Transcription
April 2022Eligibility OverviewWashington Apple Health (Medicaid) ProgramsHCA 22-315 (3/18)
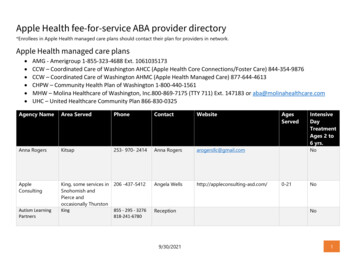
ContentsWhat is Washington Apple Health (Medicaid)? 2Medically Needy (MN) and Spenddown How to use this guide 2Medicare Savings Programs (MSP) Scope of care 3Modified Adjusted Gross Income (MAGI) Programs 3Qualified Medicare Beneficiary (QMB) (S03)Specified Low-Income Medicare Beneficiary(SLMB) (S05)Qualified Disabled Working Individual(QDWI) (S04)Adult Medical (N05)Family Medical (N01)Health Care Extension (N02)Pregnancy and Family PlanningPregnancy Medical (N03, N23)Medically Needy Pregnant Individuals (P99)Long-term services and supports (LTSS)and Hospice 11Covered services—scope of service 11Family Planning Extension (P05)Scope of service categoriesFamily Planning Only (P06)Table: Benefit packages by programApple Health for KidsOther services Apple Health for Newborns (N10):Apple Health for Kids with Premiums (N13, N33)Interpreter Services for Sign and SpokenLanguageApple Health for Medically Needy Kids (F99)6Where to apply for health care coverage Breast and Cervical Cancer Treatment Program(BCCTP) (S30)MAGI ProgramsFoster Care/Adoption Support/Former Foster Care(D01, D02, D26)Long-term CareMedical Care Services (A01, A05)7Alien Emergency Medical (AEM) (K03, N21, N25,S07)State-funded long-term care services (L04, L24)14Classic Medicaid ProgramsAged, Blind, Disabled CoverageResources Refugee (R02, R03)Supplemental Security Income (SSI)Related Programs 14Non-emergency Medical Transportation (brokeredtransport)Apple Health for Kids (N11, N31)Non-Citizen Program 10Qualified Individual (QI-1) (S06)AdultsClassic Medicaid Programs 915Apple Health Toll-free Customer Services(through the Health Care Authority)HCA Online ResourcesScope of Care WACsDefinitions 168SSI Program (S01)SSI-Related Program (S02)SSI-Related MN Program (S95, S99)Apple Health for Workers with Disabilities (HWD)(S08)1
What is Washington Apple Health (Medicaid)?Medicaid is the federally matched medical aid programsunder Title XIX of the Social Security Act (and TitleXXI of the Social Security Act for the Children’s HealthInsurance Plan) that covers the Categorically Needy (CN)and Medically Needy (MN) programs.Washington Apple Health is an umbrella term or“brand name” for all Washington State medicalassistance programs, including Medicaid. The brandname may be shortened to “Apple Health.”The Health Care Authority (HCA) administers mostWashington Apple Health programs. (The Departmentof Social and Health Services administers theSupplemental Security Income (SSI), SSI-related, Statefunded Medical Care Services (MCS), and MedicareSavings programs.)Medicaid expansion: Building on compassionThe Patient Protection and Affordable Care Act (ACA),enacted by Congress in 2010, created an unrivaledopportunity for increasing health coverage. Stateshad the option to expand eligibility for Medicaid andWashington State said yes.How to use this guideThis guide gives an overview of eligibilityrequirements for Washington Apple Health. It doesn’tinclude every requirement or consider every situationthat might arise. The explanation of Scope of Careon page 3 is helpful in understanding the differencesbetween the programs. Refer to the Definitions onpage 16 if you are not familiar with some of the termsused in this guide.Income levels, such as those based on Federal PovertyLevel (FPL) and Cost of Living Adjustments (COLA),and specific program standards change yearly, but indifferent months. Please understand that, while theinformation in this publication is current at the timeof publication, some of these standards will changebefore the next annual update. For the most currentinformation, go to the Health Care Authority websitehca.wa.gov/apple-health .2Before Medicaid expansion, coverage was essentiallylimited to low-income children, people withdisabilities or devastating illnesses, and those whoseincomes were far below the federal poverty level.Today, Apple Health covers adults with incomes up to138 percent of the federal poverty level. In April 2022that translated to about 18,754 for a single personor 38,295 for a family of four.Many low-income adults suffering from chronicconditions, such as diabetes, high blood pressure,asthma, and other diseases have better optionsthan waiting until they are sick enough to go to theemergency room. People living on the edgefinancially don’t have to choose between going tothe doctor and paying the electric bill. And peopleused to doing without are able to get regular doctorvisits, including preventive care.More people served todayThe number of people eligible for Apple Healthincreased significantly with higher income limits.Others who had previously qualified but not enrolledalso obtained coverage. By 2022, over 780,000enrollees were receiving Apple Health for Adultscoverage.
