Transcription
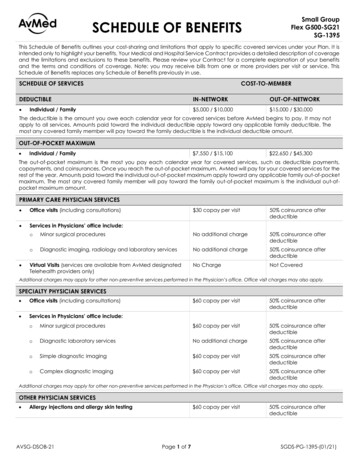
SCHEDULE OF BENEFITSSmall GroupFlex G500-SG21SG-1395This Schedule of Benefits outlines your cost-sharing and limitations that apply to specific covered services under your Plan. It isintended only to highlight your benefits. Your Medical and Hospital Service Contract provides a detailed description of coverageand the limitations and exclusions to these benefits. Please review your Contract for a complete explanation of your benefitsand the terms and conditions of coverage. Note: you may receive bills from one or more providers per visit or service. ThisSchedule of Benefits replaces any Schedule of Benefits previously in use.SCHEDULE OF SERVICESCOST-TO-MEMBERDEDUCTIBLE Individual / FamilyIN-NETWORKOUT-OF-NETWORK 5,000 / 10,000 15,000 / 30,000The deductible is the amount you owe each calendar year for covered services before AvMed begins to pay. It may notapply to all services. Amounts paid toward the individual deductible apply toward any applicable family deductible. Themost any covered family member will pay toward the family deductible is the individual deductible amount.OUT-OF-POCKET MAXIMUM Individual / Family 7,550 / 15,100 22,650 / 45,300The out-of-pocket maximum is the most you pay each calendar year for covered services, such as deductible payments,copayments, and coinsurances. Once you reach the out-of-pocket maximum, AvMed will pay for your covered services for therest of the year. Amounts paid toward the individual out-of-pocket maximum apply toward any applicable family out-of-pocketmaximum. The most any covered family member will pay toward the family out-of-pocket maximum is the individual out-ofpocket maximum amount.PRIMARY CARE PHYSICIAN SERVICES Office visits (including consultations) Services in Physicians’ office include: 30 copay per visit50% coinsurance afterdeductibleoMinor surgical proceduresNo additional charge50% coinsurance afterdeductibleoDiagnostic imaging, radiology and laboratory servicesNo additional charge50% coinsurance afterdeductibleNo ChargeNot CoveredVirtual Visits (services are available from AvMed designatedTelehealth providers only)Additional charges may apply for other non-preventive services performed in the Physician’s office. Office visit charges may also apply.SPECIALTY PHYSICIAN SERVICES Office visits (including consultations) Services in Physicians’ office include: 60 copay per visit50% coinsurance afterdeductibleoMinor surgical procedures 60 copay per visit50% coinsurance afterdeductibleoDiagnostic laboratory servicesNo additional charge50% coinsurance afterdeductibleoSimple diagnostic imaging 60 copay per visit50% coinsurance afterdeductibleoComplex diagnostic imaging 60 copay per visit50% coinsurance afterdeductibleAdditional charges may apply for other non-preventive services performed in the Physician’s office. Office visit charges may also apply.OTHER PHYSICIAN SERVICES Allergy injections and allergy skin testingAVSG-DSOB-21 60 copay per visitPage 1 of 750% coinsurance afterdeductibleSGDS-PG-1395-(01/21)
SCHEDULE OF BENEFITSSmall GroupFlex G500-SG21SG-1395COST-TO-MEMBERSCHEDULE OF SERVICESIN-NETWORKOUT-OF-NETWORK Podiatry serviceso Routine foot care is limited to medically necessaryservices for individuals with diabetes, peripheralcirculatory or neurovascular disease 30 copay per visit50% coinsurance afterdeductible Diabetes self-managementoIncludes care, education, and nutritional counseling 60 copay per visit50% coinsurance afterdeductibleCounseling by licensed nutritionist limited to 3 visits per calendar year. Additional charges may apply for other non-preventive servicesperformed in the Physician’s office. Office visit charges may also apply.PREVENTIVE CARE AND SERVICES Preventive care services:o Annual physical examinations and immunizationso Lactation support/counseling and breast pump supplieso Colorectal cancer screening, including colonoscopieso HIV screeningo Preventive radiology and laboratory serviceso Prostate specific antigen (PSA) testingo Routine screening mammogramso Voluntary family planning serviceso Well-child care and immunizations, including routinevision and hearing screenings by a pediatriciano Well-woman examinations, including