Transcription
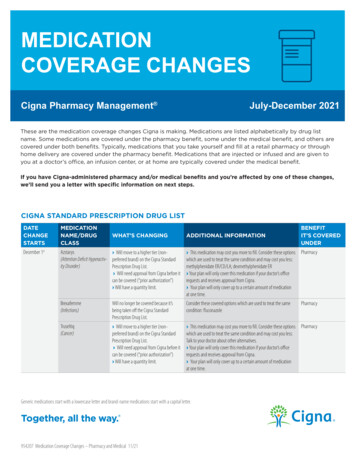
MEDICATIONCOVERAGE CHANGESCigna Pharmacy Management July-December 2021These are the medication coverage changes Cigna is making. Medications are listed alphabetically by drug listname. Some medications are covered under the pharmacy benefit, some under the medical benefit, and others arecovered under both benefits. Typically, medications that you take yourself and fill at a retail pharmacy or throughhome delivery are covered under the pharmacy benefit. Medications that are injected or infused and are given toyou at a doctor’s office, an infusion center, or at home are typically covered under the medical benefit.If you have Cigna-administered pharmacy and/or medical benefits and you’re affected by one of these changes,we’ll send you a letter with specific information on next steps.CIGNA STANDARD PRESCRIPTION DRUG er 1stAzstarys› Will move to a higher tier (non(Attention Deficit Hyperactiv- preferred brand) on the Cigna Standardity Disorder)Prescription Drug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.› This medication may cost you more to fill. Consider these options Pharmacywhich are used to treat the same condition and may cost you less:methylphenidate ER/CD/LA; dexmethylphenidate ER› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.Brexafemme(Infections)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.Consider these covered options which are used to treat the samecondition: fluconazoleTruseltiq(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.› This medication may cost you more to fill. Consider these options Pharmacywhich are used to treat the same condition and may cost you less:Talk to your doctor about other alternatives.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.WHAT’S CHANGINGADDITIONAL INFORMATIONGeneric medications start with a lowercase letter and brand-name medications start with a capital letter.954207 Medication Coverage Changes – Pharmacy and Medical 11/21BENEFITIT’S COVEREDUNDERPharmacy
CIGNA STANDARD PRESCRIPTION DRUG LIST mber 1stBENEFITIT’S COVEREDUNDERWHAT’S CHANGINGADDITIONAL INFORMATIONWelireg(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.› This medication may cost you more to fill. Consider these options Pharmacywhich are used to treat the same condition and may cost you less:Talk to your doctor about other alternatives.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.November 15thEmpaveli(Miscellaneous)› Will move to a lower tier (preferredbrand) on the Cigna Standard PrescriptionDrug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› This medication will move, or recently moved, to preferred brand. PharmacyThis means it may cost you less to fill.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.November 1stBystolic(Blood pressure/Heartmedications)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.Consider these covered options which are used to treat the samecondition: nebivololChantix(Smoking Cessation)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› This medication may cost you more to fill. Consider these options Pharmacywhich are used to treat the same condition and may cost you less:varenicline› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.Exservan(Miscellaneous)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.Consider these covered options which are used to treat the samecondition: riluzole, TiglutikLumakra(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.› This medication may cost you more to fill. Consider these options Pharmacywhich are used to treat the same condition and may cost you less:Talk to your doctor about other alternatives.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.Myfembree(Hormonal Agents)› Will move to a lower tier (preferredbrand) on the Cigna Standard PrescriptionDrug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.3› This medication will move, or recently moved, to preferred brand. PharmacyThis means it may cost you less to fill.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.Nextstellis(Contraception Products)Will move to a higher tier (non-preferredbrand) on the Cigna Standard PrescriptionDrug List.This medication may cost you more to fill. Consider these optionswhich are used to treat the same condition and may cost you less:Generic oral contraceptives (e.g. drospirenone-ethinyl estradiol)PharmacyQelbree(Attention DeficitHyperactivity Disorder)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.Consider these covered options which are used to treat the samecondition: atomoxetine, clonidine ER, guanfacine ERPharmacyZegalogue(Diabetes)› Will move to a lower tier (preferredbrand) on the Cigna Standard PrescriptionDrug List.