Transcription
The New Age of Insulin:Exploring the Latest Trends inInsulin TherapySusan Cornell, PharmD, CDE, FAPhA, FAADEAssociate Director of Experiential EducationAssociate Professor of Pharmacy PracticeMidwestern University Chicago College of PharmacyDowners Grove, IL1DisclosureConflicts of Interest and Financial Relationships Disclosures:Susan Cornell, PharmD, CDE, FAPhA, FAADE Advanced Practitioner Advisory Board andSpeaker’s Bureau: Sanofi, Novo Nordisk.2ObjectivesAt the conclusion of this knowledge‐based educational activity,participants will be able to:1. Discuss the current trends in the pathophysiology andprogressive nature of diabetes.2. Describe implications for the use of different insulinproducts in the diabetes management and care plan.3. Compare the pharmacokinetic and pharmacodynamicparameters of insulin formulations and delivery methods.3
International Diabetes Federation. http://www.idf.org/about-diabetes/facts-figures (accessed 2016 Aug 20).429.1 millionwith Diabetes86 millionwith PrediabetesCenters for Disease Control and Prevention (CDC). National diabetes statistics report, 4/national-diabetes-report-web.pdf (accessed 2016 Aug 20).Why is Glucose Control Important? 60% of people with type 2 diabetes have at leastone complication because of diabetes Complications are often present at time ofdiagnosisAACE. State of diabetes complications in America. ocs/Diabetes Complications Report.pdf (accessed 2016 Aug 20).6
Change in insulin / change glucose / IRβ‐cell Decline in Prediabetesand lucosetoleranceIR insulin ype 2 diabetesDeFronzo RA. Diabetes. 2009; 58:773-95.7The Ominous Octet:Circa 2008BrainPeripheral tissuePancreas‐ ß‐cellPancreas – α‐cellmuscleeHyperglycemiaLiverFat cells(adiposetissue)GI tract‐stomach/smallintestineKidneyCornell S et al. Postgrad Med. 2012; 124:84-94.Defronzo RA. Diabetes. 2009; 58:773-95.Treatment Approach to T2DM Dietary changes– Reduce consumption of calories– Reduce consumption of simple carbohydrates Increase physical activity Medications– Improve or replace insulin secretion– Reduce insulin resistance– Reduce glucagon secretion– Reduce hepatic glucose production– Increase urinary glucose excretionDeFronzo RA et al. Diabetes Care. 2013; 36(suppl 2):S127-38.98
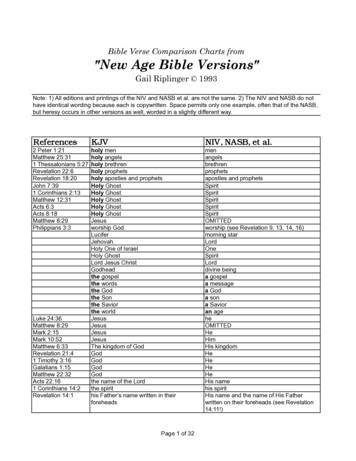
ADA Standards of Medical Care (2017)American Diabetes Association.Diabetes Care 2017;40:(Suppl 1).11Garber AJ. Endocr Pract 2016;22(1):84-113.Glucose‐Lowering ComparisonMonotherapyUsed in Pre‐DiabetesTargets InsulinResistanceTarget Glucose:FPG or PPGA1C inidesNoNoPPG0.5‐2.0AGIsYesNoPPG0.5‐1.0DPP‐4 inhibitorsNoNoPPG0.5‐0.7Bile acid sequestrantNoNoPPGDopamine agonistsNoNoPPG0.4SGLT‐2 inhibitorsNoMaybe?FPG0.7 – 1.10.8‐1.50.4GLP‐1 agonistsYesNoShort‐acting – PPGLong‐acting – BothAmylin analogsNoNoPPG0.6InsulinNoYes (to a degree)Basal – FPGBolus – PPG as much as neededAGIs alpha‐glucosidase inhibitors; DPP‐4 dipeptidyl peptidase 4; GLP‐1 glucagon‐like peptide‐1; FPG fasting plasmaglucose; PPG postprandial glucose; SGLT‐2 sodium‐glucose cotransporter 2.Unger J, et al. Postgrad Med. 2010;122(3):145‐157. Cornell S, et al. Postgrad Med. 2012;124(4):84‐94.12
