Transcription
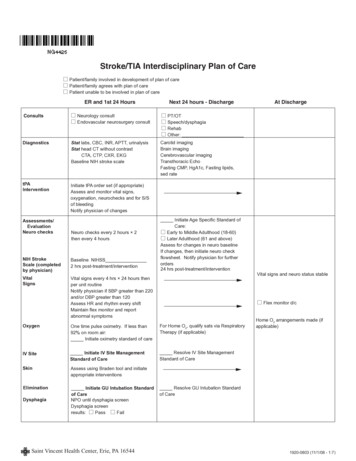
Stroke/TIA Interdisciplinary Plan of Care Patient/family involved in development of plan of care Patient/family agrees with plan of care Patient unable to be involved in plan of careER and 1st 24 HoursNext 24 hours - DischargeConsults Neurology consult Endovascular neurosurgery consult PT/OT Speech/dysphagia Rehab Other:DiagnosticsStat labs, CBC, INR, APTT, urinalysisStat head CT without contrastCTA, CTP, CXR, EKGBaseline NIH stroke scaleCarotid imagingBrain imagingCerebrovascular imagingTransthoracic EchoFasting CMP, HgA1c, Fasting lipids,sed ratetPAInterventionInitiate tPA order set (if appropriate)Assess and monitor vital signs,oxygenation, neurochecks and for S/Sof bleedingNotify physician of changesAssessments/EvaluationNeuro checksNeuro checks every 2 hours 2then every 4 hoursNIH StrokeScale (completedby physician)Baseline NIHSS2 hrs post-treatment/interventionVitalSignsVital signs every 4 hrs 24 hours thenper unit routineNotify physician if SBP greater than 220and/or DBP greater than 120Assess HR and rhythm every shiftMaintain flex monitor and reportabnormal symptomsInitiate Age Specific Standard ofCare:Early to Middle Adulthood (18-60)Later Adulthood (61 and above)Assess for changes in neuro baselineIf changes, then initiate neuro checkflowsheet. Notify physician for furtherorders24 hrs post-treatment/intervention One time pulse oximetry. If less than92% on room air:Initiate oximetry standard of careFor Home O2, qualify sats via RespiratoryTherapy (if applicable)IV SiteInitiate IV Site ManagementStandard of CareResolve IV Site ManagementStandard of CareSkinAssess using Braden tool and initiateappropriate interventionsEliminationInitiate GU Intubation Standardof CareNPO until dysphagia screenDysphagia screenresults:PassFail Vital signs and neuro status stable Flex monitor d/cOxygenDysphagiaAt DischargeHome O2 arrangements made (ifapplicable)Resolve GU Intubation Standardof Care Saint Vincent Health Center, Erie, PA 165441920-0803 (11/1/08 - 1:7)
Stroke/TIA Interdisciplinary Plan of CareER and 1st 24 HoursNutritionIf FAIL dysphagia screen, keep patientNPO and consult speechIf PASS dysphagia screen, then diet:Diet as tolerated, low animal fatDiabetic 1800 calOther: Activity/Safety Activity:OOBOOB with assistanceOther:Turn and position every 2 hours while inbed if unable to move selfMonitor fall risk and documentinterventions per Morse Score LipidsDVT/ProphylaxisNext 24 hours - Discharge Tube feedingInitiate GI Intubation Standardof CareWhen patient identified with dysphagia,follow recommendations from speechtherapistInitiate AnticoagulationStandard of Care Ambulating without any assistance Lovenox Coumadin SEQsResolve GI Intubation Standard ofCarePatient will tolerate nutrition withoutaspirationMonitor tolerance of ordered diet/supplement.Attend and participate in PT/OTProvide appropriate teaching tool IV Heparin Stroke protocol Coumadin Lovenox ASA Plavix AggrenoxAt DischargeInstruct patient in Lovenox selfadministration and managment ofanticoagulantsResolve Anticoagulation Standardof Care Lipitor Zocor Niacin Pravachol Gemfibrozil Other:If patient not ambulating independentlyby the end of hospital day 2, must initiateDVT prophylaxisPatient/family knowledgeable inanticoagulant and antiplatelet therapyLab draws arrangedLovenox arrangements completedPatient/family self-administers LovenoxEnsure patient is discharged on lipidlowering agents if LDLgreater than 100,HDL less than 40 or triglycerides greaterthan 150Patient/FamilyOrient to unit and roomPrepare for dischargeReview and give pt/family DischargeTeachingUpdate patient/family about conditionInitiate teaching tool and use to ContractAssess learning needs and homeinstruct patient/caregiver on:situation- Stroke warning signs & symptomsEnsure physician has completedGive patient stroke booklet- Activation of EMS Stroke EBP discharge planExplain treatments- Personal risk factors & preventionProvide emotional support- Medication TeachingPatient/family able to safely manageProvide patient/family with TV guide- Importance of routine follow up with care at homeand instruct to watch stroke-relatedPCPvideos- Disease process- Complications- Safety- ActivityDocument appropriate dischargeinstructions on Stroke/TIA dischargecontractGive home safety tip sheetSaint Vincent Health Center, Erie, PA 165441920-0803 (11/1/08 - 2:7)