› Will have a quantity limit.3› This medication will move, or recently moved, to preferred brand. PharmacyThis means it may cost you less to fill.› Your plan will only cover up to a certain amount of medicationat one time.ivermectin(Infections)Will be available on the Cigna StandardPrescription Drug List, but will need approval from Cigna before it can be covered(“prior authorization”).3Your plan only covers this medication if your doctor’s office requests Pharmacyand receives approval from Cigna.October 15thOctober 7thGeneric medications start with a lowercase letter and brand-name medications start with a capital letter.PharmacyPharmacy
CIGNA STANDARD PRESCRIPTION DRUG LIST ber 7thOctober 1stBENEFITIT’S COVEREDUNDERWHAT’S CHANGINGADDITIONAL INFORMATIONStromectol(Infections)Will be available on the Cigna StandardPrescription Drug List, but will need approval from Cigna before it can be covered(“prior authorization”).3Your plan only covers this medication if your doctor’s office requests Pharmacyand receives approval from Cigna.Aubagio(Multiple Sclerosis)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List and› Will need approval from Cigna before itcan be covered (“prior authorization”).› This medication will move, or recently moved, to preferred brand. PharmacyThis means it may cost you less to fill.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.Elepsia XR(Seizure Disorders)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.Consider these covered options which are used to treat the samecondition: levetiracetam ERFortivda(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List and› Will need approval from Cigna before itcan be covered (“prior authorization”).Pharmacy› If Cigna approves coverage of this medication, it may cost youmore to fill.› Consider these options which are used to treat the same conditionand may cost you less: Talk to your doctor about other alternatives.Ingrezza(Miscellaneous)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List and› Will need approval from Cigna before itcan be covered (“prior authorization”).› If Cigna approves coverage of this medication, it may cost youmore to fill.› Consider these options which are used to treat the samecondition and may cost you less: AustedoPonvory(Multiple Sclerosis)› Will move to a lower tier (preferredbrand) on the Cigna StandardPrescription Drug List and› Will need approval from Cigna before itcan be covered (“prior authorization”).› This medication will move, or recently moved, to preferred brand. PharmacyThis means it may cost you less to fill.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.Roszet(Cholesterol Medications)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List and› Will need approval from Cigna before itcan be covered (“prior authorization”).› If Cigna approves coverage of this medication, it may cost youmore to fill.› Consider these options which are used to treat the samecondition and may cost you less: atorvastatin, ezetimibe,ezetimibe-simvastatin, lovastatin, pravastatin, rosuvastatin,simvastatin tabletSomatuline Depot(Hormonal Agents)Will move to a lower tier (preferred brand) This medication will move, or recently moved, to preferred brand.on the Cigna Standard Prescription DrugThis means it may cost you less to fillList.PharmacySeptember 15thProlate solution(Pain Relief andInflammatory Disease)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.Consider these covered options which are used to treat the samecondition: oxycodone w/ acetaminophenPharmacySeptember 1stKloxxado(Substance Abuse)› Will move to a lower tier (preferredbrand) on the Cigna Standard PrescriptionDrug List and› Will have a quantity limit.3› This medication will move, or recently moved, to preferredbrand. This means it may cost you less to fill.› Your plan will only cover up to a certain amount of medicationat one time.PharmacyAugust 15thWegovy(Weight Management)Will have a quantity limit.3Your plan will only cover up to a certain amount of medication atone time.PharmacyGeneric medications start with a lowercase letter and brand-name medications start with a capital letter.PharmacyPharmacyPharmacy