Insulin “fixes 5 defectsBrainPeripheral tissuePancreas‐ ß‐cellPancreas – α‐cellmuscleeHyperglycemiaLiverFat cells(adiposetissue)GI tract‐stomach/smallintestineKidneyCornell S et al. Postgrad Med. 2012; 124:84-94.Defronzo RA. Diabetes. 2009; 58:773-95.13GLP‐1RA “fixes” 6 defectsBrainPeripheral tissuePancreas‐ ß‐cellPancreas – α‐cellmuscleeHyperglycemiaLiverFat cells(adiposetissue)GI tract‐stomach/smallintestineKidneyCornell S et al. Postgrad Med. 2012; 124:84-94.Defronzo RA. Diabetes. 2009; 58:773-95.Insulin Resistance Major defect in individuals with type 2 diabetes Reduced biological response to insulin Closely associated with obesity Associated with cardiovascular risk Type 1 diabetes patients can be insulin resistant aswellAmerican Diabetes Association. Diabetes Care. 1998;21(2):310‐314. Beck‐Nielsen H, et al. J Clin Invest.1994;94(5):1714‐1721. Bloomgarden ZT. Clin Ther. 1998;20(2):216‐231. Boden G. Diabetes. 1997;46(1):3‐10.1514
Insulin Therapy for Insulin Resistance Insulin, insulin, and yet more insulin! Causes weight gain and fluid retention Increased risk of hypoglycemia Expensive at high volumes (especially the pens) Multiple injections per day often needed Pumps not practical with high‐volume insulin usageAmerican Diabetes Association. Diabetes Care. 2016;39(Suppl 1):S6‐S12.16High Doses of Insulin Concerns: Hypoglycemia Medication errors in dosing Absorption issues Patient insulin variability (pharmacokinetics andpharmacodynamics) Problems: Over‐basalization Failure to treat the physiological defects Insulin resistance Decrease satiety17Thinking like a PancreasBasalMore for “Dawn phenomenon”BolusLess overnight8 am12N3 pm6 pm9 pm3 am7 am18
19The Basal‐Bolus Concept “Components” of Insulin Replacement Basal insulin: 50% of daily needs Controls nighttime and between‐meal glucose at a nearlyconstant level Bolus insulin: 50% of daily needs Controls mealtime glucose 10% to 20% of total daily insulin requirement at each meal Correction dose (sensitivity factor) Additional insulin needed (usually pre‐meal) Often to correct for fasting hyperglycemia19Pharmacokinetic Profile ofCurrently Available InsulinsPlasma Insulin LevelsRapid (aspart, lispro, glulisine, insulin human [inhaled])Short (regular U‐100)Mixed short/intermediate (regular U‐500)Intermediate (NPH)Long (detemir)Long (U‐100 glargine)Ultra‐long (degludec U‐100 & U‐200)Glargine U‐300024681012141618202224262830323436Time (hr)Hirsch IB. N Engl J Med. 2005; 352:174-83.Flood TM. J Fam Pract. 2007; 56(suppl 1):S1-S12.Becker RH et al. Diabetes Care. 2015; 38:637-43.20Insulin ComparisonInsulinOnset (hr)Peak (hr)Duration (hr)AppearanceInsulin Lispro U100 & U200Insulin AspartInsulin GlulisineRegular U100Regular inhaledwithin 15 minwithin 15 min0.25-0.50.5 – 1Within 5 min0.5- 1.51-30.5-12-420-40 r U-50030 min2-4Up to 24 hrClearNPH1-24-1014 CloudyInsulin Detemir3-46-8 (though relatively flat) up to 20-24ClearInsulin Glargine U1001.5flat24ClearInsulin Glargine U3001.5flat26ClearInsulin Degludec U100 & U2000.5 – 1flat 30ClearLispro Mix 50/50Lispro Mix 75/25Aspart Mix 70/30Degludec/aspart Mix 70/300.25-0.50.25-0.50.1-0.20.23 – 1.20.5-30.5-2.51-42.314-2414-2418-24 24CloudyCloudyCloudyCloudyNote: Patient specific onset, peak, duration may vary from times listed in table. Peak and duration are often verydose-dependent with shorter duration of actions with smaller doses and vice versa.21
