Transcription
CE: M.S.; ANNSURG-D-16-02083; Total nos of Pages: 8;ANNSURG-D-16-02083ORIGINAL ARTICLEReducing Length of Stay Using a Robotic-assisted Approach forRetromuscular Ventral Hernia RepairA Comparative Analysis From the Americas Hernia Society Quality CollaborativeAlfredo M. Carbonell, DO, Jeremy A. Warren, MD, Ajita S. Prabhu, MD,y Conrad D. Ballecer, MD,zRandy J. Janczyk, MD,§ Javier Herrera, MD,ô Li-Ching Huang, PhD,jj Sharon Phillips, MSPH,jjMichael J. Rosen, MD,y and Benjamin K. Poulose, MD, MPH Objective: The aim of this study was to compare length of stay (LOS) afterrobotic-assisted and open retromuscular ventral hernia repair (RVHR).Background: RVHR has traditionally been performed by open techniques.Robotic-assisted surgery enables surgeons to perform minimally invasiveRVHR, but with unknown benefit. Using real-world evidence, this studycompared LOS after open (o-RVHR) and robotic-assisted (r-RVHR) approach.Methods: Multi-institutional data from patients undergoing elective RVHRin the Americas Hernia Society Quality Collaborative between 2013 and 2016were analyzed. Propensity score matching was used to compare median LOSbetween o-RVHR and r-RVHR groups. This work was supported by anunrestricted grant from Intuitive Surgical, and all clinical authors havedeclared direct or indirect relationships with Intuitive Surgical.Results: In all, 333 patients met inclusion criteria for a 2:1 match performedon 111 r-RVHR patients using propensity scores, with 222 o-RVHR patientshaving similar characteristics as the robotic-assisted group. Median From the Department of Surgery, Division of Minimal Access and BariatricSurgery, Greenville Health System, University of South Carolina School ofMedicine, Greenville, SC; yDepartment of General Surgery, Cleveland ClinicComprehensive Hernia Center, Cleveland Clinic Main Campus, Cleveland,OH; zDepartment of General Surgery, Center for Minimally Invasive andRobotic Surgery, Abrazo Arrowhead Hospital, Glendale, AZ; §Department ofSurgery, Oakland University/William Beaumont School of Medicine, WilliamBeaumont Hospital, Royal Oak, MI; ôDepartment of General Surgery,North Florida Surgeons, St. Vincent’s Medical Center, Jacksonville, FL;jjDepartment of Biostatistics, Vanderbilt University Medical Center, 571Preston Building, Nashville, TN; and Department of Surgery, Division ofGeneral Surgery, Vanderbilt University Medical Center, Nashville, TN.Funding: This work was supported by an unrestricted grant from Intuitive Surgical.The Americas Hernia Society Quality Collaborative Foundation is supportedby Bard-Davol, Acelity-LifeCell, Intuitive Surgical, Medtronic, and W.L.Gore. The Americas Hernia Society (AHS, parent organization of the AHSQC)has received payment from Intuitive Surgical for exhibitor space at the AHSannual meeting.Conflicts of interest: A.C., DO, has received honoraria from Intuitive Surgical,Maquet Surgical, and W.L. Gore. J.W., MD, has received honoraria fromIntuitive Surgical, Maquet Surgical, and W.L. Gore. A.P., MD, has receivedhonoraria from Bard-Davol, Medtronic, and Cooper Surgical, and researchgrants from Miromatrix, and Intuitive Surgical. C.B., MD, has receivedhonoraria from Intuitive Surgical, Cook Surgical, and Ethicon. R.J., MD,has received honoraria and educational funds from Intuitive Surgical. J.H.,MD, has received honoraria from Intuitive Surgical. M.R., MD, has receivedhonoraria from Bard-Davol and W.L. Gore, and has received research grantsfrom Miromatrix; he has received educational funds from Intuitive Surgical; heis on the Board of Ariste Medical and receives salary from the AHSQC asMedical Director of AHSQC B.P., MD, MPH, has received research supportfrom Bard-Davol, and served as a consultant for Pfizer and Ariste Medical; hereceives salary from the AHSQC as the AHSQC Director for Quality andOutcomes.Reprints: Benjamin K. Poulose, MD, MPH, Vanderbilt University Medical Center,D-5203 Medical Center North, 1161 21st Avenue South, Nashville, TN 37232.E-mail: benjamin.poulose@vanderbilt.edu.Copyright ß 2017 Wolters Kluwer Health, Inc. All rights reserved.ISSN: 0003-4932/16/XXXX-0001DOI: 10.1097/SLA.0000000000002244Annals of Surgery Volume XX, Number XX, Month 2017LOS [interquartile range (IQR)] was