CIGNA STANDARD PRESCRIPTION DRUG LIST (cont)DATECHANGESTARTSMEDICATIONNAME/DRUGCLASSJuly 20thBENEFITIT’S COVEREDUNDERWHAT’S CHANGINGADDITIONAL INFORMATIONHeparin Sod 5,000 Unit/MLsyringe(Blood Thinners/Anti-clotting)Will move to a higher tier (non-preferredbrand) on the Cigna Standard PrescriptionDrug List.This medication may cost you more to fill. Consider these optionswhich are used to treat the same condition and may cost you less:Talk to your doctor about other � Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List and› Will need approval from Cigna before itcan be covered (“prior authorization”).Pharmacy› If Cigna approves coverage of this medication, it may cost youmore to fill.› Consider these options which are used to treat the same conditionand may cost you less: Nebusal 3%, Pulmosal, Pulmozyme, sodiumchloride inhalationUkoniq(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List and› Will need approval from Cigna before itcan be covered (“prior authorization”).› Will have a quantity limit.3› If Cigna approves coverage of this medication, it may cost youmore to fill.› Consider these options which are used to treat the samecondition and may cost you less: Talk to your doctor about otheralternatives.› Your plan will only cover up to a certain amount of medicationat one time.PharmacyDupixent(Pain Relief andInflammatory Disease)Will move to a lower tier (preferred brand) This medication will move, or recently moved, to preferred brand.on the Cigna Standard Prescription DrugThis means it may cost you less to fillList.PharmacyHeparin 2,000 Unit/2 MLVial(Blood Thinners/Anti-Clotting)Will move to a lower tier (generic) on theCigna Standard Prescription Drug List.This medication will move, or recently moved, to preferred brand.This means it may cost you less to fillPharmacyHeparin 5,000 Unit/MLCarpujct(Blood Thinners/Anti-Clotting)Will move to a lower tier (generic) on theCigna Standard Prescription Drug List.This medication will move, or recently moved, to preferred brand.This means it may cost you less to fillPharmacyJuly 12thWegovy(Weight Management)Will move to a lower tier (preferred brand) This medication will move, or recently moved, to preferred brand.on the Cigna Standard Prescription DrugThis means it may cost you less to fillList.PharmacyJuly 6thLupkynis(Transplant Medications)Will need approval from Cigna before itcan be covered (“precertification”).Your plan only covers this medication if your doctor’s office requests Pharmacyand receives approval from Cigna.Tepmetko(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List and› Will need approval from Cigna before itcan be covered (“prior authorization”).› Will have a quantity limit.3› If Cigna approves coverage of this medication, it may cost youmore to fill.› Consider these options which are used to treat the samecondition and may cost you less: Talk to your doctor about otheralternatives.› Your plan will only cover up to a certain amount of medicationat one time.PharmacyVerquvo(Blood Pressure/Heartmedications)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.Consider these covered options which are used to treat the samecondition: Talk to your doctor about other alternatives.PharmacyJuly 15thGeneric medications start with a lowercase letter and brand-name medications start with a capital letter.Pharmacy
CIGNA STANDARD PRESCRIPTION DRUG LIST (cont)DATECHANGESTARTSMEDICATIONNAME/DRUGCLASSJuly 1stBENEFITIT’S COVEREDUNDERWHAT’S CHANGINGADDITIONAL INFORMATIONActemra syringe, ActemraACTpen(Pain Relief andInflammatory Disease)Will no longer be covered under themedical benefit (benefit exclusion).› This medication will only be covered under the Cignapharmacy benefit.› If you currently have approval for your plan to cover thismedication, it’s important to know that approval will end onJune 30th.MedicalAvsola(Pain Relief andInflammatory Disease)Will be available on the Cigna StandardPrescription Drug list, but will needapproval from Cigna before it can becovered (“prior authorization”).³› Your plan only covers this medication if your doctor’s officerequests and receives approvalfrom Cigna.PharmacyWill be a preferred medication under themedical benefit.If you’re currently using Remicade, ask your doctor if you shouldconsider switching to Avsola.MedicalCimzia syringe(Pain Relief andInflammatory Disease)Will no longer be covered under themedical benefit (benefit exclusion).MedicalCystaran(Eye Conditions)Will need approval from Cigna before itcan be covered (“prior authorization”) onthe Cigna Standard Prescription Drug List.3› This medication will only be covered under the Cignapharmacy benefit.