Scope of careScope of care describes which medical and healthcare services a particular Apple Health programcovers. There are four categories of scope of care: Categorically Needy (CN): The broadest, mostcomprehensive scope of health care services covered. Alternative Benefits Plan (ABP): The same scope ofcare as CN, with the addition of habilitative services,applicable to the Apple Health for Adults program. Medical Care Services (MCS): This scope of carecovers fewer health care services than MedicallyNeedy. MCS is a state-funded medical programavailable to adults who are not eligible for AppleHealth programs with CN, ABP, or MN scope of careand meet the eligibility criteria for either the Aged,Blind or Disabled–cash or the Housing EssentialNeeds (HEN) program. Medically Needy (MN): This scope of carecovers slightly fewer health care services thanCategorically Needy. Medically Needy coverage isavailable to individuals who qualify for disabilitybased Apple Health, Apple Health for LongTerm Care, or Apple Health for Kids or PregnantIndividuals, except that their income and/orresources are above the applicable Apple Healthprogram limits.Modified Adjusted Gross Income(MAGI) ProgramsAdultsAdult Medical (N05):Family Medical (N01):Effective April 1, 2022Effective April 1, 2022Household SizeMonthly Income LimitHousehold SizeMonthly Income Limit1 1,5071 5112 2,0302 6583 2,5533 8204 3,0764 9725 3,5995 1,1276 4,1226 1,284This program provides ABP coverage to adults withcountable income at or below 133 percent of the FPLwho are ages 19 up to 65, who are not incarcerated,and who are not entitled to Medicare.This program provides CN coverage to adultswith countable income at or below the applicableMedicaid standard and who have dependent childrenliving in their home who are under the age of 18.Health Care Extension (N02):This program provides CN coverage to individualswho lost eligibility for Family Medical because of anincrease in their earned income after they receivedFamily Medical coverage for at least 3 of the last 6months. These individuals are eligible for up to 12months extended CN medical benefits.3
Pregnancy and Family PlanningPregnancy Medical (N03, N23):Effective April 1, 2022Household SizeMonthly Income Limit1N/A2 2,9453 3,7044 4,4645 5,2236 5,982This program provides CN coverage to pregnantindividuals with countable income at or below 193percent of the FPL without regard to citizenship orimmigration status. Once enrolled in Apple Healthfor Pregnant Individuals, the individual is coveredregardless of any change in income through the endof the month after the 60th day after the pregnancyend date (e.g., pregnancy ends June 10, health carecoverage continues through August 31). Individualsreceive this post-partum coverage regardless of howthe pregnancy ends.Individuals who apply for Pregnancy Medical after thebaby’s birth may not receive postpartum coverage, butthey may qualify for help paying costs related to thebaby’s birth if they submit the application within threemonths after the month in which the child was born.To determine the pregnant individual’s family size,include the number of unborn children with thenumber of household members (e.g., an individualliving alone and pregnant with twins is considered athree-person household).4Medically Needy Pregnant Individuals (P99):This program provides MN coverage to pregnantindividuals with income above 193 percent of theFPL. Individuals who qualify are eligible for MNcoverage after incurring medical costs equal to theamount of the household income that is above the193 percent FPL standard.Family Planning Extension (P05):This program provides family planning servicesonly for 10 months after Pregnancy Medical ends.Individuals receive the Family Planning Extensionautomatically, regardless of how the pregnancy ends.Family Planning Only (P06):This program provides both men and womencoverage for pre-pregnancy family planning servicesto help participants take charge of their lives andprevent unintended pregnancies.Family Planning Only: Annual examination. Family planning education and risk reductioncounseling. FDA-approved contraceptive methods including:birth control pills, IUDs, and emergencycontraception. Over the counter contraceptive products, such ascondoms, and contraceptive creams and foams. Sterilization procedures.Clients access Family Planning Only services throughlocal family planning clinics that participate in theprogram.Find additional information at hca.wa.gov/familyplanning.