significantly decreased for r-RVHRpatients [2 days (IQR 2)] compared with o-RVHR patients [3 days (IQR 3),P 0.001]. No differences in 30-day readmissions or surgical site infectionswere observed. Higher surgical site occurrences were noted with r-RVHR,consisting mostly of seromas not requiring intervention.Conclusions: Using real-world evidence, a robotic-assisted approach toRVHR offers the clinical benefit of reduced postoperative LOS. Ongoingmonitoring of this technique should be employed through continuous qualityimprovement to determine the long-term effect on hernia recurrence, complications, patient satisfaction, and overall cost.Keywords: AHSQC, Americas Hernia Society Quality Collaborative, hernia,length of stay, outcomes, retromuscular, robotic, surgery, ventral(Ann Surg 2017;xx:xxx–xxx)Ventral hernia repair remains 1 of the most common proceduresperformed by general surgeons. Despite the prevalence, there islittle agreement on appropriate operative techniques or ideal outcomemeasures for patients with ventral hernias. There is considerablevariability in costs and outcomes when performing ventral herniarepairs. Subsequently, it can be challenging to determine the valueadded to patients and hospital systems for specific hernia operations.When new and potentially innovative medical devices are introducedfor ventral hernia repair, there is usually additional variability in cost.Given the changing healthcare landscape and the drive towardsvalue-based care, it is important that any additional cost added tothe system demonstrates some objective benefit in terms of reducingoverall costs or improving patient outcomes. One such example is therobotic-assisted surgical platform, which is currently seeing rapidadoption by general surgeons for hernia repair. This value-basedassessment has led our group to examine the value added to herniarepairs with the utilization of the robot for performing retromuscularventral hernia repairs (RVHRs).There has been a recent trend in hernia surgery to reconstructabdominal wall defects by bringing the fascial edges to their normalanatomic position, utilizing a retromuscular approach while avoidingexcessive subcutaneous dissection.1–3 These techniques when performed through an open approach can result in significant patientmorbidity, including wound infections, postoperative pain, andextended length of stay (LOS).4 Several innovative surgeons haverecently begun to evaluate the role of the robot in retromuscularrepairs.5 These investigators have replicated the open RVHR(o-RVHR) using robotic assistance (r-RVHR) to allow the prostheticto be placed in the retromuscular position, with formal reconstructionof the linea alba, as performed in a classic open approach. However,the robotic-assisted platform adds potential cost to the systemthrough capital expenditures in the robot itself, and the expenseof the instruments required to perform the procedure. Given thesewww.annalsofsurgery.com 1Copyright 2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
CE: M.S.; ANNSURG-D-16-02083; Total nos of Pages: 8;ANNSURG-D-16-02083Annals of Surgery Volume XX, Number XX, Month 2017Carbonell et alissues, we felt it was critical to evaluate the potential advantage ofutilizing the robotic-assisted platform in performing RVHR versusthe standard open approach in terms of clinical outcomes that arerelevant to a patients and hospital systems. The objective of this studywas to evaluate the impact of r-RVHR on postoperative LOScompared with o-RVHR using real-world data from the AmericasHernia Society Quality Collaborative (AHSQC).METHODSDesign OverviewThe goal of this study was to evaluate postoperative LOS afterr-RVHR and o-RVHR using AHSQC data; we hypothesized thatmedian LOS after r-RVHR was less than o-RVHR. To adjust forconfounding factors impacting LOS, a propensity score matchingalgorithm was used to create 2 similar groups. Performance of thisstudy conformed to Strengthening the Reporting of ObservationalStudies in Epidemiology (STROBE) guidelines for cohort studies.6Data SourceData for this analysis were obtained from the AHSQC, amulti-institutional national quality and value improvement effortfocused on hernia disease. The AHSQC is comprised of 181 