Transcription
GE HealthcareCentricity Healthcare User GroupTurbocharge your Claims, Remits andEligibility ProcessMichael Rose, Senior Product Marketing ManagerOctober 2013
2013 General Electric Company – All rights reserved.This does not constitute a representation or warranty or documentation regarding the product orservice featured. All illustrations are provided as fictional examples only. Your product featuresand configuration may be different than those shown. Information contained herein isproprietary to GE. No part of this publication may be reproduced for any purpose without writtenpermission of GE.This information does not constitute legal, financial, coding, or regulatory advice in connectionwith your use of the product or service. Please consult your professional advisors for any suchadvice. Operation of GE Healthcare products should neither circumvent nor take precedence overrequired patient care, including human intervention of healthcare providers. GE Healthcareproducts and services do not code medical procedures. Accurate coding is the responsibility ofthe provider or billing professional.DESCRIPTIONS OF FUTURE FUNCTIONALITY REFLECT CURRENT PRODUCT DIRECTION, ARE FORINFORMATIONAL PURPOSES ONLY AND DO NOT CONSTITUTE A COMMITMENT TO PROVIDESPECIFIC FUNCTIONALITY. TIMING AND AVAILABILITY REMAIN AT GE’S DISCRETION AND ARESUBJECT TO CHANGE AND APPLICABLE REGULATORY CLEARANCE.* GE, the GE Monogram, Centricity and imagination at work are trademarks of General ElectricCompany.General Electric Company, by and through its GE Healthcare division.
Today’s discussion Learn best practices for claims, remits andeligibility Understand how your practice is performingand ways to make improvements Share knowledge with other users
AgendaWho are we?What kind of relationship do we have withpayers?How we get data?Where do things go wrong?What can you do to improve?
Key Trends in the Industry
Key challenges facing practicesThere is no shortage of challenges in today’shealthcare landscape Healthcare reform, new mandates Reduced reimbursement, increase in selfpay Making the same billing mistakes over andover again
Average cost per claim for reworkSource: The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series (2009)
Industry average for claims that arerejected or deniedSource: OPTUMInsight 2012
Centricity EDIServicesA proven full serviceclearinghouse that streamlinesthe electronic schedule topayment workflow and deliversinsight for improving financialperformance
Centricity EDI ServicesProven, robust services 85BClaims billed annually2000Customers leverage EDIservices from GE Healthcare200MClaims processed annually byCentricity EDI Services
Centricity EDI Services /Auto ClaimStatusCentricity EDI Services is a full portfolioof critical electronic transactions andservices that helps drive ntAnalyticsDenial g
4 categories of stuff that goes wrong1. Missing claims2. Rejections3. Denials4. Missing remittance
Missing claimsWhat is 546,521?Number of claim files received by CentricityEDI in February 2012
The black hole 1% of Files 1% of FilesHealthcareOrganizationFile not sent toPayor in 4 hoursGECentricity EDIServicesClaims importedwithin 1 hrFile transferReport not receivedin 18 hoursClaims pendingafter 42 hoursTotal claims at risk:5-10%Claims not paidafter 35 daysPayer2% of Files2% of Files1-5% of Files
Missing claims by the numbersFebruary 2012 . 546,521 files submittedProblems come from . Connectivity Fail betweencustomer, clearinghouse orpayer 0.21% had a problem from Payer side problems (5010!)customer to clearinghouse 2.21% didn’t receive a filelevel acknowledgementwithin 18 hours 2.92% didn’t receive a claimlevel acknowledgementwithin 42 hoursPayers say Be sure you getaccept msg Weekly checkin is bestpractice
RejectionsWhat is 48,800?Average number of claims rejected on everybusiness day in February 2012
Top reasons for rejections 5.78% of claims were rejected inFebruary 2012! 922,394,798 REJECTED andneeded correctionPayers say Send 5010 correctly Enrollment shouldhappen early Train coders
Other rejection best practices Have a well defined credentialing process;monthly reviews Know your rejections; practices always makethe same mistakes Practice Registration best practices;capturing data and checking eligibility Continuous improvements in codingpractices
Denials andHosted ClaimsManager
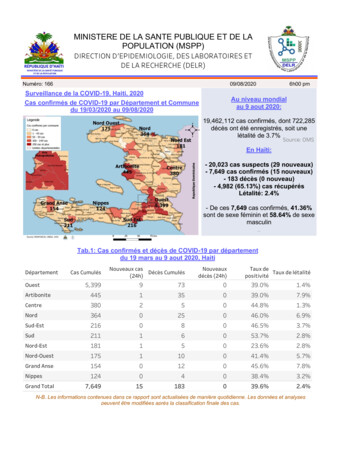
DenialsWhat is 18.3%?Percentage of DENIED claims in February2012
Top reasons for denials Denial are a more complexproblem than rejectionsThere are 4 most commonclinical denial reasonsPayers say Check eligibilityto eliminatethese type ofdenials forcoders Know the topdenial reasons
Top clinical denial reasons1. Duplicate Claim: one or more claims that have identicalDates of Services, Procedures, Modifiers, Departments, andProviders (including previous claim history)2. Global Follow-up Period: an E&M that was billed during theglobal follow up period of an earlier procedure, has the sameprimary Dx as on Dx for the earlier procedure and wasperformed by the same Provider2. Medical Necessity: no diagnosis on the claim line supportsmedical necessity for the procedure billed (as specified byLocal Medicare Guidelines)3. Modifier: a line item that contains a modifier that is notappropriate for use with a particular procedure code
Hosted ClaimsManagerHosted ClaimsManager is a pre-claim, clinical editing solution andproactive claim analysis service that helps identify and resolve postingerrors that would later result in a rejection or a denial. The best way toprevent rejections and denials is to stop them before they occur.