Apple Health for KidsApple Health for Kids coverage is free to children in households with income at or below 210 percent of the FPLand available for a monthly premium to children in households with income at or below 312 percent of the FPL.Effective April 1, 2022HouseholdSizeMonthly Income Limit210% FPL(No Cost)Monthly Income Limit260% FPL( 20 Premium/Child, 40 Family Maximum)Monthly Income Limit312% FPL( 30 Premium/Child, 60 Family Maximum)1 2,379 2,945 3,5342 3,205 3,968 4,7613 4,031 4,990 5,9884 4,857 6,013 7,2155 5,683 7,036 8,4436 6,509 8,058 9,670Apple Health for Newborns (N10):This program provides 12 months of CN coverage ifthe mother was enrolled in an Apple Health programwhen the child was born. There is no resource orincome limit for this program.Children who would have been eligible for AppleHealth for Kids with Premiums had they metimmigration status requirements receive CNcoverage under state-funded Apple Health for Kidswith Premiums.Apple Health for Kids (N11, N31):This program provides CN coverage to children underage 19 whose families have income at or below210 percent of the FPL. Children who would havebeen eligible for Apple Health for Kids had they metimmigration status requirements receive CN coverageunder state-funded Apple Health for Kids.Apple Health for Medically Needy Kids (F99):This program provides MN coverage to childrenunder age 19 whose families have income above312 percent of the FPL. Children who qualify and areenrolled in Apple Health for Medically Needy Kidsbecome eligible for MN coverage after incurringmedical costs equal to the amount of the householdincome that is above the 312 percent FPL standard.Apple Health for Kids with Premiums (N13, N33):This program provides CN coverage to childrenunder age 19 whose families have income above210 percent and at or below 312 percent of theFPL. Participants pay a low-cost monthly premium.5
Classic Medicaid ProgramsBreast and Cervical Cancer Treatment Program(BCCTP) (S30):This federally-funded program provides healthcare coverage for individuals diagnosed withbreast or cervical cancer or a related pre-cancerouscondition. Eligibility is determined by the Breast,Cervical, and Colon Health Program (BCCHP) in theWashington State Department of Health (DOH). DOHis responsible for screening and eligibility, whileHCA administers enrollment and provider payment.Coverage continues through the full course oftreatment as certified by the BCCHP.An individual is eligible if they meets all of thefollowing criteria: Screened for breast or cervical cancer under theBCCHP. Requires treatment for either breast or cervicalcancer or for a related pre-cancerous condition. Is under age 65. Is not covered for another CN (Categorically Needy)Apple Health program. Has no insurance or has insurance that is notcreditable coverage. Meets residency requirements. Meets social security number requirements. Meets citizenship or immigration statusrequirements. Meets income limits set by the BCCHP.For further information, go to the DOH ase/Cancer/BreastCervicalandColonHealth.aspxFoster Care/Adoption Support/Former Foster Care(D01, D02, D26):This program provides CN coverage to childrenreceiving foster care or adoption support services.This program also provides CN coverage toindividuals from the age of 18 up to 26 who age outof foster care in Washington State.6Medical Care Services (A01, A05, A24):This state-funded program provides limited healthcare coverage to adults who are not eligible for AppleHealth programs with CN, ABP, or MN scope of careand meet the eligibility criteria for either the Aged,Blind or Disabled–cash, the Housing Essential Needs(HEN) program, or the Survivors of Certain Crimes(SCC) program, which includes victims of humantrafficking as described in RCW 74.04.005.Refugee (R02, R03):The Refugee Medical Assistance program (RMA)provides CN coverage to refugees who are not eligiblefor Apple Health programs with CN or ABP scope ofcare and who meet the income and resource standardsfor this program. RMA is a 100 percent federally fundedprogram for persons granted asylum in the U.S. asrefugees or asylees. Individuals enrolled in RMA arecovered from the date they entered the U.S.Eligibility for refugees/asylees that have been inthe United States for more than eight months isdetermined the same as for U.S. citizens.Immigrants from Iraq and Afghanistan who weregranted Special Immigrant status under Section101(a)(27) of the Immigration and Nationality Act(INA) are eligible for Medicaid and Refugee MedicalAssistance (RMA) the same as refugees.