surgeonspracticing at 219 hospitals. AHSQC data are characterized bypredetermined standard definitions for the preoperative, operative,and postoperative phases of hernia care. Details regarding theAHSQC and its data assurance process have been previously published.7 The information collected is available to all hospitals andsurgical teams in the AHSQC on a real-time basis for qualityimprovement. For this analysis, a retrospective review of prospectively collected data was performed using AHSQC data between2013 and 2016. The analysis of this information for research wasapproved by the AHSQC Data Coordination Center (VanderbiltUniversity Medical Center) Human Research Protection Programand completed in cooperation with the AHSQC Foundation.PopulationAll patients undergoing elective, RVHR with mesh underCenters for Disease Control (CDC) and Prevention wound class 1(clean), class 2 (clean-contaminated), or class 3 (contaminated)conditions were eligible for analysis. RVHR in the AHSQC wasdefined as separation of the posterior sheath of the rectus muscle withplacement of mesh behind the muscle and anterior to the reapproximated posterior rectus sheath; preperitoneal mesh extension wasallowed [usually via transversus abdominis release (TAR)]. Patientsundergoing concomitant procedures or parastomal hernia repair wereexcluded. Patients were identified using standardized AHSQC variables corresponding to these criteria.the difference in days between the patient’s discharge date afterrepair and the patient’s date of operation.Secondary outcome measures included perioperative complications, reoperations, and readmissions that occurred within the30-day postoperative time period. Wound events were divided intosurgical site infection (SSI), surgical site occurrence (SSO), andsurgical site occurrence requiring procedural intervention (SSOPI).SSI was defined as a superficial, deep, or organ space infection. SSOincluded any SSI, and also wound cellulitis, nonhealing incisionalwound, fascial disruption, skin or soft tissue ischemia, skin or softtissue necrosis, wound serous or purulent drainage, stitch abscess,seroma, hematoma, infected or exposed mesh, or development of anenterocutaneous fistula. SSOPI was defined as any SSO that requiredopening of the wound, wound debridement, suture excision, percutaneous drainage, or mesh removal (partial or complete).Propensity Score Matching AlgorithmTo identify comparable groups for analysis regarding preoperative comorbidities and operative technique, a propensity scorebased matching algorithm was used. A logistic regression model wasused to estimate the propensity score for each patient, defined as theprobability of undergoing r-RVHR conditional on selected covariates. These covariates included those having a high likelihood ofimpacting LOS after operation including body mass index, VentralHernia Working Group classification,10 CDC wound class, AmericanSociety of Anesthesiologists class, epidural analgesia, presence ofdiabetes, sex, age, smoking status, hernia width, use of TAR, herniatype (primary vs acquired), and repair of recurrent hernia. A nearestneighbor matching method was used to identify the best o-RVHRcontrol matches for each individual r-RVHR patient.Power, Sample Size, and Statistical AnalysisTo estimate sample size, we assumed a 2:1 ratio of o-RVHRpatients to r-RVHR patients, based on available patients undergoingRVHR in the AHSQC. We conservatively estimated a difference of 2days in LOS between groups based on previous work, with standarddeviation of 5 days.5,11 If the true difference between groups is 2days, this study needed a minimum of 100 r-RVHR patients and 200o-RVHR patients to reject the null hypothesis that the LOS is equalwith power of 90%. After propensity score matching, hypothesistesting was performed using Wilcoxon rank-sum test for LOS andcontinuous variables. Pearson chi-square analysis or Fisher exact testwas used for categorical variables. A 2-tailed P value less than 0.05was considered significant. The performance of the propensity scorematched comparison was assessed by comparing propensity scoredistributions and by evaluating homogeneity across propensity scorequartiles for the primary outcome measure.12RESULTSComparison