Transcription
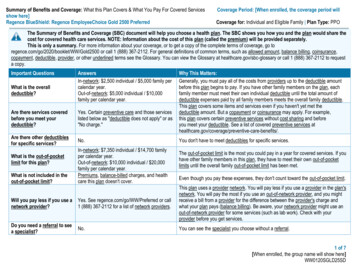
Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered Servicesshow here]Regence BlueShield: Regence EmployeeChoice Gold 2500 PreferredCoverage Period: [When enrolled, the coverage period willCoverage for: Individual and Eligible Family Plan Type: PPOThe Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan would share thecost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately.This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, go toregence.com/go/2020/booklet/WW/Gold2500 or call 1 (888) 367-2112. For general definitions of common terms, such as allowed amount, balance billing, coinsurance,copayment, deductible, provider, or other underlined terms see the Glossary. You can view the Glossary at healthcare.gov/sbc-glossary or call 1 (888) 367-2112 to requesta copy.Important QuestionsWhat is the overalldeductible?AnswersIn-network: 2,500 individual / 5,000 family percalendar year.Out-of-network: 5,000 individual / 10,000family per calendar year.Are there services coveredbefore you meet yourdeductible?Yes. Certain preventive care and those serviceslisted below as "deductible does not apply" or as"No charge."Are there other deductiblesfor specific services?No.What is the out-of-pocketlimit for this plan?What is not included in theout-of-pocket limit?In-network: 7,350 individual / 14,700 familyper calendar year.Out-of-network: 10,000 individual / 20,000family per calendar year.Premiums, balance-billed charges, and healthcare this plan doesn't cover.Why This Matters:Generally, you must pay all of the costs from providers up to the deductible amountbefore this plan begins to pay. If you have other family members on the plan, eachfamily member must meet their own individual deductible until the total amount ofdeductible expenses paid by all family members meets the overall family deductible.This plan covers some items and services even if you haven't yet met thedeductible amount. But a copayment or coinsurance may apply. For example,this plan covers certain preventive services without cost sharing and beforeyou meet your deductible. See a list of covered preventive services /.You don't have to meet deductibles for specific services.The out-of-pocket limit is the most you could pay in a year for covered services. If youhave other family members in this plan, they have to meet their own out-of-pocketlimits until the overall family out-of-pocket limit has been met.Even though you pay these expenses, they don't count toward the out-of-pocket limit.Will you pay less if you use anetwork provider?Yes. See regence.com/go/WW/Preferred or call1 (888) 367-2112 for a list of network providers.This plan uses a provider network. You will pay less if you use a provider in the plan'snetwork. You will pay the most if you use an out-of-network provider, and you mightreceive a bill from a provider for the difference between the provider's charge andwhat your plan pays (balance billing). Be aware, your network provider might use anout-of-network provider for some services (such as lab work). Check with yourprovider before you get services.Do you need a referral to seea specialist?No.You can see the specialist you choose without a referral.1 of 7[When enrolled, the group name will show here]WW0120SGLD25SD
All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.Common MedicalEventServices You May NeedPrimary care visit to treatan injury or illnessIf you visit a healthcare provider's officeor clinicSpecialist visitWhat You Will PayIn-network ProviderOut-of-network Provider(You will pay the least)(You will pay the most) 30 copay / office visit 20 copay / office visit at aretail clinicDeductible does not apply50% coinsurancefor these visits30% coinsurance for allother services 50 copay / visitDeductible does not applyfor these visitsLimitations, Exceptions, & Other ImportantInformationCoverage includes primary care visits at a retail clinic.In-network acupuncture and spinal manipulations aresubject to 30 copay / visit, deductible does not apply.Acupuncture services are limited to 12 visits / year.Spinal manipulations are limited to 10 / year.50% coinsurance30% coinsurance for allother servicesIf you have a c test (x-ray,blood work)Imaging (CT/PET scans,MRIs)No charge50% coinsurance30% coinsurance,deductible does not apply50% coinsurance30% coinsurance50% coinsuranceYou may have to pay for services that aren'tpreventive. Ask your provider if the services neededare preventive. Then check what your plan will pay for.None2 of 7