Pap smearsNo Charge50% coinsurance afterdeductibleFor a comprehensive list of covered preventive services, visit e-benefits/.OUTPATIENT FACILITY SERVICES & DIAGNOSTIC TESTS OUTPATIENT FACILITY SERVICESoOutpatient surgeries (include cardiac catheterizationsand angioplasty) 750 copay per visit atindependent facilities;30% coinsurance afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductibleoPhysician charges for surgical and medical servicesNo Charge50% coinsurance afterdeductibleoDialysis services 750 copay per visit atindependent facilities;30% coinsurance afterdeductible at hospitalowned or affiliated facilitiesNot CoveredoRadiation therapy (covers administration and facilitycharges) 750 copay per course oftreatment at independentfacilities;30% coinsurance afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductibleOUTPATIENT DIAGNOSTIC TESTSoRoutine outpatient laboratory tests and blood work 30 copay per visit50% coinsurance afterdeductibleoSpecialty labs 750 copay per visit atindependent facilities;30% coinsurance afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductibleAVSG-DSOB-21Page 2 of 7SGDS-PG-1395-(01/21)
SCHEDULE OF BENEFITSSmall GroupFlex G500-SG21SG-1395COST-TO-MEMBERSCHEDULE OF SERVICESIN-NETWORKOUT-OF-NETWORKoSimple diagnostic tests (including x-rays, ultrasounds,echocardiograms, fluoroscopes, diagnosticmammography, and other standard radiology services) 100 copay per visit atindependent facilities;30% coinsurance afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductibleoComplex diagnostic tests (MRI, MRA, PET, CT, NuclearMedicine) 350 copay per visit atindependent facilities;30% coinsurance afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductibleOutpatient facility services require prior authorization. Please see your Contract for details.PRESCRIPTION DRUGS Tier 1: Value Generic Drugs 10 copay per prescription(retail); 25 copay per prescription(mail order)Not Covered Tier 2: Generic Drugs 20 copay per prescription(retail); 50 copay per prescription(mail order)Not Covered Tier 3: Preferred Brand Drugs 50 copay per prescription(retail); 125 copay per prescription(mail order)Not Covered Tier 4: Non-Preferred Brand Drugs 75 copay per prescription(retail); 187.50 copay perprescription (mail order)Not Covered Tier 5: Specialty Drugs50% coinsurance afterdeductible (retail only)Not CoveredBrand additional charge may apply if a Brand is selected when a Generic is available. Certain drugs require prior authorization. AvMed doesnot apply manufacturer or provider cost-share assistance program payments (e.g. manufacturer cost-share assistance, manufacturer discountplans, and/or manufacturer coupons) to the deductible or out-of-pocket maximums. Retail charge applies per 30-day supply. Mail-order chargeapplies per 60-90 day supply. AvMed’s commercial Formulary List is available at www.avmed.org under the Preferred Medication Lists section.INFUSION AND OTHER DRUG THERAPY Drug therapy administered by a medical professionaloin a Physician’s office 60 copay per visit50% coinsurance afterdeductibleoin the home 30 copay per visit50% coinsurance afterdeductibleoin an outpatient facility 120 copay per visit atindependent facilities;50% coinsurance afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductible50% coinsurance afterdeductible50% coinsurance afterdeductibleRequires prior authorization Chemotherapy (covers administration and facility charges)Requires prior authorizationAVSG-DSOB-21Page 3 of 7SGDS-PG-1395-(01/21)
SCHEDULE OF BENEFITSSmall GroupFlex G500-SG21SG-1395COST-TO-MEMBERSCHEDULE OF SERVICESIN-NETWORKOUT-OF-NETWORK 550 copay per visit 550 copay per visitIMMEDIATE / EMERGENCY CARE Emergency room services at participating or nonparticipating hospitals (copay waived if admitted)Charges for Physician services may also apply, and may be billed separately. AvMed must be notified within 24 hours of inpatient admissionfollowing emergency services or as soon as reasonably possible. Ambulance transport for emergency servicesoGround transport 150 copay per one wayground transport afterdeductible 150 copay per one wayground transport after InNetwork deductibleoAir and water transport50% coinsurance afterdeductible50% coinsurance