Transcription
Centers for Medicare & Medicaid ServicesCenters for Medicare & Medicaid ServicesCMS Alliance to Modernize Healthcare (The Health FFRDC)A Federally Funded Research and Development CenterMedicare Ambulance Services Special AnalysisTask Order No. HHSM-500-T0052Medicare’s Ground Ambulance Data CollectionSystem: Sampling and Instrument Considerationsand RecommendationsFinalJuly 30, 2019The views, opinions, and/or findings contained in this report are those of The MITRE Corporation and should not beconstrued as official government position, policy, or decision unless so designated by other documentation. 2019, The MITRE Corporation. All Rights Reserved.Medicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.
Centers for Medicare & Medicaid ServicesAuthors of this Report (the Health FFRDC Team)Andrew Mulcahy (RAND)Kirsten Becker (RAND)Jonathan Cantor (RAND)Scott Ashwood (RAND)Jeanne Ringel (RAND)Lisa Sontag-Padilla (RAND)Christine Buttorff (RAND)Michael Robbins (RAND)Susan Lovejoy (RAND)Thomas Goughnour (RAND)Sara Heins (RAND)Beverly Weidmer (RAND)Monique Martineau (RAND)Mike Oelrich (MITRE)Jennifer Gildner (RAND)Gina Karimi (RAND)Thomas Goode (RAND)Medicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.ii
Centers for Medicare & Medicaid ServicesAcronymsAcronymDefinitionAAAAmerica Ambulance AssociationACSAmerican Community SurveyAFSAmbulance Fee ScheduleALSAdvanced Life SupportBBABipartisan Budget Act of 2018BLSBasic Life SupportCAHCritical Access HospitalCDCCenters for Disease Control and PreventionCESCost Element StructureCMSCenters for Medicare & Medicaid ServicesEMREmergency Medical ResponderEMSEmergency Medical ServicesEMSCAPEmergency Medical Services Cost Analysis ProjectESRDEnd-Stage Renal DiseaseFDAFood and Drug AdministrationFFRDCFederally Funded Research and Development CenterFTEFull-Time EquivalentGAOGovernment Accountability OfficeGEMTGround Emergency Medical TransportationHCPCSHealthcare Common Procedure Coding SystemHCRISHealthcare Cost Report Information SystemHHSDepartment of Health and Human ServicesHIPAAHealth Insurance Portability and Accountability ActHRSAHealth Resources and Services AdministrationIAFCInternational Association of Fire ChiefsIAFFInternational Association of Fire FightersIDRIntegrated Data RepositoryIOMInstitute of MedicineMedPACMedicare Payment and Advisory CommissionNAEMTNational Association of Emergency Medical TechniciansMedicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.iii
Centers for Medicare & Medicaid ServicesAcronymDefinitionNASEMSONational Association of State EMS OfficialsNHSTANational Highway Transportation Safety AdministrationNPINational Provider IdentifierNPPESNational Plan and Provider Enumeration SystemNRHANational Rural Health AssociationNVFCNational Volunteer Fire CouncilONCOffice of the National Coordinator for Health Information TechnologyPDFPortable Document FormatPECOSProvider Enrollment, Chain and Ownership SystemRVURelative Value UnitSNFSkilled Nursing FacilitySUVSport Utility VehicleMedicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.iv
Centers for Medicare & Medicaid ServicesExecutive SummaryIntroductionThe Bipartisan Budget Act of 2018 (BBA of 2018); Public Law 115-123, Section 50203(b)requires the Secretary of the Department of Health and Human Services (HHS) to develop a datacollection system to collect data on costs, revenue, and utilization, and other information deemedappropriate by the Secretary, from a representative sample of entities that furnish ground (i.e.,land and water) ambulance services. The BBA of 2018 specifies that the data collection systemapplies to Medicare ambulance “providers”—hospitals and other facilities that are Medicare“providers of service”—and Medicare ambulance “suppliers”—all other organizations that enrollin Medicare specifically to furnish and bill for ground ambulance services. The BBA of 2018further requires the Medicare Payment Advisory Commission (MedPAC) to use the collecteddata to assess the relationship between Medicare’s payment rates and the cost of providingground ambulance services.The Center for Medicare and Medicaid Services (CMS) commissioned support from the CMSAlliance for Modernizing Health Care Federally Funded Research and Development Center (theHealth FFRDC) in developing the data collection instrument and sampling plan to meet theserequirements. This report summarizes the Health FFRDC’s work under this effort, including: An overview of the ground ambulance industry (Chapter 2) A summary and comparison of existing tools to collect information related to groundambulance costs, revenue, and volume (Chapter 3) Findings from discussions with ground ambulance providers and suppliers (collectively,“ground ambulance organizations” 1) and industry groups (Chapter 4) Analysis