Common MedicalEventServices You May NeedPreferred generic drugs &generic drugsPreferred brand drugsIf you need drugs totreat your illness orconditionMore information aboutprescription drugcoverage is available atregence.com/go/druglist/2020/WW/6tier.Brand drugsPreferred specialty drugs& specialty drugsFacility fee (e.g.,ambulatory surgerycenter)If you have outpatientsurgeryPhysician/surgeon feesWhat You Will PayIn-network ProviderOut-of-network Provider(You will pay the least)(You will pay the most) 10 copay* / preferred generic retail prescription 20 copay / preferred generic mail order prescription25% coinsurance* / generic retail prescription20% coinsurance / generic mail order prescription 50 copay* / retail prescription 100 copay / mail order prescription50% coinsurance* / retail prescription45% coinsurance / mail order prescription20% coinsurance / preferred specialty drugs50% coinsurance / specialty drugs20% coinsurance forambulatory surgery centers;30% coinsurance for allother facilities20% coinsurance forambulatory surgery centerphysicians;30% coinsurance for allother physiciansLimitations, Exceptions, & Other ImportantInformationNo coverage for prescription drugs not on the Drug Listor prescription drugs from an out-of-network pharmacy.Limited to a 90-day supply retail (1 copay per 30-daysupply), mail order and self-injectable drugs.Limited to a 30-day supply specialty drugs (includingpreferred) and self-administrable cancer chemotherapydrugs.Deductible does not apply for all prescription drugs.No charge for FDA-approved women's contraceptivesprescribed by a health care provider and for certainpreventive drugs and immunizations at a participatingpharmacy.The first fill for specialty drugs (including preferred)may be provided at a retail pharmacy, additional fillsand fills for specialty self-administrable cancerchemotherapy drugs must be provided at a specialtypharmacy.Coverage for self-administrable cancer chemotherapydrugs is subject to 30% coinsurance.* 5 copayment or 5% coinsurance discount when filledat a preferred retail pharmacy.50% coinsuranceNone50% coinsuranceNone3 of 7
Common MedicalEventIf you need immediatemedical attentionIf you have a hospitalstayIf you need mentalhealth, behavioralhealth, or substanceabuse servicesIf you are pregnantServices You May NeedWhat You Will PayIn-network ProviderOut-of-network Provider(You will pay the least)(You will pay the most)Emergency room care30% coinsurance after 300copay / visit30% coinsurance after 300 copay / visitEmergency medicaltransportation30% coinsurance30% coinsuranceUrgent care 50 copay / visit, deductibledoes not apply; otherservices 30% coinsurance50% coinsurance30% coinsurance50% coinsurance30% coinsurance 30 copay / visit, deductibledoes not apply; otherservices 30% coinsurance50% coinsuranceInpatient services30% coinsurance50% coinsuranceOffice visitsChildbirth/deliveryprofessional services30% coinsurance50% coinsurance30% coinsurance50% coinsurance30% coinsurance50% coinsuranceFacility fee (e.g., hospitalroom)Physician/surgeon feesOutpatient servicesChildbirth/delivery facilityservices50% coinsuranceLimitations, Exceptions, & Other ImportantInformationCopayment applies to the facility charge for each visit(waived if admitted), whether or not the in-networkdeductible has been met.In-network deductible applies to in-network and out-ofnetwork services.Copayment applies to each in-network urgent care visitonly.Limited to 3,500 / day for inpatient non-emergencyadmissions in out-of-network facilities.NoneCopayment applies to each in-network office visit andpsychotherapy only.Limited to 3,500 / day for inpatient non-emergencyadmissions in out-of-network facilities.Cost sharing does not apply to certain preventiveservices. Depending on the type of services, acoinsurance or deductible may apply. Maternity caremay include tests and services described elsewhere inthe SBC (i.e. ultrasound).Limited to 3,500 / day for inpatient non-emergencyadmissions in out-of-network facilities.4 of 7
Common MedicalEventServices You May NeedHome health careIf you need helprecovering or haveother special healthneedsIf your child needsdental or eye careWhat You Will PayIn-network ProviderOut-of-network Provider(You will pay the least)(You will pay the most)30% coinsurance50% coinsuranceLimitations, Exceptions, & Other ImportantInformationRehabilitation servicesInpatient: 30% coinsuranceOutpatient: 30 copay /visit, deductible does notapply50% coinsuranceHabilitation servicesInpatient: 30% coinsuranceOutpatient: 30 copay /visit, deductible does notapply50% coinsuranceSkilled nursing careDurable medicalequipmentHospice services30% coinsurance50% coinsuranceLimited to 130 visits / year.Inpatient is limited to 30 days / year.Outpatient is limited to 25 visits / year. Copaymentapplies to each in-network outpatient visit only.Limited to 3,500 / day for inpatient non-emergencyadmissions in out-of-network facilities.Inpatient habilitative services is limited to 30 days /year.Outpatient habilitative services is limited to 25 visits /year.Neurodevelopmental therapy is subject to deductibleand coinsurance; outpatient is limited to 25 visits /year.Limited to 3,500 / day for inpatient non-emergencyadmissions in out-of-network facilities.Limited to 60 inpatient days / year.30% coinsurance50% coinsuranceNone30% coinsurance50% coinsuranceChildren's eye examNo charge50% coinsuranceChildren's glassesNo charge50% coinsuranceChildren's dental checkupNo chargeNo chargeLimited to 14 respite days / lifetime.Limited to 1 routine exam / year for individuals underage 19.Limited to 1 pair of lenses (2 lenses) and 1 standardframe / year for individuals under age 19.Limited to 2 cleanings and 2 preventive oralexaminations / year for individuals under age 19.Additional coverage is provided for basic and majorpediatric dental services.5 of 7
