W., Cosentino, S., Ornstein, K. A., Gu, Y., Andrews, H., & Stern, Y. (2017). Interactive effects of dementia severity and comorbidities on Medicare expenditures.Journal of Alzheimer's Disease, 57(1), om
Dementia Pushes Some Familiesinto Poverty§ Medicare expenditures for dementia are similar toother chronic conditions, but out-of-pocket costsare 81% higher5§Costs such as assistance with dressing andpersonal hygiene may not be covered§ Out-of-pocket medical expenses relative to totalhousehold wealth are much higher for dementiathan other conditions§ Family spending on dementia reduces amountavailable for intergenerational wealth transfer58. Kelley, A. S., McGarry, K., Gorges, R., & Skinner, J. S. (2015). The burden of health care costs for patients with dementia in the last 5 years of life.Annals of internal medicine, 163(10), om
Medical Care for DementiaSometimes Falls Short§ Most persons with dementia are cared for in primary care settings,but the typical primary care physician (PCP) cares for only 25older adults living with dementia9-11§ Less than 50% receive recommended evaluation for dementiadiagnosis1§ Less than 50% of Medicare beneficiaries with a diagnosis ofdementia are told they have the diagnosis1§ More than 20% are prescribed inappropriate medications,including anticholinergic medications that are linked to worseningof dementia symptoms11§ Half of caregivers of people with dementia indicate no experienceperforming nursing-related tasks and information for managingcomplex medication regimens19. Callahan, C. M., Hendrie, H. C., & Tierney, W. M. (1995). Documentation and evaluation of cognitive impairment in elderly primary care patients. Annals of internal medicine, 122(6), 422-429.10. Boustani, M., Callahan, C. M., Unverzagt, F. W., Austrom, M. G., Perkins, A. J., Fultz, B. A., Hendrie, H. C. (2005). Implementing a screening and diagnosis program for dementia inprimary care. Journal of general internal medicine, 20(7), 572–577. doi:10.1111/j.1525-1497.2005.0126.x11. Boustani, M., Sachs, G., & Callahan, C. M. (2007). Can primary care meet the biopsychosocial needs of older adults with dementia? Journal of general internal medicine, 22(11), 1625–1627.1. Alzheimer’s Association, 201916https://www.ResourcesForIntegratedCare.com
Patients with Dementia HaveFrequent Transitions12. Callahan, C. M., Arling, G., Tu, W., Rosenman, M. B., Counsell, S. R., Stump, T. E., & Hendrie, H. C. (2012). Transitions in care for older adults with and without dementia. Journal ofthe American Geriatrics Society, 60(5), 813-820.13. Callahan, C. M., Tu, W., Unroe, K. T., LaMantia, M. A., Stump, T. E., & Clark, D. O. (2015). Transitions in care in a nationally representative sample of older Americans withdementia. Journal of the American Geriatrics Society, 63(8), 1495-1502.14. Unroe, K. T., Carnahan, J. L., Hickman, S. E., Sachs, G. A., Hass, Z., & Arling, G. (2018). The complexity of determining whether a nursing home transfer is avoidable at time oftransfer. Journal of the American Geriatrics Society, 66(5), om
Unpaid Family Caregivers ofIndividuals with Dementia§ Persons living with dementia often adaptto provide their own care for years§ Family caregivers provide 80% of totalcare to persons with dementia§ Most persons with dementia havemultiple caregivers§ Most caregivers are women§ All medical and social models of care relyon family caregivers, high risk of burnout§ In 2018, 18.5 billion hours of care, valuedat 234 billion, were provided by familyand unpaid caregivers1. Alzheimer’s Association, 201918https://www.ResourcesForIntegratedCare.com
Systems of Dementia Care Need toAddress Multiple Issues§ Integrated dementia care models attempt to address therange of medical and non-medical issues related todementia care.§§§19Support for caregivers (e.g., including improved education andaccess to different resources)Quality of medical care (avoiding inappropriate prescriptions,improving PCP education regarding persons with dementia)Coordination of care (across different providers and settings ofcare, working with community om
Research On Redesigning Systemsof Dementia Care15. de Waal, H., Lyketsos, C., Ames, D., & O'Brien, J. (Eds.). (2013). Designing and delivering dementia services. Hoboken, NJ: John Wiley & Sons.20https://www.ResourcesForIntegratedCare.com