GroupsOf the total number of eligible patients, those identified asundergoing open operations were included in the o-RVHR group,whereas patients undergoing robotic-assisted procedures using the daVinci Surgical System (Intuitive Surgical, Inc.) were included in ther-RHVR group. Patients undergoing purely laparoscopic procedureswere excluded, as were patients undergoing planned ‘‘hybrid’’repairs using both open and minimally invasive techniques. Roboticcases converted to an o-RVHR were included in the r-RVHR groupusing an intent-to-treat approach. The techniques used for each of thesurgical approaches have been previously described.5,8,9Outcome MeasuresThe primary outcome measure for this study was postoperative LOS after elective RVHR. This was determined by calculating2 www.annalsofsurgery.comOf the 5602 AHSQC patients, 1250 met inclusion and exclusion criteria. Forty-five of these patients were not included in thematching algorithm due to 14 patients with missing LOS and 31patients with at least 1 missing value for a matching variable. Theresulting 1205 patients were used for the propensity score match,with 111 r-RVHR matched to 222 o-RVHR patients. Four r-RVHRpatients required conversion to o-RVHR repair and were included inthe r-RVHR group for analysis. The o-RVHR operations wereperformed by 39 surgeons in the AHSQC (28% private practice,72% academic practice). For r-RVHR, 14 surgeons performed theprocedures (36% private practice, 64% academic practice). The 2patient groups were similar in terms of demographics, comorbidities,and clinical characteristics (Table 1). A higher proportion of o-RVHRpatients underwent regional block analgesia and had a history ofß2017 Wolters Kluwer Health, Inc. All rights reserved.Copyright 2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
CE: M.S.; ANNSURG-D-16-02083; Total nos of Pages: 8;ANNSURG-D-16-02083Annals of Surgery Volume XX, Number XX, Month 2017Robotic-assisted Retromuscular Hernia RepairTABLE 1. Preoperative and Operative Characteristics of Open (o-RVHR) and Robotic-assisted (r-RVHR) Retromuscular VentralHernia Repair PatientsDemographicsAge, yrs (mean standard deviation)Women, %Non-White, %Body mass index, kg/m2 (mean standard deviation)ComorbiditiesCurrent nicotine use, %Diabetes, %COPD, %Hypertension, %Dyspnea, %Dialysis, %History of abdominal wall infection, %History of abdominal aortic aneurysmRecurrent ventral hernia, %Current steroid use, %Inflammatory bowel disease, %Crohn disease, %Ventral Hernia Working Group hernia grade123Modified hernia grade123ASA class1234Clinical characteristicsIncisional hernia, %Primary ventral hernia, %Epidural analgesia used, %Regional block analgesia used, %Hernia width, cm (mean standard deviation)Categorized hernia width, %Width 4 cmWidth 4 cm and 10 cmWidth 10 cmHernia length, cm (mean standard deviation)Categorized hernia length, %Length 8 cmLength 8 cm and 15 cmLength 15 cmHernia area, cm2 (mean standard deviation) Operative detailsCenters for Disease Control wound class, %Class 1 (clean)Class 2 (clean-contaminated)Class 3 (contaminated)Operative time, %0–59 min60–119 min120–179 min180–239 min240þ minMesh used, %Mesh placement, %RetromuscularRetromuscular and preperitonealMesh type, %Uncoated permanent syntheticAbsorbable barrier composite permanent syntheticUncoated absorbable syntheticß2017 Wolters Kluwer Health, Inc. All rights reserved.o-RVHR (n ¼ 222)r-RVHR (n ¼ 111)P55.08 13.7657%18%33.23 7.3955.59 12.3661%14%33.88 1%2%37%60%1%95%5%5%32%7.17 3.6895%5%5%6%7.51 3.3413%62%25%12.00 6.8910%64%26%13.17 6.5831%32%37%80.13 74.0222%32%46%87.96 .31%8.11%95%5%0%0.910.70.70.7 0.0010.20.70.10.20.11 0.001 0.001 0.001www.annalsofsurgery.com 3Copyright 2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
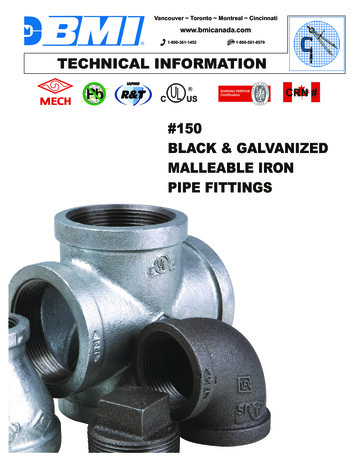