Non-Citizen ProgramsAlien Emergency Medical (AEM) (K03, N21, N25, S07):This program covers health care services to treatqualifying emergency medical conditions. To be eligiblefor AEM, an individual must: Be categorically relatable to an Apple Health programbut not eligible for the an Apple Health programsolely due to immigration status requirements (whichprogram an individual is related to determines whetherthey follow the MAGI or Classic Medicaid eligibility rulesand application processing); and Have a qualifying emergency medical condition asdescribed in WAC 182-507-0115, or 182-507-0120, thatis approved by HCA’s medical consultant team. Income and resource limits are the same as forthe program to which the AEM applications arecategorically relatable.Below is a summary of the 3 WACs that cover the AlienEmergency Medical Programs: 182-507-0110: Alien Medical Programs: This explainsthe eligibility requirements for the program. 182-507-0115: Alien Emergency Medical (AEM):The qualifying services must be provided in a hospitalsetting (inpatient, outpatient surgery, emergencyroom) that includes evaluation and management visitsby a physician and be needed to treat the emergencymedical condition. Certification is limited to the dateson which the qualifying services were provided. 182-507-0120: Alien Medical for Dialysis and CancerTreatment: The qualifying services must be needed totreat the qualifying condition of cancer, acute renalfailure, or end stage renal disease, or be anti-rejectionmedication. These services do not need to be providedin a hospital setting.State-funded long-term care services (L04, L24) This program provides in-home, residential, or nursingfacility care for a limited number of individuals whoare not eligible for an Apple Health due to immigrationstatus who need long-term care services. 182-507-0125: State-funded long-term care services –The applicant must meet all other eligibility factors forplacement including receiving an assessment that theperson meets nursing facility level of care, and receiveprior authorization by the Aging & Long-Term SupportAdministration (ALTSA), Home and Community Services(HCS). This program is subject to caseload limits.7
Supplemental Security Income (SSI)Related ProgramsSSI Program (S01):This program provides CN coverage to individualsreceiving SSI (Supplemental Security Income) cashbenefits.SSI-Related Program (S02):Effective January 1, 2022Household SizeMonthlyIncome LimitResourceLimit1 841 2,0002 1,261 3,000This program provides CN coverage to individualswho meet the SSI income and resource limits and atleast one of the following requirements: 65 years old or older (aged). Blind (as defined by the Social SecurityAdministration and determined by DSHS). Disabled (as defined by the Social SecurityAdministration and determined by DisabilityDetermination Services (DDS)).SSI-Related MN Program (S95, S99):Effective January 1, 2022Household SizeMonthly Income Limit1 8412 8413 8414 8415 8586 975This program provides MN coverage to individualswith income above the SSI income limits. Individualswho qualify and enroll in the Apple Health SSIRelated MN Program become eligible for MNcoverage after incurring medical costs equal to theamount of the household income that is above theSSI income standard.8Apple Health for Workers with Disabilities (HWD)(S08):This program provides CN coverage to adults withdisabilities (aged 16 and above) who are employedwith earnings. Health care premiums are based on asliding income scale.HWD has no asset test and no upper income limit.To be eligible, an individual must meet federaldisability requirements, be employed (including selfemployment) full or part time, and pay the monthlypremium. To receive HWD benefits, enrollees pay amonthly premium determined as a percentage oftheir income. The premium will never exceed 7.5percent of total income and may be less. AmericanIndians and Alaska Natives are exempt from payingpremiums for HWD. Also, while enrolled in HWD,a person may put earnings into a separate anddesignated account that will not be counted whendetermining eligibility for another program.