Insulin Strategies in T2DM Metformin basal insulin Fasting coverage Hypoglycemic risk Glargine, detemir, degludec – lower risk Human insulin isophane (NPH) – higher risk Weight gain/neutral Basal insulin bolus insulin (with or without metformin) Fasting and postprandial coverage High hypoglycemic risk (mostly from bolus) Regular, aspart, lispro, glulisine Weight gain Basal insulin GLP‐1 agonist (with or without metformin) Fasting and postprandial coverage Low hypoglycemic risk (glargine, detemir, degludec) Weight neutral/lossInzucchi SE et al. Diabetes Care. 2015; 38:140-9.22Approach To Starting and Adjusting Insulin in T2DInitiate Basal InsulinUsually with metformin /- other noninsulin agentStart: 10 U/day or 0.1-0.2 U/Kg/dayAdjust: 10-15% or 2-4 units once/twice weekly to reach FBG targetFor hypo: identify/fix cause; can decrease does by 10-20% or 4 units.Add 1 rapid-acting insulin injection beforelargest --------Start: 4 units, .01U/kg, or 10% basal dose.If A1c 8%, Can basal by same amountAdjust: dose by 1-2 units or 10-15% onceonce/twice weekly until reach SMBG targetFor hypo: identify/fix cause; can does by2-4 units or 10-20%If A1c not controlled - ConsiderAdd GLP-1RA---------------------------If not tolerated or A1ctarget not reached, changeto 2 injections insulinregimen.If A1c not controlled - ConsiderChange to premixed insulin twice daily(before breakfast and -----------Start: Divide current basal dose into2/3 AM & 1/3 PM or ½ AM & ½ PMAdjust: dose by 1-2 units or 10-15%once once/twice weekly until reach SMBGtargetFor hypo: identify/fix cause; can does by2-4 units or 10-20%If A1c not controlled - ConsiderAdd 2 rapid-acting insulin injection before -----------------------Start: 4 units, .01U/kg, or 10% basal dose.If A1c 8%, Can basal by same amountAdjust: dose by 1-2 units or 10-15% onceonce/twice weekly until reach SMBG targetFor hypo: identify/fix cause; can does by 2-4 unitsor 10-20%Change to premixed analog insulin 3 times daily(breakfast, lunch, ------------Start: add additional injection before lunchAdjust: dose by 1-2 units or 10-15% onceonce/twice weekly until reach SMBG targetFor hypo: identify/fix cause; can does by 2-4 units or10-20%23Adapted from Approaches to Glycemic Treatment. Diabetes Care 2017;40(suppl 1):S67.Concentrated & “Low Volume” Insulin24
The Evolution of InsulinBovineinsulin(1922)Lente ulisine(2004)Aspart,glargine(2000)Detemir(2005)The history of insulin. www.karger.com/ProdukteDB/Katalogteile/isbn3 8055/ 83/ 53/Insulin 02.pdf(accessed 2016 Aug 20).25Polling Question #1Which insulin is not a true basal insulin?1.2.3.4.Insulin detemir U‐100Insulin glargine U‐100NPH U‐100Regular insulin U‐50026“Concentrated and/or Low Volume” Insulins Basal Insulin degludec (U‐100, U‐200) Insulin glargine (U‐300) Bolus Insulin lispro (U‐200) Bolus that thinks it’s a basal Insulin human regular (U‐500 pen)27