Excluded Services & Other Covered Services:Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Bariatric surgery Infertility treatment Routine foot care Cosmetic surgery, except congenital anomalies Long-term care Vision hardware (Adult) Dental care (Adult) Private-duty nursing Hearing aids Routine eye care (Adult)Weight loss programs, except as covered underpreventive careOther Covered Services (Limitations may apply to these services. This isn't a complete list. Please see your plan document.) Acupuncture Chiropractic care Non-emergency care when traveling outside theU.S. Termination of pregnancyYour Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agenciesis: the U.S. Department of Labor, Employee Benefits Security Administration at 1 (866) 444-3272 or dol.gov/ebsa/healthreform, or the U.S. Department of Health andHuman Services, Center for Consumer Information and Insurance Oversight at 1 (877) 267-2323 x61565 or cciio.cms.gov or your state insurance department. You mayalso contact the plan at 1 (888) 367-2112. Other coverage options may be available to you too, including buying individual insurance coverage through the HealthInsurance Marketplace. For more information about the Marketplace, visit HealthCare.gov or call 1 (800) 318-2596.Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called agrievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents alsoprovide complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance,contact the plan at 1 (888) 367-2112 or visit regence.com or the U.S. Department of Labor, Employee Benefits Security Administration at 1 (866) 444-3272 ordol.gov/ebsa/healthreform.Does this plan provide Minimum Essential Coverage? YesIf you don't have Minimum Essential Coverage for a month, you'll have to make a payment when you file your tax return unless you qualify for an exemption from therequirement that you have health coverage for that month.Does this plan meet the Minimum Value Standards? YesIf your plan doesn't meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace.Language Access Services:Spanish (Español): Para obtener asistencia en Español, llame al 1 (888) ––––––––To see examples of how this plan might cover costs for a sample medical situation, see the next ––––––––6 of 7
About these Coverage Examples:This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will bedifferent depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharingamounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion ofcosts you might pay under different health plans. Please note these coverage examples are based on self-only coverage.Peg is Having a BabyManaging Joe's type 2 DiabetesMia's Simple Fracture(9 months of in-network pre-natal care and ahospital delivery)(a year of routine in-network care of a wellcontrolled condition)(in-network emergency room visit and followup care) The plan's overall deductible Specialist copayment Hospital (facility) coinsurance Other coinsurance 2,500 5030%30%This EXAMPLE event includes services like:Specialist office visits (prenatal care)Childbirth/Delivery Professional ServicesChildbirth/Delivery Facility ServicesDiagnostic tests (ultrasounds and blood work)Specialist visit (anesthesia)Total Example CostIn this example, Peg would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn't coveredLimits or exclusionsThe total Peg would pay is 12,800 2,500 33 2,914 60 5,507 The plan's overall deductible Specialist copayment Hospital (facility) coinsurance Other coinsurance 2,500 5030%30%This EXAMPLE event includes services like:Primary care physician office visits (includingdisease education)Diagnostic tests (blood work)Prescription drugsDurable medical equipment (glucose meter)Total Example CostIn this example, Joe would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn't coveredLimits or exclusionsThe total Joe would pay is 7,400 0 2,288 31 255 2,574 The plan's overall deductible Specialist copayment Hospital (facility) coinsurance Other coinsurance 2,500 5030%30%This EXAMPLE event includes services like:Emergency room care (including medicalsupplies)Diagnostic test (x-ray)Durable medical equipment (crutches)Rehabilitation services (physical therapy)Total Example CostIn this example, Mia would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn't coveredLimits or exclusionsThe total Mia would pay isThe plan would be responsible for the other costs of these EXAMPLE covered services. 1,925 1,301 512 19 0 1,8327 of 7
medical attention Emergency room care 30% coinsurance after 300 copay / visit 30% coinsurance after 300 copay / visit Copayment applies to the facility charge for each visit (waived if admitted), whether or not the in-network deductible has been met. Emergency medical transportation 30% coinsurance 30% coinsurance