Medically Needy (MN) and SpenddownMedically Needy (F99, G95, G99, K95, K99, L95, L99,P99, S95, S99):The Medically Needy (MN) program is a federal andstate-funded Apple Health program for individualswho are aged, blind, disabled, pregnant, or a child withincome above the applicable CN limits. MN providesslightly less health care coverage than CN and requiresgreater financial participation by the individual.SpenddownAn individual with income above the limits forthe applicable CN program may enroll in the MNprogram. An enrollee is given a base period, typicallythree or six months, to spend down excess income—in other words, to incur financial obligations formedical expenses equal to their spenddown amount.(Spenddown is the amount of the individual’s incomeminus the income limit for their particular program.)The enrollee is responsible for paying these medicalexpenses.The enrollee receives MN health care coverage for theselected base period once the spenddown is met.Example: Martha is 67 years of age and applies for Apple Health for MN coveragein April. Her monthly Social Security benefit is 1,207. After disregarding 20from her Social Security benefit, which leaves 1,187, she is over the SSI monthlyincome limit of 841 by 346.Martha is found eligible for the MN spenddown program for the aged. She selectsa six- month spenddown base period. Her spenddown amount is 2,076 ( 346 x6 months) for April through September. This means that Martha is responsible forthe first 2,076 in medical costs she incurs.On May 12, Martha has surgery. After Medicare pays the eligible 80 percent of thebill, there remains a balance of 5,200 that Martha is responsible to pay. Based onher participation in the MN spenddown program, she is liable for 2,076. Once herspenddown has been met, Apple Health will pay the remaining amount of the bill.Her certification period is May 12 to September 30.If Martha’s monthly income were below 841, she would have qualified for theno-cost Apple Health for the Aged program for 12 months coverage.9
Medicare Savings Program (MSP)The Medicare Savings Program (MSP) can provideassistance with premium costs, copayments,deductibles, and co-insurance for individuals who areentitled to Medicare and meet program requirements.Qualified Medicare Beneficiary (QMB) (S03) Pays Part A and Part B premiums. Pays deductibles. Pays copayments except for prescriptions.Specified Low-Income Medicare Beneficiary(SLMB) (S05) Pays Part B premiums.Qualified Individual (QI-1) (S06) Pays Part B premiums.Qualified Disabled Working Individual(QDWI) (S04) Pays Part A premiums.Income Limits–Effective April 1, 2022 (Below limits include a 20 disregard allowed to all households)Medicare SavingsProgramFederal Poverty Level(FPL)Monthly Income Limit –One PersonMonthly Income Limit –Two PersonsQMB100% 1,133 1,526SLMB120% 1,359 1,831QI-1135% 1,529 2,060QDWI200% 2,265 3,072Resource Limits–Effective April 1, 202210Medicare SavingsProgramResource Limit – OnePersonResource Limit – TwoPersonsQMB 8,400 12,600SLMB 8,400 12,600QI-1 8,400 12,600QDWI 4,000 6,000
Long-Term Services and Supports (LTSS)and HospiceHospice servicesApple Health benefits include hospice services forpeople who are eligible under categorically needy(CN), medically needy (MN), or alternative benefitplan (ABP) programs. If a person is not eligible forCN, MN, or ABP, a determination can be made usingeligibility rules under a separate Hospice program.The hospice provider notifies the agency whenhospice services are elected. The Hospice programpays for hospice care at home, a hospice care center,or hospice in a nursing facility.Long-Term Services and Supports (LTSS)Long-term Services and Supports (LTSS) are tailoredto fit client individual needs and situations. Servicesmay be authorized through the Department of Socialand Health Services (DSHS) by Home and CommunityServices (HCS) or the Developmental DisabilitiesAdministration (DDA). These services enable peopleto continue living in their homes with help meetingtheir physical, medical, and