of ground ambulance organization characteristics and Medicare groundambulance service volume and mix using available Medicare data (Chapter 5)The final chapters of the report present the Health FFRDC’s recommendations to CMS regardingthe development of a sampling plan (Chapter 6) and an instrument to collect data (Chapter 7) tomeet the requirements specified in the BBA of 2018. We include a data collection instrumentconsistent with our design recommendations in an appendix to this report (Appendix E).The findings in Chapters 2 through 5 describe our work to arrive at our recommendations andoffer support for specific recommendations. Readers primarily interested in the Health FFRDC’srecommendations are directed to Chapters 6 and 7 and the instrument in Appendix E.Ground Ambulance Services in MedicareMedicare covers medically necessary ground ambulance services meeting certain conditions. 2These services are provided by a diverse set of organizations enrolled in Medicare as providersor suppliers, including fire departments, hospitals, stand-alone government agencies, non-profit1Air ambulance organizations and services are out of scope for both CMS’s ground ambulance data collectionsystem and for this report.2 In addition to medical necessity, Medicare requires that (a) transports are to the nearest appropriate facility giventhe patient’s condition, and (b) all other forms of transportation are contraindicated.Medicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.v
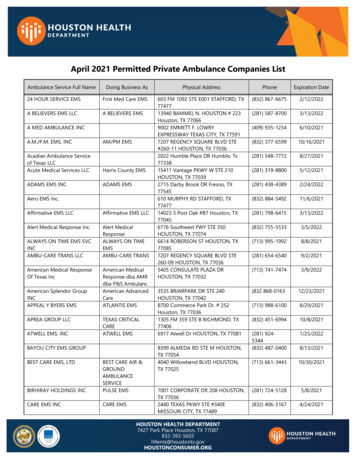
Centers for Medicare & Medicaid Servicesorganizations, and private for-profit companies. While most Medicare transports are covered bythe Medicare Part B medical benefit, transports involving inpatients at a hospital or other facilityfall under the Part A hospital benefit.Medicare pays ambulance organizations 3 for Part B-covered transports using the Ambulance FeeSchedule (AFS). The AFS establishes a base rate that varies by the level of transport provided(e.g., basic life support vs. advanced life support). The AFS also includes a per-mile rate appliedto the distance traveled with the patient. The AFS incorporates a permanent add-on payment of a50 percent increase in the standard mileage rate for ground ambulance transports that originate inrural areas where the travel distance is between 1 and 17 miles. Both base and mileage paymentsare only made when a patient is transported—in other words, Medicare does not pay forambulance responses to calls for service that do not result in a patient transport.Since the inception of the AFS in 2002, the base and mileage payment rates have been modifiedby three temporary “add-on” payments that are higher for transports originating in rural areas.These add-ons have been extended several times, most recently by the BBA of 2018.Challenges in Comparing Payment Rates to CostsAssessing how Medicare payment rates are related to costs is complicated by the significantvariation in ambulance organizations and by differences in how ambulance services are deliveredand financed across communities. Ambulance organizations vary in the mix of services theyprovide, including the share of responses resulting in transport, the blend of emergency and nonemergency transports, and, even within emergency and non-emergency transport categories, thelevel of transport. 4 Different types of services require different capabilities and inputs andtherefore contribute differentially to organizations’ costs. Furthermore, many ambulanceorganizations share personnel, facilities, and vehicles with other services such as firedepartments or hospitals. Determining the specific share of costs that should be allocated to theirambulance services for the purposes of comparing payments to costs is challenging.Furthermore, manyambulance organizations receive significant revenue from communities tosupport emergency medical services (EMS) systems with varying capabilities. It is not clear howMedicare and other healthcare payers’ rates should align with costs in this case. Neither is itclear whether payments should cover the total costs involved in furnishing ambulance services,including the costs of responses that do not result in billable transports, or only the costsassociated with patient transports.3The BBA of 2018 and this report focus on ground ambulance organizations and ground ambulance services (asopposed to air ambulance organizations and air ambulance services). Air ambulance organizations and servicesare out of scope for this report. For the remainder of the Executive Summary, we use “ambulance organization”and “ambulance service” to refer to “ground ambulance organization” and “ground ambulance service,”respectively.4 Transports are provided and billed to Medicare as either Advanced Life Support (ALS) or Basic Life Support (BLS)based on the staff and resources involved in the response. There is further differentiation in the AFS betweenlevels of ALS transports, Specialty Care transport, and Paramedic Intercept, which is an ALS level of service thatCMS defines as: a rural area transport furnished by a volunteer ambulance company which is prohibited by statelaw from billing third party payers where services are provided by an entity that is under contract with thevolunteer ambulance company that does not provide the transport but is paid for their paramedic interceptservice. (State of NY only meets these requirements).Medicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.vi