after InNetwork deductible 150 copay per one wayground transport afterdeductible 150 copay per one wayground transport afterdeductibleNon-emergent ambulance serviceso Covered when the skill of medically trained personnel isrequired and the Member cannot be safely transportedby other meansRequires prior authorization Medical services at urgent/immediate care facilities 100 copay per visit atindependent facilities;30% coinsurance afterdeductible at hospitalowned or affiliated facilities 100 copay per visit afterdeductible at independentfacilities;50% coinsurance afterdeductible at hospitalowned or affiliated facilities Medical services at retail clinics 40 copay per visit 40 copay per visit afterdeductibleINPATIENT HOSPITAL Inpatient services at hospitals includes:o Room and board - unlimited days (semi-private)o Anesthesia, use of operating and recovery rooms,oxygen, drugs and medicationo Intensive care unit and other special units, general andspecial duty nursingo Laboratory and diagnostic imagingo Required special dietso Radiation and inhalation therapieso Acute rehabilitation services (limited to 30 days percalendar year) 750 copay per day for thefirst 3 days per admissionafter deductible50% coinsurance afterdeductible Physician charges for surgical and medical servicesNo charge after deductible50% coinsurance afterdeductibleInpatient services require prior authorization.MENTAL HEALTH AND SUBSTANCE ABUSE TREATMENT Office visits 30 copay per visit50% coinsurance afterdeductible Partial hospitalization.No Charge50% coinsurance afterdeductibleAVSG-DSOB-21Page 4 of 7SGDS-PG-1395-(01/21)
Small GroupFlex G500-SG21SG-1395SCHEDULE OF BENEFITSCOST-TO-MEMBERSCHEDULE OF SERVICES IN-NETWORKOUT-OF-NETWORKInpatient servicesoAcute care for mental health and substance usedisorders 750 copay per day for thefirst 3 days per admissionafter deductible50% coinsurance afterdeductibleoIntermediate care at residential treatment facilities 750 copay per day for thefirst 3 days per admissionafter deductible50% coinsurance afterdeductibleInpatient and partial hospitalization services require prior authorization.MATERNITY Pre- and post-natal careoRoutine office visits (including obstetrical and midwifeservices) 30 copay for first visit only;subsequent visits at nocharge50% coinsurance afterdeductibleoSpecialist office visits 60 copay per visit50% coinsurance afterdeductibleNo charge after deductible50% coinsurance afterdeductibleChildbirth/delivery professional serviceso Routine OB (including obstetrical and midwife services)Childbirth/delivery facility servicesoHospital 750 copay per day for thefirst 3 days per admissionafter deductible50% coinsurance afterdeductibleoBirthing center 30 copay per visit50% coinsurance afterdeductibleInpatient services require prior authorization. Maternity care may include tests and services described elsewhere in this document (e.g.,ultrasound). For lactation support/counseling and breast pump supply benefits, please see the Preventive Care and Services section.RECOVERY Home health care 60 copay per visit afterdeductible50% coinsurance afterdeductibleCoverage is limited to 20 skilled visits per calendar year. Approved treatment plan and prior authorization required. Rehabilitation servicesoShort-term physical, occupational and speech therapiesfor acute conditions 60 copay per visit atindependent facilities; 60 copay per visit afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductibleoCardiac rehabilitation for the following conditions: Acute myocardial infarction Percutaneous transluminal coronary angioplasty(PTCA) Repair or replacement of heart valves Coronary artery bypass graft (CABG) Heart transplantPulmonary rehabilitation 60 copay per visit atindependent facilities; 60 copay per visit afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductible 60 copay per visit atindependent facilities; 60 copay per visit afterdeductible at hospitalowned or affiliated facilities50% coinsurance afterdeductibleoAVSG-DSOB-21Page 5 of 7SGDS-PG-1395-(01/21)