CE: M.S.; ANNSURG-D-16-02083; Total nos of Pages: 8;ANNSURG-D-16-02083Annals of Surgery Volume XX, Number XX, Month 2017Carbonell et alTABLE 1. (Continued)Combination of permanent and absorbableOther meshyFixation used, %Fixation type (% if fixation used)Sutures onlyTacks onlySutures and tacksOther fixationzTransversus abdominis release performed, %Drains used, %Fascial closure achieved, %Fascial closure suture type, %AbsorbablePermanentAbsorbable and permanentFascial closure suture technique, %RunningFigure of eightSimple interruptedRunning and simple interruptedo-RVHR (n ¼ 222)4.50%4.50%80%r-RVHR (n ¼ 2%7%1%67.57%31.53%0.90%85%11%3%1%98%0%1%1%P0.02 0.0010.7 0.0010.6 0.001 0.001 Hernia area calculated from hernia length and width using formula of an ellipse.yOther mesh types include biologic, biologic barrier composite permanent synthetic, preformed hernia system, permanent barrier composite permanent synthetic, and unknownmesh type.zOther fixation types include combinations of adhesives and sutures.Bold values signifies statistically significant.dyspnea versus r-RVHR patients. Patients undergoing o-RVHR hadshorter operative times, wider array of mesh products, more uniformuse of suture fixation, and a higher proportion of drain usagecompared with r-RVHR. Regarding fascial closure, r-RVHR patientshad higher use of permanent suture and running closure technique.multifactorial. Some explanations for this may include smallerincision size versus open operations, and also decreased tractionon the abdominal wall by retractors, and finally fixation of the meshusing retromuscular suture fixation instead of transfascial suturefixation. Additional investigation is to determine the reasons for theDISCUSSIONOur study reports the largest collective experience of r-RVHRto date. We found that the robotic-assisted approach resulted insignificant postoperative LOS reduction, which was both statisticallysignificant and clinically relevant. The shortened LOS in the roboticassisted group may be attributable to decreased pain, which may be4 www.annalsofsurgery.com3020Length of Stay (Days)Table 3 summarizes perioperative complications, reoperations, and readmissions within 30 days of RVHR. There were nodifferences in recognized intraoperative complications. A partialthickness bowel injury and gastric injury were observed in the rRVHR group, with 1 partial-thickness and 2 full-thickness bowelinjuries occurring in the o-RVHR group. One r-RVHR patientexperienced an unrecognized bowel injury requiring reoperation.No differences were observed for SSIs between the 2 groups. Ahigher proportion of r-RVHR patients experienced SSOs which weremostly seromas not requiring intervention. Reoperation rates, readmission rates, and rates of other complications were similar betweenthe groups.10Secondary Outcome Measures0The overall median LOS was significantly decreased for rRVHR patients [2 days; interquartile range (IQR) 2] compared witho-RVHR patients (3 days; IQR 3, P 0.001; Fig. 1). Figure 2 showsthe same comparison with outlier values removed (ie, values higherthan the third quartile value þ 1.5 the IQR). The propensity scorematched comparison for the primary outcome measure was homogenous across propensity score quartiles (Table 2), suggesting goodperformance of the propensity score matching algorithm.40Primary Outcome Measure: Length of Stayo RVHRr RVHRFIGURE 1. Length of stay (days) comparison after open (oRVHR) and robotic-assisted (r-RVHR) retromuscular ventralhernia repair; each box plot represents data from propensityscore matched groups (222 o-RVHR patients and 111 r-RVHRpatients). Box plots show the interquartile range (boxes),median, 1.5 the third quartile (upper whisker), minimumvalue (lower whisker), and outlier values (open circles)for length of stay values. Median length of stay is shown withP 0.001 between the 2 groups.ß2017 Wolters Kluwer Health, Inc. All rights reserved.Copyright 2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
CE: M.S.; ANNSURG-D-16-02083; Total nos of Pages: 8;ANNSURG-D-16-02083Annals of Surgery Volume XX, Number XX, Month 20174Length of Stay (Days)68Robotic-assisted Retromuscular Hernia RepairMedian 302Median 2o RVHRr RVHRFIGURE 2. Length of stay (days) comparison after open (oRVHR) and robotic-assisted (r-RVHR) retromuscular ventralhernia repair with outlier values removed (ie, values higherthan the third quartile value þ 1.5 the interquartile range);each box plot represents data from propensity score matchedgroups (222 o-RVHR patients and 111 r-RVHR patients). Boxplots show the interquartile range (boxes), median, 1.5 thethird quartile (upper whisker) and minimum value (lowerwhisker). Median