Centers for Medicare & Medicaid ServicesLittle data exists to evaluate the relationship between Medicare payments and the costs borne byambulance organizations, and the data that does exist is limited to certain types of ambulanceorganizations. A 2012 report by the Government Accountability Office (GAO) measuredambulance costs per transport relative to Medicare payments using survey data, but this data waslimited in sample size and only included ambulance services that were not delivered byorganizations based at hospitals or fire departments. 5 The CMS Healthcare Cost ReportInformation System (HCRIS) contains information on overall hospital costs, including datarelated to ambulance services, but this data is only available for ambulance services that areowned and operated by hospitals and other healthcare institutions. A 2015 U.S. Department ofHealth and Human Services (HHS) report addressing the extent to which cost reporting dataaccessed via HCRIS could be used for comparisons to Medicare payment rates was thereforelimited to ambulance providers. 6 The data collection required by the BBA of 2018 will fill thesegap by assembling timely and comprehensive information on ambulance costs, revenue, andservices from a representative sample of all ambulance organizations.Key AssumptionsWe assumed that the use of “cost” in the BBA of 2018 referred primarily to accounting costs,including operating and capital costs. We also assumed that the intent of the data collectionsystem required by the BBA of 2018 was to capture an organization’s total ground ambulancecosts and revenue rather than the share of costs and revenue associated with providing services toMedicare beneficiaries.Through initial discussions with CMS, the Health FFRDC focused on developingrecommendations for a survey-based instrument. Together with CMS, we considered otherformats for data collection, including Medicare cost reporting. 7 Survey instruments allow moreflexibility than cost reporting, which, in the context of diverse ambulance organizations, iscritical. Furthermore, cost reporting typically requires significant accounting and data systemsand expertise that not all ambulance organizations currently have in place.While we describe the data collection instrument as a survey, there are three key characteristicsof the instrument described in this report that differentiate the instrument from some otherprovider and supplier surveys. First, the instrument requests detailed financial information,similar to what would be collected via a Medicare Cost Report. Second, CMS intends to allowsampled ambulance organizations a full year to collect the requested information prior toreporting. Third, a 10 percent reduction to Medicare payments for a period of one year will beapplied for failure to report the required information under the ground ambulance data collectionsystem.The Health FFRDC made several additional assumptions in consultation with CMS on aspects ofthe broader ambulance data collection system and process (as opposed to the instrument and5GAO (2012) “Ambulance Providers: Costs and Medicare Margins Varied Widely; Transports of Beneficiaries HaveIncreased.”6 "HHS (2015) “Report to Congress Evaluations of Hospitals’ Ambulance Data on Medicare Cost Reports andFeasibility of Obtaining Cost Data from All Ambulance Providers and Suppliers."7 Medicare providers, including hospitals, are required to report financial information annually as part of costreporting. Cost reporting is a requirement for participation in the Medicare program. Information submitted viacost reports is used for a variety of purposes including updating prospective payment rates.Medicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.vii