Hosted ClaimsManagerHosted ClaimsManager enablesyou to identify claims denialsprior to claim submission byutilizing an integrated GE hostedclaim scrubbing engine.Exceptional performance isenabled by denial insight coupledwith a team of revenue cyclespecialists who proactivelyidentify opportunities forimprovement.Hosted ClaimsManager – Back-end denial analysisWhy Hosted ClaimsManager: Exceptional workflow - integrated priorto claim submission Reduce denials and follow-up costs Customized high value supportexperience to drive performanceimprovements
Hosted ClaimsManager helpsIdentify charge entry errors, enabling theability to resolve potential rejections ordenialsComplete pre-claim edits prior tosubmissionProvides insight to claim data prior to yourcharge entry processProvide greater confidence that claims willget paid without disruption
Hosted ClaimsManagerOffers the ability to build comprehensive invoice history ofthe patient into the editing processNear real-time clinical editsCan trend the effectiveness of the edits and identify areas forcontinued process improvement – payment analysisIntegrates clinical edits with your PM workflow
Missing remittance filesWhat is the most common case we receive?Missing remittance files.
Top reasons for missing remit Delays on the payer productionof remittance filesProblems with the file that wereceive from the payer Crashes, but workable Need new files from payerPayers say Know whenyou expect tobe paid, takingholidays intoaccount Know the topdenial reasons
Payment Automation and Tracking
Payment Automation and Advanced PaymentTrackingPayment Automation enables a practice to achieve nearly 100% electronicposting of payment information. With Payment Automation, you are able toreceive, process and post third-party paper payments electronically withminimal manual effort, saving staff processing time and reducing delays anderrors.30GE Title or job number10/18/2013
Customer payment challenges Approximately 20-30% of payerpayments today are made frompaper EOBs 10% of practice costs are forpayment posting, hand postingand managing of payments* Lack of standardization ofdenials causes inefficiency andlack of follow-up31Centricity EDI Services10/18/2013
Steps of payment automationStep 1: ngFundsdeposit
Steps of payment automationStep 2: Data extractionSourceData ExtractionMail/EOBprocessingOCR “freeform”DocumentscanningData map& editingSourceFundsdeposit
Steps of payment automationStep 2: Data standardizationSourceData ExtractionDataStandardizationMail/EOBprocessingOCR “freeform”Claimsmatch &balancingDocumentscanningData map &editingDenial codetranslationSourceFundsdepositData to reconciliation
Adding advanced payment trackingMatch the claimand remittanceCreate a customerand payer specificprofile base onmonths of dataNotify you when aclaim is late orlikely missing
ample payer datadicaidBCBSicarenitedAetna0510Very Late15Late2025
ey takeawaysEDI Services can determinewhen a claim is very latemuch sooner thantraditional practicesPilot customer examples –simple steps to touch highdollar claimsIntegration plans with CPS,including Task Manager
Understanding Your Payers andPeers
mbursement Analyticsealthcare’s Reimbursement Analytics tool provides a detailedssment of a practice’s financial well being. Using a real-time, webd application, the Performance Intelligence service providesparative healthcare data on reimbursement, utilization anductivity.
eimbursement Analyticsrovides comparative healthcareata on reimbursement, utilizationnd productivityncludes over 100 fields in the ANSI35 (electronic remits) comparedt a state or national levelvailable for any size practice orealth system that employs ormanages outpatient providers,ubmits claims electronically andeceives electronic remitsvailable to Centricity PracticeManagement, Group Managementnd EDI Services Users
he value of informationGet answers to resolve keychallenges . And help improve theoutcomesReimbursementRevenue cycle efficienciesHow are payers treating us?How do we compare to ourpeers?UtilizationReimbursementAre we an outlier on a code thatmay be an “audit-trigger”? AreAnalyticswe coding appropriately?roductivityHow is our staff performingversus our peers?Correct incomplete or incorrectprior to submission.Reduce claim denials,underpayments and re-work.HostedClaimsClaims accuracyRelational editing for ICD and CPT.ManagerPayer-specific claims checkingbefore submission.Regulatory complianceEvaluates claims against rules andinitiatives
eedback lthcareServiceProvided s andTrendingAppealProcessFinalReconciling
Best Practices
est practices checklist - weeklyReview weekly trend of rejected claims anddenialsConfirm that all claims have made it to theend of the process, and have appropriateacknowledgements from payers
est practices checklist - monthlyMonthly reviews of rejections and denialsMake plans to resolve root causes; set goals andmeasurementsReview industry events like ICD-10 and EFT; keepup to date on any changes you might need toprepare forMonthly credentialing review
ummary – questions to askDo you know your overall rejection and denialrate by payer?Do you know the fraction that are “clinical”?Do you know the magnitude to the cash flowmpact?Do you have an improvement process in placeto reduce defects?
estimoniale've been using Centricity EDI Services with Centricity Practice Solutionce 2007, and Centricity EDI Services has helped make our entire revenuele process more efficient. We get paid faster and the workflowegration provides a streamlined workflow that requires less effort to getwork done. Most importantly, we get visibility into the status of ourms so that we can address potential issues in our revenue cycle beforere is a negative impact on revenue cycle performance."Nancy MedeirosSoftware AnalystSturdy MemorialAttleboro, MA
GE Healthcare doesn’t just providecustomers a method for conductingclearinghouse transactions Centricity EDI Services helpsyou produce cleaner claims,track the status of all claimsand accelerate remittanceand payments.
hank you for joining us.Questions
e've been using Centricity EDI Services with Centricity Practice Solution ce 2007, and Centricity EDI Services has helped make our entire revenue le process more efficient. We get paid faster and the workflow egration provides a streamlined workflow that requires less effort to get work done.