Stroke/TIA Interdisciplinary Plan of CareKey Patient OutcomesKPO Problem ListER & 1st 24 HoursDischargePlanningNotify Care Coordination Services for- Home Health Referral- placement- rehab/transitional care- medication assistanceHemodynamicsand ArrhythmiasPatient will be hemodynamicallystable as evidenced by SBP less than220 DBP less than 120 (every shift)Patient in normal sinus rhythm orcontrolled Afib - (every shift)Adequate Intake/OutputOxygenationPatient will maintain O2 sat above92% (every shift)Patient exhibits adequate pulmonaryhygiene as evidenced by (every shift) maintenance of patient airway clear BBS effective cough airway clearanceSafetyPatient will be free of injury fromfalls - (every shift)Complications ofStroke/TIAPatient will be free of preventablecomplications (every shift) thrombophebitis choking/aspiration foot dropPatient will remain free of furtherbrain injury as evidenced by stable orimproving neuro status (every shift)Knowledge Deficiton TeachingPatient and family will verbalize and/ordemonstrate knowledge of1. Stroke warning signs & symptoms2. Activation of EMS3. Personal risk factors & prevention4. Medication teaching5. Importance of routine follow upwith Primary Care PhysicianCopingMechanismsNext 24 Hours - DischargeAppropriate referrals/follow-up initiatedand completedPatient and family will demonstrateappropriate coping mechanisms asevidenced by participation in therapy & D/C planning verbalizing & expressing concerns(every day)NutritionPatient will maintain adequate nutritionalstatus as evidenced by greater than75% of meals or via alternative sourceof nutrition at goal rate (i.e. TPN or tubefeedings)HomeMaintenance/D/C PlanningPatient/family will demonstrate andverbalize knowledge of: disease process complications safety communication/cognition prevention/risk factors medications, as precribed proper home managementSaint Vincent Health Center, Erie, PA 16544At DischargePatient/family will demonstrate andverbalize understanding of all postdischarge needs and care1920-0803 (11/1/08 - 3:7)
Patient StamperHemorrhagic Stroke/Ischemic Stroke/TIA Teaching ducatorDateLearnerq Hemorrhagic Strokeq Ischemic Strokeq TIAMethodUpon completion of teaching, patient and/or Learner/Caregiver(s) will demonstrate and/or verbalize knowledge of:STROKE ESSENTIALS (all videos are on TV channel 16)*Give Stroke Essentials Folder w/booklet and magnetComments:*Stroke Warning Signs and Symptoms*Activation of Emergency Medical Services (EMS)/911*Importance of Routine Physician follow-up after dischargeReview physiology of diagnosisStroke videos, especially video: “Stroke: Reducing the risk”*PERSONAL RISK FACTORS FOR PREVENTION AND/ORLIFESTYLE CHANGE (checked box indicates reviewed)Comments:q High Blood Pressureq Smoking Cessationq Elevated cholesterol (goal LDL 100, total cholesterol 200)q Diabetes Managementq Weight and BMI (obese greater than or equal to 25)q Physical Inactivity / Exerciseq Nutrition / Diet / Alcoholq Atrial Fibrillationq Carotid Stenosisq Illicit drug use (i.e. cocaine)q Other:qq*MEDICATIONS (checked box indicates reviewed)q Antiplatelets (q aspirin q clopidogrel q dipyridamole/aspirin)Comments:q Anticoagulants (q warfarin q heparin q enoxaparin)q Lipid-lowering medication (q statins q other)q Diabetic medicationsq Blood Pressureq Otherqq*Major components required for patient educationLearner CodesPt – PatientLearner (enter initials)Caregiver (enter initials)Learner/CaregiverTeaching Method CodesV – VerbalAV – AudiovisualW – WrittenD – Demo/redemoInitialsSaint Vincent Health Center, Erie, PA 16544Evaluation Code1. Pt, learner, caregiver verbalizes/demonstrates knowledge2. Needs reinforcement3. Refused education4. Education given to member of nursing home, home health or othercaregiver staff memberEducator SignatureInitialsEducator SignatureInitials1920-0803 (11/1/08 - 4:7)
GENERAL TEACHING TOOL INSTRUCTIONSPURPOSE:The Teaching Tool is an interdisciplinary document used to manually record the teaching that a patient or other learner,receives during the patient’s hospitalization.NATURE OF THE FORM:The Teaching Tool is a permanent part of the medical record. It is to be stamped or labeled with patient identificationinformation in the upper right hand corner and completed in black ink. The Teaching Tool may be general (GeneralMedical Teaching Tool or General Surgical Teaching Tool) or specific to a particular patient population or healthproblem.PERSONS RESPONSIBLE:The registered nurse will initiate the Teaching Tool, most appropriate to the patient’s educational needs, after completingthe Patient Admission Assessment/Screening Tool. More than one Teaching Tool may be needed for patients withmultiple health problems. Example: A CHF patient who is a newly diagnosed Type 2 Diabetic.Other members of the interdisciplinary team will document on the Teaching Tool as well as in discipline specific MISnotes.The registered nurse is responsible to review the Teaching Tool as part of the