Centers for Medicare & Medicaid Servicessampling plan more narrowly, which are the focus of this report), particularly related to timing.For example, we assumed that CMS will allow sampled ambulance organizations a full year tocollect the requested data prior to reporting. If ambulance organizations are sampled in late 2019,we assume they would collect data through 2020 and report data in early 2021. This processwould repeat for a minimum of three additional years of data collection. This timeline providesat least one and possibly two full years of collected data for analysis before MedPAC’s report isdue to Congress not later than March 15, 2023. These details regarding timing were not finalizedwhen we developed our recommendations and may change. CMS’s final decisions regarding thedata collection system, including the timing of data collection, will be made through therulemaking process that will occur over the summer of 2019. Finally, we assume that theinstrument will be programmed and fielded to facilitate sophisticated functionality in terms ofskip patterns and supplemental schedules.Aims Guiding the Sampling Plan and Instrument DevelopmentOur recommendations for the design of the sampling plan and instrument align with our aims to:1. Balance respondent burden against the need to collect the data required by the BBA of2018.2. Provide flexibility to collect data from diverse ambulance organizations.3. Enable the calculation of per-transport costs for comparison to Medicare payment rates.4. Leave open as many avenues for analysis as possible, for example comparisons of pertransport costs across subgroups of ambulance organizations and analyses estimating themarginal cost of a particular type of transport, while remaining consistent with the BBAof 2018 specifications for data collection and while balancing respondnet burden againstthe potential utility of collected data.With respect to the last two aims, we note that the BBA of 2018 does not specify the methods orapproach that MedPAC should use to compare reported costs and Medicare payment rates.Similarly, it is not clear how Congress might ultimately direct CMS to use the collected data. Weassume that MedPAC will, like the earlier analyses from GAO and HHS described above,calculate costs per transport. We also assume that MedPAC will explore methods to estimate thecost associated with individual Medicare ground ambulance services, for example models usingcurrent relative value unit (RVU) weights to calculate a per-RVU cost or regression modelsexpressing total costs as a function of observable characteristics of the ambulance organizationand information on service mix. We assume that MedPAC will combine the data reported via thedata collection system with Medicare fee-for-service claims data to further their analysis.Approach OverviewIn order to develop our recommendations to CMS, we conducted an initial literature review andenvironmental scan of the ambulance industry and past ambulance data collection efforts, soughtthe perspectives of ground ambulance organizations and industry groups, and analyzed availableMedicare data relevant to ambulance organizations and services. Specifically, we: Reviewed peer-reviewed literature, government and association reports, andexisting ambulance data collection tools to collect information on costs and revenues ofMedicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.viii
Centers for Medicare & Medicaid Services ambulance organizations and to identify background information regarding the variabilityamong ambulance organizations, state and local requirements that may impact the costsof providing ambulance services, and financial challenges facing amublanceorganizations. We summarized and compared five previously developed ambulance datacollection tools, including a mix of surveys and cost report-based tools developed andfielded by different organizations.Collected information from ground ambulance organization key informants andindustry groups through discussions to identify key ambulance organizationcharacteristics, identify cost and revenue components, and understand differences in thesecomponents across types of ambulance organizations. These discussions providedvaluable information on the process for collecting data, including how best to elicit validresponses, how to limit burden on respondents, and the extent to which the required datais already collected by ambulance organizations. Conducted a small number of cognitive interviews after developing a draft instrumentto assess respondents’ understanding of instructions, definitions, and draft questions andto assess whether information required to complete the instrument is readily available. Analyzed Medicare claims and enrollment data, including all fee-for-service Medicareclaims with 2016 service dates for ambulance services and the enrollment data for theground ambulance organizations that billed for these services. We calculatedorganization-level ambulance service Medicare volume and payments and explored howavailable Medicare data can be used to describe and categorize ambulance organizations.We relied on the inputs from these channels