› If you currently have approval for your plan to cover thismedication, it’s important to know that approval will end onJune 30th.› If you’re currently taking this medication, this change won’taffect you.› For new prescriptions as of July 1st, your plan will only coverthis medication if your doctor’s office requests and receivesapproval from Cigna.Dexcom G6 Sensor, DexcomG6 Transmitter(Diabetes - CGMs)Will no longer be covered under themedical benefit (benefit exclusion).This diabetic supply will only be covered under the Cigna pharmacy Medicalbenefit.Eligard(Hormonal Agents)Will need approval from Cigna before itcan be covered (“precertification”).Fasenra pen (auto-injector)(Pain Relief andInflammatory Disease)Will no longer be covered under themedical benefit (benefit exclusion).Your plan only covers this medication if your doctor’s office requests Medicaland receives approval from Cigna.› This medication will only be covered under the CignaMedicalpharmacy benefit.› If you currently have approval for your plan to cover thismedication, it’s important to know that approval will end onJune 30th.Fensolvi(Hormonal Agents)Will need approval from Cigna before itcan be covered (“precertification”).Your plan only covers this medication if your doctor’s office requests Medicaland receives approval from Cigna.Firmagon(Hormonal Agents)Will need approval from Cigna before itcan be covered (“precertification”).Your plan only covers this medication if your doctor’s office requests Medicaland receives approval from Cigna.FreeStyle Sensor 10,14, 2(Diabetes - CGMs)Will no longer be covered under themedical benefit (benefit exclusion).This diabetic supply will only be covered under the Cigna pharmacy Medicalbenefit.Fulphila(Blood Modifiers/BleedingDisorders)Will move to a higher tier (non-preferredbrand) on the Cigna Standard PrescriptionDrug List.This medication may cost you more to fill.4 Consider these options Pharmacywhich are used to treat the same condition and may cost you less:Nyvepria, Udenyca, Neulasta.› If you’re currently taking this medication, this change won’tMedicalaffect you until your current coverage approval ends.› Consider these preferred medications, which are availableunder the Cigna medical benefit: Nyvepria, Udenyca, Neulasta.Will have a change to itscoverage policy.Generic medications start with a lowercase letter and brand-name medications start with a capital letter.Pharmacy
CIGNA STANDARD PRESCRIPTION DRUG LIST (cont)DATECHANGESTARTSMEDICATIONNAME/DRUGCLASSJuly 1stGranix(Blood Modifiers/BleedingDisorders)WHAT’S CHANGINGADDITIONAL INFORMATIONBENEFITIT’S COVEREDUNDER› Will move to a higher tier (nonpreferred brand) on the CignaStandard Prescription Drug List and› Will need approval from Cignabefore it can be covered (“priorauthorization”).3This medication may cost you more to fill.4 Consider these optionswhich are used to treat the same condition and may cost you less:Nivestym, Zarxio.Will need approval from Cigna before itcan be covered (“precertification”).› Will move to a lower tier (preferredbrand) on the Cigna StandardPrescription Drug List.› Will need aprroval from Cignabefore it can be covered (“priorauthorization”).3Your plan only covers this medication if your doctor’s office requests Medicaland receives approval from Cigna.› This medication will move, or recently moved,Pharmacyto preferred brand. This means it may cost you less to fill.› If you’re currently using Remicade, ask your doctor if youshould consider switching to Inflectra.Will be a preferred medication under themedical benefit.If you’re currently using Remicade, ask your doctor if you shouldconsider switching to Inflectra.MedicalIngrezza5(Miscellaneous)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.PharmacyKuvan Tablet & Packets5(Miscellaneous)Will no longer be covered because it’sbeing taken off the Cigna StandardPrescription Drug List.If you’re currently taking this medication, this change won’t affectyou. Consider this covered option which is used to treat the samecondition: Austedo.› If you currently have approval for your plan to cover thismedication, it’s important to knowthat approval will end on June 30th. However, you’reautomatically approved for coverageof the generics.