Pharmacokinetic Profile ofCurrently Available “Basal” InsulinsPlasma Insulin LevelsMixed short/intermediate (regular U‐500)Intermediate (NPH)Long (detemir)Long (U‐100 glargine)Ultra‐long (degludec U‐100 & U‐200)(glargine U‐300)024681012141618202224262830323436Time (hr)Hirsch IB. N Engl J Med. 2005; 352:174-83.Flood TM. J Fam Pract. 2007; 56(suppl 1):S1-S12.28Becker RH et al. Diabetes Care. 2015; 38:637-43.“Basal” Insulin ComparisonInsulin - BolusOnset (hr)Peak (hr)Duration (hr)AppearanceRegularU-50030 min2-4Up to 24 hrClearCloudyInsulin - BasalNPHInsulin DetemirInsulin GlargineU100Insulin GlargineU300Insulin DegludecU100 & U2001-24-1014 3-46-8 (thoughrelatively flat)up to 16-20Clear1.5flat20-24Clear1.5flat26Clear0.5 – 1flat 30ClearNote: Patient specific onset, peak, duration may vary from times listed in table. Peak and duration areoften very dose dependent with shorter duration of actions with smaller doses and vice versa.29Candidates for Concentrated/Low Volume InsulinConditionRationaleProduct to ConsiderNocturnal hypoglycemiaNeeds peak‐less (flat) basalinsulin profileDegludec U‐100, U‐200Glargine U‐300Insulin resistance(severe with high insulinrequirements;e.g. 200 units TDD)Temporary “fix” for insulinresistanceRegular U‐500High basal insulin needs( 80 units per injection)High dose requires 2 basalinjections/dayDegludec U‐200Glargine U‐300High bolus insulin needs( 20 units per day)Reduces the number of penchanges per monthLispro U‐200TDD total daily doseAdapted from Smith J, Rx Consultant 201630
Safety Concerns with “Newer” Insulins Familiarity with new products Understanding of pharmacokinetic andpharmacodynamic nuances Knowledge on dose adjustments and conversions “Lack” of interchangeability31Rationale for Concentrated Insulin Use When daily insulin requirements are in excess of 200 units/day, thevolume of U‐100 injected insulin may become an issue Physically too large for a single subcutaneous administration Multiple injections are required to deliver a single dose Increased injections may lead to compliance issues and poorglycemic control Discomfort Unpredictable absorption (rate‐limiting step in insulin activity)32Insulin Human Regular U‐500 Insulin characteristics Five times as concentrated as U‐100 insulin Decreased injection volume (vs. U‐100) Solely for severely insulin‐resistant patients Total daily dose exceeding 200 units/day Pharmacokinetics/pharmacodynamics Mean onset of action 15 minutes Mean duration of action 21 hours (range 13‐24 hours) Each individual patient varies in their response depending on: Site of injection Exercise patterns Other variables Clinical pearls Time to onset: similar to U‐100 regular insulin Duration of effect: similar to NPH insulin Consider it a “mixed short/intermediate” type insulinHumulin R U‐500 (insulin human injection, solution) PI. Eli Lilly and Company; 2016 33Mar.