to inform the development of our finalrecommendations on the sampling plan and instrument design (including the design of theinstrument itself).Key Findings from Initial ResearchThe literature review and environmental scan, key informant discussions and other stakeholderengagement, and analyses of Medicare data yielded important information that informed ourrecommendations for the data collection instrument and sampling plan. Our findings from thisinitial research are summarized below and presented in more detail in Chapters 2 through 5.Ambulance Organizations and Other StakeholdersAmbulance organizations operate within the context of the broader healthcare system and labormarket, which necessarily involves many interconnected stakeholder groups, including publicand private insurance payers, government at various levels, individuals and communities, paidand volunteer labor, and vendors (e.g., drug and medical supply manufacturers and wholesalers).There are some commonalities in the relationships between ambulance organizations and otherstakeholders groups. For example, most ambulance organizations bill Medicare and otherhealthcare payers for services. There are also, however, important differences, particularly withregard to the mix of paid and volunteer labor that ambulance organizations utilize to provideambulance services meeting federal, state, local, and other requirements.Ambulance organizations are diverse and vary considerably in size and organizational makeup,activities beyond ground ambulance transport (if any), approaches to respond to communities’Medicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.ix
Centers for Medicare & Medicaid Servicesdemands for services, and sources of revenue. Community expectations of service area, level ofservice, and response time vary and have important implications for their costs.Even with these variations, several key characteristics of ambulance organizations emerged fromthe literature review, key informant interviews, and other stakeholder engagement that are relatedto ground ambulance costs and revenue: Medicare provider versus supplier status Transport volume Service area population density Ownership (for-profit, government, or non-profit) Service mix Staffing models (e.g., use of volunteer labor) Response timesWe explore the first five of these characteristics in detail using available Medicare data inanalyses described below. We return to these characteristics in our sampling plan as a way toassess whether our recommendations will yield a representative sample.Ambulance Cost and Revenue FrameworksWe developed an initial hierarchical cost and revenue framework to help organize cost andrevenue components identified in our background research and to help ensure that all relevantcomponents were considered. We then identified, reviewed, and compared five existing toolsthat have been proposed or used to collect information related to ground ambulance costs andrevenue. We compared the information collected via these tools to the initial cost and revenueframework that we developed in order to revise and refine the framework.We organized both the initial and revised frameworks using these highest level domains, each ofwhich was comprised of multiple individual elements: Labor costs Facilities costs Vehicle costs Equipment and supply costs Miscellaneous costs RevenueAll the tools that we reviewed covered each of these higher level domains (e.g., labor costs,facilities, vehicles); however, no single tool covered all cost elements at the more detailed levelin our framework (e.g., salaries of all labor categories, or breakdown of durable medicalequipment versus non-durable medical equipment). The five tools also differed in terms of theirinstructions, format, approach for handling allocation, and reporting time frame. We found thatnone of the five existing tools would collect all of the data needed to meet the requirements ofthe BBA of 2018.Medicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.x
Centers for Medicare & Medicaid ServicesDiscussions with StakeholdersOur individual and group-based discussions with stakeholders early in our study highlighted thesignificant variation in organizational structure, services provided, and personnel involved inproviding ambulance services. This variation is an important consideration in determining howinstructions and questions should be framed and the ease with which organizations may be ableto report certain data. Some ambulance organizations, for instance, use sophisticated groundambulance service, labor, and supply tracking systems. Other ambulance organizations may lackthese systems and not be able to answer questions as easily. Organizations vary in the reports andanalysis related to ground ambulance costs, revenue, and