social needs. When theseneeds can’t be met at home, care in a residential ornursing facility is available.In HCS, there are also programs available that providehelp to caregivers and people without a caregiver—Tailored Supports for Older Adults and MedicaidAlternative Care. The person in need of care must beage 55 or older and meet financial eligibility criteria.Different income standards are used to determineeligibility for CN or MN coverage for LTSS. To beeligible for most LTSS programs, a person mustfile an application and meet financial eligibilitycriteria and functional eligibility criteria (based on acomprehensive assessment).For more information about nursing home care, or home &community based services offered by HCS, contact a localHCS office. To locate the closest HCS office: visit dshs.wa.gov/office-locations.For information about financial eligibility for the DDAservices, contact the LTC Specialty Unit at 1-855-873-0642.For information about functional eligibility criteria for homeand community-based services through DDA, go to dshs.wa.gov/dda.LTSS services include the following programs:Through HCS: Community Options Program Entry System (COPES), NewFreedom, and Residential Support Waiver (RSW) (L21, L22) Community First Choice (CFC), Medicaid PersonalCare (MPC) (L51, L52) Roads to Community Living (RCL) (L41, L42) Program of All-Inclusive Care for the Elderly (PACE) (L31,L32) Nursing Facility care (L01, L02, L95, L99) Tailored Supports for Older Adults (T02) Medicaid Alternative Care (MAC) Limited funding for state-funded Long-term services fornon-citizens (L04, L24)Through DDA: Developmental Disabilities Administration (DDA) Waivers(L21, L22) Community First Choice (CFC), Medicaid Personal Care(MPC) (L51, L52) Roads to Community Living (RCL) (L41, L42) DDA Residential Habitation Centers and Intermediate CareFacilities (L01, L02, L95, L99) Hospice program (L31, L32)Covered services—scope of serviceApple Health provides access to a wide range ofmedical services. Not all eligibility groups receiveall services. Coverage is broadest under theCategorically Needy (CN) and Alternative BenefitsPlan (ABP) programs.The scope of services covered for any individualdepends on the Apple Health program in which theindividual is enrolled. The table on pages 12-13 listsspecific health care services and shows which scope ofservice category covers which services. An individual’sage is also a factor. Some services may require priorauthorization from HCA, the individual’s Apple HealthManaged Care plan, or DSHS as applicable.This table is provided for general information onlyand does not in any way guarantee that any servicewill actually be covered at the time of inquiry,because benefits, coverage, and interpretation ofbenefits and coverage may change at any time.Coverage limitations can be found in federal statutesand regulations, state statutes and regulations,state budget provisions, and Apple Health providerguides. Individuals with questions regardingcoverage should call the 800 number on the back oftheir Services Card.11
Benefit packages by programServiceABP20-ABP21 CN120-CN21 MN20-MN21 MCSAmbulance (Ground/Air)YYYYYYYApplied Behavior Analysis (ABA)YYYYYYNBehavioral health servicesYYYYYYYBlood/blood products/related servicesYYYYYYYDental servicesYYYYYYYDiagnostic services (lab and X-ray)YYYYYYYEarly and periodic screening, diagnosis, andtreatment (EPSDT) servicesYNYNYNNEnteral nutrition programYYYYYYYHabilitative servicesYYNNNNNHealth care professional servicesYYYYYYYHealth homesYYYYNNNHearing evaluationsYYYYYYYHearing aidsYYYYYYYHome health servicesYYYYYYYHome infusion therapy/parenteral nutritionprogramYYYYYYYHospice servicesYYYYYYNHospital services Inpatient/outpatientYYYYYYYIntermediate care facility/services for personswith intellectual disabilitiesYYYYYYYMaternity care & delivery servicesYYYYYYYMedical equipment, durable (DME)YYYYYYYMedical nutrition therapyYNYNYNYNursing facility servicesYYYYYYYOrgan transplantsYYYYYYYOrthodontic servicesYNYNYNNOut-of-state servicesYYYYYYNOutpatient rehabilitation services (OT, PT, ST)YYYYYNYPersonal care servicesYYYYNNNPrescription drugsYYYYYYYPrivate duty nursingYYYYYYNProsthetic/orthotic devicesYYYYYYY12