PK and PD profiles forU-500 vs U-100 Human InsulinHuman Regular U-100 Insulin100080060040020000Glucose Infusion Rate(mg/min)Mean Serum IRIConcentration (pmol/L)50-Unit Dose12004812162050-Unit Dose6004002000048121620100-Unit Dose12001000800600400200001000800140024Glucose Infusion Rate(mg/min)Mean Serum IRIConcentration (pmol/L)Human Regular U-500 Insulin140048100012162024100-Unit Dose80060040020002404812162024IRI immunoreactive insulin; PK pharmacokinetic; PD pharmacodynamic.de la Peña A, et al. Diabetes Care. 2011;34(12):2496-2501.34Human Regular U‐500 Now available in an insulin pen: 1500 units/pen Maximum 300 units/injection No “dose conversions” needed Dials in increments of 5 units Still available in vial form (20 mL) New syringe dedicated for U‐500 approved July 2016 Use with U‐500 insulin onlyHumulin R U‐500 (insulin human injection, pen) PI. Eli Lilly and Company; 2016 Sept.35Regular U‐100 to U‐500 Dosing Converting from any U‐100 insulin to U‐500 human regularinsulin: A1C 8%: empiric reductions in total daily dose (TDD)of 10‐20% have been recommended A1C 10%: empiric increases in TDD of 10‐20% canbe considered Distributing the Total Daily Dose (TDD): Recommendations vary from 2‐3 doses per day Algorithm available Administer 30 minutes before meals due to the relativelyshort onset of actionLane WS, et al. Endocr Pract. 2009;15(1):71‐9.Cochran E, Musso C, Gordon P. Diabetes Care. 2005;28:1240‐4.36
Regular U‐500 to U‐100 Dosing No recommendations are currently available on howto convert from Regular U‐500 to basal‐bolus U100dosing Can differ based on delivery device used Pen vs. U‐100 insulin syringe or TB syringe Clinical expertise warranted37Concentrated Glargine (U‐300) Smaller depot surface area Reduced rate of absorption Relatively flat and prolonged PK/PD profiles Half‐life 23 hours Steady state in 4 days Duration of action 36 hours Available only in a pen 450 units/pen (1.5 mL) Maximum 80 units/injection 3 pens per boxGarber AJ. Diabetes Obes Metab. 2014;16(6):483‐491.Owens DR, et al. Diabetes Metab Res Rev. 2014;30(2):104‐119.Steinstraesser A, et al. Diabetes Obes Metab. 2014;16(9):873‐876.38US Food and Drug Administration. www.accessdata.fda.gov/scripts/cder/drugsatfda/PK and PD of U-300 Insulin Glarginevs U-100 Insulin GlargineU‐300 glargine displays a more even and prolonged PK/PD profile compared with U‐100glargine, offering blood glucose control beyond 24 ‐1]03Gla‐100 0.4 U/kg‐1Gla‐300 0.4 U/kg‐12N 3010061218243036LLOQ lower limit of quantification; GIR glucose infusion rate.Becker RH, et al. Diabetes Care. 2015;38(4):637-643.39
Glargine U‐100 to U‐300 Dosing Changing from once daily long‐acting: Initial dose can be same U‐100 insulinglargine Expect that a higher daily dose of U‐300 insulin glarginewill be needed to maintain the same level of glycemiccontrol Changing from BID NPH insulin: Initial dose is 80% of the total daily NPHdosageToujeo (insulin glargine injection) U-300 PI. sanofi-aventis U.S.; 2016 Sept.40Glargine U‐300 to U‐100 Dosing When converting from U‐300 to U‐100 A 20% reduction is recommended to minimizehypoglycemic risk with the U‐100 insulin productToujeo (insulin glargine injection) U-300 PI. sanofi-aventis U.S.; 2016 Sept.41Insulin Degludec (U‐100 & U‐200) “Ultra long acting” insulin Relatively flat and prolonged PK/PD profiles–Duration of action 42 hours (at least)–Half‐life 25 hours–Steady state in 3 to 4 days–Less patient insulin variability Flexible dosing schedule Available only in a pen–U‐200: 600 units/pen (3 mL), max 160 units/injection Dial in increments of 2 units!–U‐100: 300 units/pen (3 mL), max 80 units/injectionGarber AJ. Diabetes Obes Metab. 2014;16(6):483-491.Owens DR, et al. Diabetes Metab Res Rev. 2014;30(2):104-119.US Food and Drug Administration. www.accessdata.fda.gov/scripts/cder/drugsatfda/42