SCHEDULE OF BENEFITSCOST-TO-MEMBERSCHEDULE OF SERVICES Small GroupFlex G500-SG21SG-1395Chiropractic servicesIN-NETWORKOUT-OF-NETWORK 30 copay per visit50% coinsurance afterdeductibleCoverage is limited to 35 visits per calendar year for outpatient rehabilitative PT, OT, ST, cardiac rehabilitation, pulmonary rehabilitation andchiropractic services combined. Cardiac and pulmonary rehabilitation require prior authorization. Habilitation serviceso Physical, occupational and speech therapies 60 copay per visit50% coinsurance afterdeductibleCoverage is limited to a combined maximum of 35 visits per calendar year for outpatient habilitative physical, occupational and speechtherapies. Skilled nursing facility 250 copay per day for thefirst 5 days per admissionafter deductible50% coinsurance afterdeductibleCoverage is limited to 60 days post-hospitalization care per calendar year. Requires prior authorization. Durable medical equipment includes:o Standard hospital bedso Walkerso Crutcheso Wheelchairs 100 copay per episode ofillness after deductible50% coinsurance afterdeductibleExcludes vehicle modifications, home modifications, exercise equipment, and bathroom equipment. Orthotic appliances 100 copay per deviceafter deductible50% coinsurance afterdeductible 100 copay per deviceafter deductible50% coinsurance afterdeductibleCoverage is limited to custom-made leg, arm, back, and neck braces. Prosthetic devicesCoverage is limited to artificial limbs, artificial joints, cochlear implants, and ocular prostheses. Please see your Contract for more details. Hospiceo Inpatient and outpatient servicesNo charge after deductible50% coinsurance afterdeductiblePhysician certification requiredPEDIATRIC VISION AND DENTAL SERVICES Pediatric VisionoOne exam per calendar year to determine the need forsight correctionNo Charge50% coinsurance afterdeductibleoOne pair of eye glasses per calendar year (Includesstandard lenses and frames. Members may choose froma pre-selected group of frames.)No Charge50% coinsurance afterdeductibleNo charge for preventivecare from Delta DentalNetwork providersPreventive care may besubject to cost-sharing ifbilled charges exceedallowed amount.Same as any othercondition based on type ofprovider and location ofservices50% coinsurance afterdeductiblePediatric Dentalo Dental services are subject to a separate calendar yeardeductible of 65 per child.o Cost-sharing for dental services from Delta DentalNetwork providers is limited to a separate out-of-pocketmaximum of 350 per child, or 700 for 2 or more children.The out-of-pocket maximum does not apply to Out-ofNetwork benefits.o Exams are limited to one every 6 months. Please see yourContract for details regarding benefits and cost-sharing.TEMPOROMANDIBULAR JOINT (TMJ) SYNDROME Medically necessary treatment for conditions caused bycongenital or developmental deformity, disease or injury.Requires prior authorizationAVSG-DSOB-21Page 6 of 7SGDS-PG-1395-(01/21)
SCHEDULE OF BENEFITSSmall GroupFlex G500-SG21SG-1395COST-TO-MEMBERSCHEDULE OF SERVICESIN-NETWORKOUT-OF-NETWORKSame as any othercondition based on type ofprovider and location ofservicesNot CoveredTRANSPLANT SERVICES AvMed In-Network Center of Excellence facilities in the Stateof Florida.Requires prior authorization - Limitations apply - please see your Contract for details.ALL OTHER COVERED SERVICESFor cost-sharing information about items or services not listed in this document, please see your Contract, or call AvMed’sMember Engagement Center at 1-800-376-6651. Please also call Member Engagement for assistance regarding claims, resolvinga complaint, or for information about covered services. You may also log onto your secure Member portal at www.avmed.orgwhich includes a health care cost estimator and information regarding Plan details.DISCLAIMER:This Schedule of Benefits is not a contract. Please see your AvMed Small Group Flex Medical and Hospital Service Contract forspecific information on benefits, exclusions and limitations. This Plan will be administered in accordance with the requirementsof state and federal law, including the Patient Protection and Affordable Care Act.G Flex Flex G500-SG21 1395 Small Group POS SGDS-PG-1395-(01/21) XXXXAVSG-DSOB-21Page 7 of 7SGDS-PG-1395-(01/21)
SCHEDULE OF BENEFITS Small Group Flex G500-SG21 SG-1395 AVSG-DSOB-21 Page 1 of 7 SGDS-PG-1395-(01/21) This Schedule of Benefits outlines your cost-sharing and limitations