Medical Components of IntegratedDementia Care Models§§§§§§Identify individuals at risk of AD and diagnose earlyEvaluate for treatable conditionsEvaluate for reversible causes of dementiaDiscuss diagnosis and prognosisContinue care for comorbid conditionsTreat behavioral symptomsExample ModelsCollaborative Care for DementiaPartners in Dementia CareMIND at HomeUCLA Alzheimer and Dementia Care Program16. Callahan, C. M., Boustani, M. A., Unverzagt, F. W., Austrom, M. G., Damush, T. M., Perkins, A. J., . & Hendrie, H. C. (2006). Effectiveness of collaborative care for older adults withAlzheimer disease in primary care: a randomized controlled trial. Jama, 295(18), 2148-2157.17. Bass, D. M., Judge, K. S., Lynn Snow, A., Wilson, N. L., Morgan, R., Looman, W. J., . & Garcia‐Maldonado, M. (2013). Caregiver outcomes of partners in dementia care: Effect of acare coordination program for veterans with dementia and their family members and friends. Journal of the American Geriatrics Society, 61(8), 1377-1386.18. Jennings, L.A., Laffan, A.M., Schlissel, A.C., Colligan, E., Tan, Z, Wenger, N.S., Reuben, D.B. (2019). Health Care Utilization and Cost Outcomes of a Comprehensive DementiaCare Program for Medicare Beneficiaries. JAMA, 179(2), om
Social Components of IntegratedDementia Care Models§ Engage community support agenciesfor individualized and culturally competentservices§ Use an individualized care plan to focus ongoals, needs, and maximizingindependence§ Discuss advance care planning§ Facilitate physical and social activityExample ModelsResources forEnhancingAlzheimer'sCaregiver Health(REACH)Skills2CareSAVVY CaregiverSHARE forDementia19. Gitlin, L. N., & Hodgson, N. A. (2018). Better Living with Dementia: Implications for Individuals, Families, Communities, and Societies. Academic Press.22https://www.ResourcesForIntegratedCare.com
Social Components of IntegratedDementia Care Models (continued)§ Provide guidance on risks of financial fraud(e.g., telephone scams), wandering, driving,and preparation for emergencies§ Consider home modifications that supportindependence and increase comfort§ Provide culturally sensitive emotionalsupport to caregivers, and track theirwell-being and outcomesExample ModelsResources forEnhancingAlzheimer'sCaregiver Health(REACH)Skills2CareSAVVY CaregiverSHARE forDementia19. Gitlin, L. N., & Hodgson, N. A. m
Evidence Base for Dementia CareModels§ Multiple dementia care models have been testedin clinical trials and evidence from these trials hasbeen reviewed.§ These models have been shown to improvepatient and caregiver symptoms§ These models may also delay nursing home useand reduce total health care utilization or cost§ There is only limited evidence that these modelsreduce total health care utilization or cost§ Under-developed research on home redesign andincorporation of technology20. Coleman, K., Austin, B. T., Brach, C., & Wagner, E. H. (2009). Evidence on the chronic care model in the new millennium. Health Affairs, 28(1), 75-85.21. Boult, C., Counsell, S. R., Leipzig, R. M., & Berenson, R. A. (2010). The urgency of preparing primary care physicians to care for older people with chronic illnesses. HealthAffairs, 29(5), 811-818.22. Callahan, C. M., Sachs, G. A., LaMantia, M. A., Unroe, K. T., Arling, G., & Boustani, M. A. (2014). Redesigning systems of care for older adults with Alzheimer’s disease. Healthaffairs, 33(4), 626-632.23. Gitlin, L. N., Marx, K., Stanley, I. H., & Hodgson, N. (2015). Translating evidence-based dementia caregiving interventions into practice: State-of-the-science and next steps. TheGerontologist, 55(2), om
One-Third of Dementia Cases MayBe Preventable24. Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S. G., Huntley, J., Ames, D., . & Cooper, C. (2017). Dementia prevention, intervention, and care. The Lancet, 390(10113), .com
Strategies and Tools to ImproveDementia Care in the FinancialAlignment InitiativeDementia Cal MediConnect Project26Debra Cherry, PhDMegan Dankmyer, MSGExecutive Vice President,Alzheimer’s Los AngelesAssociate Vice President of CaseManagement, Molina om
Structure of California’s DementiaCal MediConnect m
Indicators for a More DementiaCapable System of Care1) Better detection and documentation of people living withdementia2) Better identification, assessment, support, and engagementof family/friend caregivers3) Better partnerships with community-based are.com
The Dementia Cal MediConnectProjectKey .com
Better Detection of Patients withDementia§ Include cognitive impairmentquestions in the Health RiskAssessment (HRA) and otherassessments§ Adopt a validated screening tool§ Document cognitive assessmentin the medical record§ Establish a follow-up protocol ifthe cognitive screen is positive SampleScreening Tools*AD8 Dementia ScreeningInterviewMini-CogGPCOG Screening TestMini Mental Status ExamAvailable from:Alzheimersla.org/professionals orin the KAER toolkit* All tools are com
Caregiver Id
1. Recognize how cognitive impairment and dementia impact the well - being of older adults and family caregivers 2. Identify opportunities to reduce the high health care and societal costs of dementia 3. Recognize key features of dementia capable