volume that they produce on a regularbasis. They also vary on whether existing data and analysis align with the calendar year ratherthan the organization’s fiscal year (when different than the calendar year).Our discussions with stakeholders highlighted the need to tailor instrument instructions andquestions to particular circumstances, including: Organizations relying primarily or exclusively on volunteer labor Organizations with fire response, police response, air ambulance services, or otheractivities and responsibilities in addition to ground ambulance operations Organizations that rely on other entities to cover certain costs such as benefits, rent, orsupplies Broad parent organizations (such as large corporations) billing for ground ambulanceservices under different subsidiary organizationsLater in our study, we used a small number of cognitive interviews with ambulanceorganizations to elicit feedback on draft instrument items and instructions. These interviewshighlighted the complexity of the draft instrument, the need for explicit instructions anddefinitions that are clear to respondents of different types, and the burden involved in collectingand reporting the requested data. All interviewees indicated that they would be able to collectand report the data requested given sufficient time. We revised the instructions and items in therecommended data collection instrument based on the feedback we received through thecognitive interviews.Analyses of Medicare DataWe used 2016 Medicare claims and enrollment information to summarize Medicare volume andpayment for ground ambulance services and to describe how ambulance organizations vary onkey dimensions identified in our literature review and qualitative research: Medicare provider versus supplier status Ownership (for-profit, government, or non-profit) Medicare billed transport volume Service area population density Service mixIn terms of Medicare volume and payment, we found that in 2016 ambulance organizationsbilled Medicare for a total of 14.8 million Part B ground ambulance transports correspondingMedicare’s Ground Ambulance Data Collection System: Sampling and Instrument Considerations and Recommendations 2019 The MITRE Corporation. ALL RIGHTS RESERVED. Approved for Public Release: 19-0989. Distribution Unlimited.xi
Centers for Medicare & Medicaid Serviceswith 6.1 billion in Medicare fee-for-service payments. Approximately 40 percent of alltransports were non-emergency. The rate of non-emergency transports per beneficiary is morevariable across geography than the rate of emergency transports.In terms of ambulance organizations’ characteristics, only 6 percent of ambulance organizationswere providers, including critical access hospitals and other hospitals. We found that over half ofthe organizations operate primarily in urban areas and that nearly half are government owned.Transport volume is highly skewed. The bottom 50 percent of organizations in terms of volumeaccounted for just 3 percent of total Medicare billed transports. In comparison, the top 5 percentof organizations by volume accounted for 51 percent of total Medicare volume.There were important relationships between the characteristics. Government organizationstended to be smaller in terms of transport volume and were more likely to serve rural areas, whilefor-profit organizations tended to be larger and serve urban areas. We identified a subset oforganizations that specialize in non-emergency, scheduled transports, such as trips to dialysisfacilities. These organizations tended to be for-profit, operate in urban areas, and have hightransport volumes.We present CMS with two approaches to categorize ground ambulance organizations for thepurposes of sampling and analysis. The first is based on combinations of the first fourcharacteristics listed above, and the second is based on grouping ambulance suppliers via acluster analysis. The first approach results in 36 “cells” differentiating ambulance organizationsbased on their characteristics. Alternatively, the cluster analysis yielded nine groups ofambulance organizations. The nine groups do not differentiate organizations based on volumebut do differentiate between urban ground ambulance organizations providing primarilyemergency and non-emergency transports.Sampling and Instrument RecommendationsWe deve
and "ambulance service" to refer to "ground ambulance organization" and "ground ambulance service," respectively. 4 : Transports are provided and billed to Medicare as either Advanced Life Support (ALS) or Basic Life Support (BLS) based on the staff and resources involved in the response. There is further differentiation in the AFS .
![MOH STANDARDS FOR EMERGENCY AMBULANCE SERVICE (2017) [Updated 21 Nov 2018]](/img/51/emergencyambulancestandards.jpg)