Benefit packages by programServiceABP20-ABP21 CN120-CN21 MN20-MN21 MCSReproductive health servicesYYYYYYYRespiratory care (oxygen)YYYYYYYSchool-based medical servicesYNYNYNNVision care Exams, refractions, and fittingsYYYYYYYVision hardware Frames and lensesYNYNYNNLEGENDY A service category is included for that program. Services within each service category are subject tolimitations and restrictions listed in the specific medical assistance program rules and agency issuances.N A service category is not included for that program.Clients enrolled in the Apple Health for Kids programs (with and without premium) receive CN-scope ofhealth care services. The Apple Health for Kids programs includes the children’s health insurance program(CHIP).1ABBREVIATIONSABP - Alternative Benefit PlanCN - Categorically Needy ProgramMCS - Medical Care ServicesMN - Medically Needy Program13
Other servicesNonemergency Medical Transportation (BrokeredTransport)HCA covers nonemergency medical transportationfor eligible clients to or from covered servicesthrough contracted brokers. The brokers arrangeand pay for trips for qualifying clients. Currently,eligible clients are those enrolled in Apple Healthand other state-funded medical assistance programsthat include a transportation benefit. Transportationmay be authorized for individuals who have no othermeans to access medical care.The most common types of transportation availableinclude: public transit bus, gas vouchers, client andvolunteer mileage reimbursement, taxi, wheelchairvan or accessible vehicle, commercial bus and air,and ferry tickets. More information is availableonline at: hca.wa.gov/transportation-help.Comments and questions may be directed to HCATransportation Services at hcanemttrans@hca.wa.gov.Interpreter Services – Sign LanguageHCA covers the cost of sign language interpretersfor eligible clients. This service must be requested byApple Health providers, HCA staff or HCA-authorizedDSHS staff, and must be provided by the HCAapproved contractor.Interpreter Services – Spoken languageHCA covers interpreter service for eligible clientsthrough the HCA approved contractor. Requestsfor this service must be submitted by Apple Healthproviders, HCA staff, or HCA-authorized DSHS staff.Where to apply for health care coverageModified Adjusted Gross Income(MAGI) programs In-person: Visit a local Community Service Office.For locations, go to dshs.wa.gov/esa/communityservices-find-an-office . Online: wahealthplanfinder.org .Questions? Call 1-877-501-2233 Phone: 1-855-923-4633 Paper: HCA Form 18-001P (Application for HealthCare Coverage) available at hca.wa.gov/assets/free-or-low-cost/18-001P.pdf .To submit a completed application by mail:Washington HealthplanfinderP.O. Box 946, Olympia, WA 98507Or send it by fax to: 1-855-867-4467If you want help applying, you can work with an inperson assister or call Healthplanfinder CustomerSupport at 1-855-923-4633.Aged, Blind, Disabled CoverageDisability-based Washington Apple Health, refugeecoverage, coverage for seniors 65 , and programsthat help pay for Medicare premiums and expenses: Online: washingtonconnection.org Paper: HCA Form 18-005 (Application for ABD/LTC)available at hca.wa.gov/assets/free-or-low-cost/18-005.pdf .To submit a completed application by mail:DSHS – Community Services DivisionP.O. Box 11699, Tacoma, WA 98411-6699Or send it by fax to: 1-888-338-741014Long-Term CareNursing home care, in-home personal care, assistedliving facil
312 percent of the FPL. Children who qualify and are enrolled in Apple Health for Medically Needy Kids become eligible for MN coverage after incurring medical costs equal to the amount of the household income that is above the 312 percent FPL standard. Effective April 1, 2022 Household Size Monthly Income Limit 210% FPL (No Cost) Monthly Income .