length of stay is shown with P 0.001between the two groups.observed reduction in LOS with the robotic approach, especially interms of pain. Our study is the first to report a significant reduction inpostoperative LOS, while maintaining open operative principles andutilizing robotic assistance. Despite the added cost of the platform,this decrease in LOS demonstrates the possible value of roboticassisted hernia repairs to patients and hospital systems. Thesefindings should encourage further investigation of this platformfor ventral hernia repair regarding reduced postoperative pain,long-term recurrence, and overall cost.The o-RVHR approach with mesh reinforcement has emergedas an acceptable approach to the repair of incisional hernias. Specifically, TAR allows wide mesh overlap of larger hernia defects in theretrorectus and preperitoneal space lateral to the posterior rectussheath. This approach also offers a decrease in the wound morbiditytypically associated with external oblique release (EOR), whichrequires the creation of a large subcutaneous flap.3 Despitereductions in wound morbidity compared with open EOR, the ratesof wound events remain significant. In a recent retrospective reviewof o-RVHR, Cobb et al4 reported a 35.7% incidence of SSO and a15.6% incidence of SSI, including a 1.9% mesh explantation rate and14.9% hernia recurrence rate for CDC class I hernia repairs, themajority of which (97.4%) were in repairs with synthetic mesh asopposed to bioabsorbable or biologic meshes. Our series noted asubstantially lower rate of SSIs in o-RVHRs compared with theseresults. This difference could be due to the smaller and less complexdefects repaired in our series versus the Cobb et al experience.Despite that difference, we noted a higher rate of SSOs in our roboticassisted cohort. These SSOs were mostly due to a higher rate ofseroma formation. However, the number of surgical site occurrencesrequiring procedural intervention was similar between the 2 groups.This suggests that the seromas were not clinically significant andreflect the known issue with minimally invasive approaches toventral hernia as previously reported.13Evaluating variation in hospital costs related to various herniarepair techniques can be difficult as contract pricing and surgeonpractice varies significantly. However, there are some insights intocosts of repair that become important as robotic-assisted repairs areutilized. Prosthetic mesh choices can significantly impact the cost ofhernia operations. Even synthetic meshes, which are known to besubstantially less costly than biologic meshes, can result in dramatically different cost profiles. For instance, an intraperitoneal syntheticmesh with an antiadhesive barrier can cost several thousands ofdollars, depending on the size of the mesh, whereas a similarly sizeduncoated mesh may cost only several hundreds of dollars. Theuncoated sublay mesh, however, should only be placed outsidethe peritoneal cavity in the retromuscular or preperitoneal position.Historically, this could only be accomplished with an open approach.Our study shows that these inexpensive materials can be placed in theextraperitoneal retromuscular position using robotic assistance.Importantly, these differences in mesh costs could potentially offsetthe cost of the robotic disposable equipment. Likewise, a standardminimally invasive hernia repair with intraperitoneal mesh oftenrequires mechanical fixation. These devices can cost several hundreddollars each, and may be obviated with robotic-assisted hernia repair,as the mesh can be sutured. Whereas our study did not specificallyexamine costs associated with r-RVHR, the avoidance of expensivecovered meshes and mechanical fixation devices combined with theability to place the mesh in the retromuscular space while stillreproducing the open technique should be taken into account. Itremains to be seen if there is overall added value attributable to therobotic-assisted approach to ventral hernia repair versus the openapproach, in terms of decreased overall costs or overall improvedoutcomes. Clearly, the robotic-assisted procedure adds to operativetime, as more r-RVHRs took longer than 2 hours compared with oRVHR. The relationship of