patient discharge process and completeany incomplete documentation. The MIS discharge contract and Discharge Instruction sheets are used as an additionalsource of patient education documentation.PLACEMENT IN CHART:The Teaching Tool(s) will be placed as the first item under the Notes Manual tab (lime green) of the chart. Other formsto be placed in order under the Teaching Tool in the Notes Manual Tab are: Teaching Tool Evidenced Based Tool Kit (Preprinted Interdisciplinary Plan of Care (IPC) and Key Patient Outcomes (KPO) Interdisciplinary Plan of Care (MIS care plan - only if needed) Interval Nursing Asssessment(s) Manual Nursing NotesSaint Vincent Health Center, Erie, PA 165441920-0803 (11/1/08 - 5:7)
Patient StamperHemorrhagic Stroke/Ischemic Stroke/TIA Teaching Tool uationEducatorDateLearnerq Hemorrhagic Strokeq Ischemic Strokeq TIAMethodUpon completion of teaching, patient and/or Learner/Caregiver(s) will demonstrate and/or verbalize knowledge of:SAFETY (checked box indicates reviewed)q Fall preventionComments:q Decreased sensationq Spatial/perceptual awarenessq OtherACTIVITY (checked box indicates reviewed)q Mobilityq TransfersComments:q ADLsq Medical equipment/assistive devicesq OtherTESTS/PROCEDURES (checked box indicates reviewed)Comments:q CT scanq CT angiogramq MRIq MRAq EKGq Echocardiogramq Carotid Ultrasoundq Trans-esophageal echocardiogram (TEE)q Flexq Dysphagia ScreenqqSTROKE RELATED COMPLICATIONS(checked box indicates reviewed)q AphasiaComments:q Communication/speech issuesq Plegia / paresisq Dysphagiaq Subluxation of shoulderq Neglectq DVT prophylaxis / preventionq Incontinenceq Active DVTqqUNIT ROUTINEq*Major components required for patient educationLearner CodesPt – PatientLearner (enter initials)Caregiver (enter initials)Learner/CaregiverTeaching Method CodesV – VerbalAV – AudiovisualW – WrittenD – Demo/redemoInitialsSaint VincentVincent HealthHealth Center,Center, Erie,Erie, PAPA 1654416544SaintEvaluation Code1. Pt, learner, caregiver verbalizes/demonstrates knowledge2. Needs reinforcement3. Refused education4. Education given to member of nursing home, home health or othercaregiver staff memberEducator SignatureInitialsEducator SignatureInitials1920-0803 (11/1/08(11/1/08 -- 6:7)5:7)1920-0803
SPECIAL INSTRUCTIONS:1. Content to be taught is found in the left-hand columns of the form. All specified items must be addressed with anevaluation code prior to patient discharge.2. Only one signature/evaluation is required in the first column to indicate that you have taught more than one topicunder the teaching category. Where indicated, you must check appropriate boxes for specific topics that youreviewed with the patient/caregiver/learner. The comment boxes in this column allow you to add comments about theteaching you have done. For example, you could write, “Reinforce a fib teaching with patient,” so others will knowthat this needs reviewed with the learner.3. The second column on the right allows you to document any re-education done or to address a single topic later, such as a test that was ordered after the initialeducation was done. reinforce education, if needed, with one learner (a return session) record teaching of more than one person for the same item4. Learning column: The code (Pt) is used when the patient is taught. If someone else is taught, on behalf of thepatient, record the persons’ name as the Caregiver(s)/Learner(s) and the person’s initials in the lower left box. Note:the learner does not need to sign the form. Those initials are used in the learner column to indicate who was taught.5. Method column: Use the Teaching Method codes, found at the bottom of the form, to indicate how the education waspresented to the learner.6. Date column: Mark the month and date of the education.7. Evaluation column: Use the evaluation codes, found at the botom of the form, to indicated the response to educationor why education was not given.1 Learner has shown by demonstration or verbalization that the material is understood.No further teaching needed.2 Learner needs to have the content reviewed again: more teaching is needed for learner to fully grasp the material a re-demo is needed, to assure proper technique is mastered3 Learner refuses to receive instruction or educational materials4 Learner is a professional staff member from a nursing home, home health agency that will be following patient,or other care
Stroke/TIA Interdisciplinary Plan of Care Consults Neurology consult Endovascular neurosurgery consult ER and 1st 24 Hours Next 24 hours - Discharge At Discharge Diagnostics PT/OT Speech/dysphagia Rehab Other: _ Stat labs, CBC, INR, APTT, urinalysis Stat File Size: 375KBPage Count: 9