43Basal Insulin DegludecFlat, stable profile of both 100 unit/mL and 200 unit/mL formulationsMean 24‐Hour GIR Profile of the Two Insulin DegludecFormulations at Steady State5GIR4IDeg 100 U/mL 0.8 U/kgIDeg 100 U/mL 0.6 U/kgIDeg 100 U/mL 0.4 U/kgIDeg 200 U/mL 0.6 U/kgMeanHalf‐life(hours)Half‐life atSteady StateIDeg 200 U/mL0.6 U/kg26.2 h32n 211n 37n 16n 220Day 6Day 7GIR glucose infusion rate.43Heise T, et al. Diabetes. 2012;61(suppl 1):A91 [abstract 349-OR]. Heise T, et al. Diabetes Obes Metab.2012;14(10):944-950.Degludec U‐200 Dosing Changing from once daily long‐acting: The dose is 1 to 1 Initial degludec dose can be same as the current U‐100 insulinthe patient is using Glargine/detemir/degludec Changing from BID NPH insulin: The dose is 1 to 1: Initial degludec (once daily) dose is same as the total dailyNPH dosageTresiba (insulin degludec injection) PI. Novo Nordisk Inc; 2016 Sept.44Degludec U‐200 to U‐100 Dosing When converting from U‐200 to U‐100 The dose is a 1 to 1 conversion No change in the initial dose is necessaryTresiba (insulin degludec injection) PI. Novo Nordisk Inc; 2016 Sept.45
Concentrated Basal Insulin DosingConversion ComparisonGlargine U‐300Degludec U‐200Human R U‐500True basal insulinTrue basal insulinMixed basal/bolus insulin1 dailyinjection1 to 12 dailyinjections80% oftotal dailybasal dose2 dailyinjections80% oftotal dailybasal doseMaximumsingle‐doseinjection80 unitsMaximumsingle‐doseinjection160 units1 dailyinjection1 to 1Multiple dailyinjections ofbasal‐bolusTotal dailydose dividedinto 2 or 3Maximumsingle‐doseinjection300 unitsDialed in 1‐unit incrementsDialed in 2‐unit incrementsDialed in 5‐unit increments450 units of insulin per pen600 units of insulin per pen1500 units of insulin per penExpect higher daily dose ofglargine U‐300 tomaintain glycemic controlMonitor for hypoglycemia;administer with meals46Tresiba package insert, Toujeo package insert, Insulin regular U-500 package insertInsulin lispro (U‐200) No difference in kinetics from U‐100 lispro Half‐life: 1 hour Duration of action: 3 hours Available only in a pen 600 units/pen (3 mL) Maximum 60 units/injection 2 pens per box Addresses the problem of frequent pen turnoverHumalog U-200 Package insert47Patient Education Equipment and supplies needed to effectivelymanage insulin therapy at home: Insulin Syringes or pen needles Blood glucose meter and strips Lancets and lancing device Glucagon emergency kit Contact information of diabetes care provider(s)48
What Patients Need to Know AboutInsulin AND Delivery Devices Storage and expiration When it should be refrigerated When it can be at room temperature When medication expires after first use How to prepare product for first use How to properly use the device How to dispose of the device49Product dOnce used (opened)VialsInsulin lispro U‐100Insulin aspartInsulin glulisineInsulin glargineExpiration Date28 days28 daysVialsInsulin human NInsulin human RExpiration Date31 d
U300 1.5 flat 26 Clear Insulin Degludec U100 & U200 0.5 – 1 flat 30 Clear Note: Patient specific onset, peak, duration may vary from times listed in table. Peak and duration are often very dose dependent with shorter duration of actions with smaller doses and vi