this finding to the robotic learning curveis unclear in our study, and likely increases cost. Undeniably,utilization of the robot adds disposable costs, specifically in termsof multiuse instruments and in some cases expensive barbed sutures.However, those costs may be offset by other considerations such asshorter LOS, earlier return to work, or decreased resources directedTABLE 2. Median Length of Stay After Open (o-RVHR) and Robotic-assisted (r-RVHR) Retromuscular Ventral Hernia Repair byPropensity Score Quartileo-RVHR (n ¼ 222)Median length of stay, d [interquartile range (IQR)]Propensity score 0.25Propensity score 0.25 to 0.5Propensity score 0.5 to 0.75Propensity score 0.754333(IQR(IQR(IQR(IQR3) (n ¼ 56)3) (n ¼ 56)2.5) (n ¼ 59)2.5) (n ¼ 51)r-RVHR (n ¼ 111)2211(IQR(IQR(IQR(IQR3) (n ¼ 28)2) (n ¼ 27)3) (n ¼ 24)1.25) (n ¼ 32)P0.00210.00410.0179 0.001Bold values signifies statistically significant.ß2017 Wolters Kluwer Health, Inc. All rights reserved.www.annalsofsurgery.com 5Copyright 2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
CE: M.S.; ANNSURG-D-16-02083; Total nos of Pages: 8;ANNSURG-D-16-02083Carbonell et alAnnals of Surgery Volume XX, Number XX, Month 2017TABLE 3. Intraoperative and 30-day Postoperative Complications of Open (o-RVHR) and Robotic-assisted (r-RVHR) Retromuscular Ventral Hernia Repair PatientsRecognized intraoperative complicationsTotal recognized intraoperative complications (n)Partial-thickness bowel injuryFull-thickness bowel injuryGastric injury30-d Postoperative complicationsSurgical site infection, %Surgical site infection type (n)SuperficialDeepOrgan spaceSurgical site occurrence, %Surgical site occurrence type (n) SeromaCellulitisHematomaNonhealing incision, skin necrosis, or ischemiaInfected seromaOther surgical site occurrenceSurgical site occurrence requiring procedural intervention, %Reoperations, %Reoperation reason (n)Bowel obstructionBleedingUnrecognized bowel injuryUnrelated intra-abdominal pathologyReadmissions, %Readmission reason (n)Wound complicationsGastrointestinal complicationsPainPain and thrombotic complicationsInterparietal herniaObstructing ureteral stoneShortness of breathOtheryPulmonary embolism (n)Urinary tract infection (n)Pneumonia (n)Reintubation (n)Death (n)o-RVHR (n ¼ 222)r-RVHR (n ¼ 111)P31202101110.60.34%2%0.571014%10132%0.410.2 0.0019626145%3%28130134%2% .6 Excluding surgical site infections.yOther unspecified readmission reasons exclusive of those listed.Bold values signifies statistically significant.towards pain management, making the cost analysis complex at best.Even a single-day reduction in LOS, as demonstrated in our study,can have a significant impact on costs.14 Further study related tothese outcomes and cost is necessary to determine if the 1-day LOSreduction is an important factor in cost analysis when utilizing therobot in RVHR.Based on the above noted factors, minimally invasive techniques for RVHR with mesh may be desirable due to reduced woundmorbidity, pain, and LOS. A pure laparoscopic approach to retromuscular hernia repair has also been described by 1 group.15 In thisstudy, the author describes the initial experience with laparoscopicTAR with fascial defect closure and reinforcement with mesh in 3patients. The average operative time was 329 minutes, with anaverage inpatient stay of 4.7 days, still twice that of our roboticassisted series. Whereas the relatively long operative time wasattributed to the learning curve, the average LOS was reported as1 day less than open cases at the same institution. There was no6 www.annalsofsurgery.comreported morbidity or mortality at 30 days, nor were there woundcomplications during 6 weeks of follow-up. The defect sizes were notreported, nor were the number of recurrent hernias. Whereas this maysuggest that laparoscopic TAR is feasible, it is likely too early tomake generalizable conclusions about the appropria
From the Department of Surgery, Division of Minimal Access and Bariatric Surgery, Greenville Health System, University of South Carolina School of Medicine, Greenville, SC; yDepartment of General Surgery, Cleveland Clinic . Beaumont Hospital, Royal Oak, MI; Department of General Surgery, North Florida Surgeons, St. Vincent's Medical Center .