› Consider these covered options which are used to treat thesame condition: sapropterin tablet and powder packet.Lupron Depot, LupronDepot-PED (7.5mg,11.25mg, 15mg), LupronDepot-PED (30mg)(Hormonal Agents)Will need approval from Cigna before itcan be covered (“precertification”).Your plan only covers this medication if your doctor’s office requests Medicaland receives approval from Cigna.› Will move to a lower tier (preferredbrand) on theCigna Standard Prescription DrugList and› Will no longer need approval fromCigna before it can be covered (“priorauthorization”).› Will be a preferred medication underthe medical benefit and› Will no longer need approval fromCigna before it can be covered(“precertification”).› This medication will move, or recently moved,Pharmacyto preferred brand. This means it may cost youless to fill.› Your doctor’s office no longer has to request coverage approvalfrom Cigna.Inflectra(Pain Relief andInflammatory Disease)Nivestym(Blood Modifiers/BleedingDisorders)Nivestym(Blood Modifiers/BleedingDisorders)Nucala syringe, Nucalaauto-injector(Pain Relief andInflammatory Disease)Will no longer be covered under themedical benefit (benefit exclusion).Ogivri(Cancer)Will no longer be a preferred medicationunder the medical benefit.PharmacyPharmacy› Your doctor’s office no longer has to request coverage approval Medicalfrom Cigna.› If you’re currently using Granix, ask your doctor if you shouldconsider switching to Nivestym.› This medication will only be covered under the Cignapharmacy benefit.› If you currently have approval for your plan to cover thismedication, it’s important to know that approval will end onJune 30th.› If you’re currently taking this medication, this change won’taffect you until your current coverage approval ends.› Consider these preferred medications, which are availableunder the Cigna medical benefit: Kanjinti, Trazimera.Generic medications start with a lowercase letter and brand-name medications start with a capital letter.MedicalMedical
CIGNA STANDARD PRESCRIPTION DRUG LIST (cont)DATECHANGESTARTSMEDICATIONNAME/DRUGCLASSJuly 1stOrencia syringe, Orenciaclickjet(Pain Relief andInflammatory Disease)Will no longer be covered under themedical benefit (benefit exclusion).Remicade(Pain Relief andInflammatory Disease)› Will move to a higher tier (nonpreferred brand) on the CignaStandard Prescription Drug List and› Will have a change to its approvalrequirements (“prior authorization”).3Remicade(Pain Relief andInflammatory Disease)Will have a change to itscoverage policy.Trelstar(Hormonal Agents)Will be available on the Cigna StandardPrescription Drug List, but will needapproval from Cigna before it can becovered (“prior authorization”).3Your plan only covers this medication if your doctor’s office requests Medicaland receives approval from Cigna.Valtoco(Seizure Disorders)Will need approval from Cigna before itcan be covered (“precertification”).Your plan only covers this medication if your doctor’s office requests Pharmacyand receives approval from Cigna.Ziextenzo(Blood Modifiers/BleedingDisorders)Will be available on the Cigna StandardPrescription Drug List, but will need approval from Cigna before it can be covered(“prior authorization”).3Your plan only covers this medication if your doctor’s office requests Pharmacyand receives approval from Cigna.Zoladex(Hormonal Agents)Will move to a higher tier (non-preferredbrand) on the Cigna Standard PrescriptionDrug List.This medication may cost you more to fill.4 Consider these optionswhich are used to treat the same condition and may cost you less:Nyvepria, Udenyca, Neulasta.WHAT’S CHANGINGADDITIONAL INFORMATIONBENEFITIT’S COVEREDUNDER› This medication will only be covered under the CignaMedicalpharmacy benefit.› If you currently have approval for your plan to cover thismedication, it’s important to know that approval will end onJune 30th.› This change won’t affect you if you’re currently takingPharmacyRemicade to treat Polyarticular Juvenile Idiopathic Arthritis(pJIA).› If you currently have approval for your plan to cover Remicade,it’s important to know that approval will end on June 30th. Ifyou were approved for coverage past July 1st and your doctorwants you to continue using Remicade, you may be able toappeal this decision.› If Cigna approves coverage of Remicade, it may cost you moreto fill.4› Consider these preferred medications which are used to treatthe same condition and may cost you less: Inflectra, Avsola.› This change won’t affect you if you’re currently takingMedicalRemicade to treat Polyarticular Juvenile Idiopathic Arthritis(pJIA).› Remicade will no longer be a preferred medication under theCigna medical benefit.› Consider these preferred medications, which are availableunder the Cigna medical benefit: Inflectra, Avsola.› If you currently have approval (precertification) for your planto cover Remicade, it’s important to know that approval willend on June 30th. If you were approved for coverage past July1st and your doctor wants you to continue using Remicade, youmay be able to appeal this decision. medications start with a lowercase letter and brand-name medications start with a capital letter.GenericMedical
CIGNA VALUE PRESCRIPTION DRUG er 1stAzstarysWill no longer be covered because it’s(Attention Deficit Hyperactiv- being taken off the Cigna Prescriptionity Disorder)Value Drug List.Consider these covered options which are used to treat the samecondition: methylphenidate ER/CD/LA; dexmethylphenidate ERPharmacyBrexafemme(Infections)Will no longer be covered becauseit’s being taken off the Cigna ValuePrescription Drug List.Consider these covered options which are used to treat the samecondition: fluconazolePharmacyTruseltiq(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna ValuePrescription Drug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.› This medication may cost you more to fill. Consider these options Pharmacywhich are used to treat the same condition and may cost you less:Talk to your doctor about other alternatives.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.Welireg(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna ValuePrescription Drug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.› This medication may cost you more to fill. Consider these options Pharmacywhich are used to treat the same condition and may cost you less:Talk to your doctor about other alternatives.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.November 15thEmpaveli(Miscellaneous)› Will move to a lower tier (preferredbrand) on the Cigna Value PrescriptionDrug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› This medication will move, or recently moved, to preferred brand. PharmacyThis means it may cost you less to fill.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.November 1stChantix(Smoking Cessation)› Will need approval from Cigna before itcan be covered (“prior authorization”)› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.PharmacyExservan(Miscellaneous)Will no longer be covered becauseit’s being taken off the Cigna ValuePrescription Drug List.Consider these covered options which are used to treat the samecondition: riluzole, TiglutikPharmacyLumakra(Cancer)› Will move to a higher tier (nonpreferred brand) on the Cigna StandardPrescription Drug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.› This medication may cost you more to fill. Consider these options Pharmacywhich are used to treat the same condition and may cost you less:Talk to your doctor about other alternatives.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.Myfembree(Hormonal Agents)› Will move to a lower tier (preferredbrand) on the Cigna ValueValu PrescriptionDrug List.› Will need approval from Cigna before itcan be covered (“prior authorization”)› Will have a quantity limit.3› This medication will move, or recently moved, to preferredbrand. This means it may cost you less to fill.› Your plan will only cover this medication if your doctor’s officerequests and receives approval from Cigna.› Your plan will only cover up to a certain amount of medicationat one time.PharmacyNextstellis(Contraception Products)Will no longer be covered becauseit’s being taken off the Cigna ValuePrescription Drug List.Consider these covered options which are used to treat the samecondition: Generic oral contraceptives (e.g. ntion DeficitHyperactivity Disorder)Will no longer be covered becauseit’s being taken off the Cigna ValuePrescription Drug List.Consider these covered options which are used to treat the samecondition: atomoxetine, clonidine ER, guanfacine ERPharmacyOctober 15thWHAT’S CHANGINGADDITIONAL INFORMATIONGeneric medications start with a lowercase letter and brand-name medications start with a capital letter.BENEFITIT’S COVEREDUNDER
CIGNA VALUE PRESCRIPTION DRUG LIST ber 15thOctober 7thOctober 1stBENEFITIT’S COVEREDUNDERWHAT’S CHANGINGADDITIONAL INFORMATIONZegalogue(Diabetes)› Wi
954207 Medication Coverage Changes - Pharmacy and Medical 11/21 MEDICATION COVERAGE CHANGES Cigna Pharmacy Management July-December 2021 These are the medication coverage changes Cigna is making.