Transcription
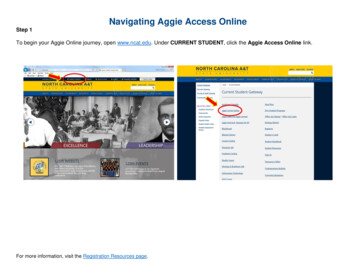
Navigating Therapy ComplianceRequirements Across The ContinuumKay Hashagen, PT, MBA, RAC-CTSenior ConsultantLW Consulting, Inc.Catherine Gill, MS, PT, MHADirector of Quality and Support Services;Compliance OfficerFranciscan VNS Home Care and Franciscan Hospice CareObjectivesMedicare Conditionsof sRequirements forTherapists in DifferentSettingsRiskReasonable & NecessaryDocumentationTraining andMonitoringCompliance forTherapists in MultipleSettingsBest Practices1
Therapy is Occurring Everywhere!HospitalsOther InpatientFacilitiesOutpatientTherapyIn Home ServicesPart A:Inpatient Units, Acute RehabUnitsPart A:Acute Rehab HospitalsLong-Term Acute HospitalsSkilled Nursing FacilitiesPart B:Freestanding Therapy ClinicsSNFsCORFsHome HealthPart A:Home HealthHospicePart B:Outpatient DepartmentsPart B:Outpatient TherapyConditions of Payment Requirements that must be met beforethe government will pay a claim2
Medicare PaymentDriversMedicare Payment DriversClinicalClinical Condition PLUSCondition Therapy me Health3
Proposed Payment ChangesHH:HHGMSNF:RCS-1Reasonable and Necessary Therapy Services Can only be safely and/oreffectively performed by or underthe supervision of a licensedtherapist Consistent with nature andseverity of patient’s illness andspecific needs Considered specific, safe andeffective treatment underaccepted professional standards4
Documentation to Support Medical NecessityGeneral Guidelines Interventions and goals directly reflect: Specific evaluation findingsSpecific functional deficitsPotential for improvement Goals are objective and measurable Standardized tests and measures are used whenavailable/appropriateAcute Care Hospitals (IP)5
Conditions of Payment - IPPhysician OrderAdmit to IPServicesCertification forLOS 20 daysMedical Necessity Requirements - IP The patient’s condition requiresinpatient hospitalization that isexpected to last at least over 2midnights The patient is receiving aMedicare-specified “inpatientonly” procedure6
Therapy Documentation Requirements - IPNo ing bodyrequirements applyState-specificdocumentation andsupervisionrequirements applyExamples:Plan of care, timelydischarge summaries,no use of inappropriateabbreviations, etc.Inpatient Rehabilitation Facilities(IRF)7
Conditions of Payment IRF60% of patients fallinto specificdiagnosticcategoriesPre-AdmissionScreen (PAS)Post AdmissionPhysician Evaluation(PAPE)Individualized Planof Care (IPOC)InterdisciplinaryTeam ConferencesPhysicianSupervisionOrders forAdmissionRequire interventionfrom multipletherapy disciplinesRequire an intensivetherapy programand meet intensityBe medically stableto benefit from theIRF servicesHave an appropriatelength of stayIRF-PAI (PatientAssessmentInstrument) must bein the recordConditions of Payment: IRF Therapy FocusIndividualizedPlan of nterventionFrom MultipleTherapyDisciplines8
Conditions of Payment: IRF Therapy FocusRequire an IntensiveTherapy Programand Meet IntensityHave an AppropriateLength of StayIRF-PAI (PatientAssessmentInstrument) Must Bein the RecordMedical Necessity Requirements IRFComplexityof nursingservicesTherapyservicesintensityThe IRF stay will onlybe considered to bereasonable andnecessary if, at thetime of admission,documentationsupports all of theseIntensity ofservicesneededNeed yteam approachfor rehab9
Therapy Medical Necessity Focus IRF Interdisciplinary team approachfor rehab Requirements for teamconferences Requirements for teammembers Therapy services intensityTherapy Documentation Requirements IRF Documentation to supportinformation entered on theIRF PAI Documentation to supportthat care is reasonable andnecessary Documentation of mode andminutes provided10
Therapy Documentation Requirements IRF Evaluation orders prior to the evaluationThe full course of intensiverehab, per the plan of care,must be initiated within 36hours from midnight the day ofadmissionFIM scores are completedaccurately for functional tasksrelated to each disciplineTherapy Documentation Requirements IRFDaily notesidentify minutesand modeProgress notessupport progresstowards dischargethat is reasonableand necessaryMissed therapy iswell documented11
Long Term Acute Care Hospitals(LTACH)Conditions of Payment LTACH The regulations thatsupport acute carehospitals apply toLTACHPhysician OrderAdmit to IPServices12
Medical Necessity Requirements LTACH The patient’s condition requiresphysician supervision either on-site oron-call 24 hours per day, 7 days perweek Admission criteria is met from day oneof the stay LOS 25 Days The need for multidisciplinary care tosupport primary and secondarydiagnoses Expected discharge planTherapy Documentation Requirements LTACHNo ing bodyrequirements applyState-specificdocumentation andsupervisionrequirements applyExamples: Plan ofcare, timely dischargesummaries, no use ofinappropriateabbreviations, etc.13
Skilled Nursing Facilities (SNF)Conditions of Payment SNF The patient must have a 3-day qualifying hospital stay OR admission within 30 days of prior discharge A physician order and certification of skilled care is required per time requirementsDiagnosis must relate to the qualifying stayMust require skilled services on a daily basisThese services can only be provided in a SNF on an inpatient basisThe patient must be assigned to a RUG groupCMS MBPM 100-02 Chapter 814
Therapy Medical Necessity Focus SNF Services must be:care provided is skilled directly related to the treatmentplan that is based on the initialevaluation at a level of complexity and thecondition of the patient mustrequire the judgment,knowledge and skills of atherapistTherapy Medical Necessity Focus SNF The services must be:reasonable and necessary provided with the expectationthat the condition will improvein a reasonable and generallypredictable period of time, or necessary for the establishmentof a safe and effectivemaintenance program15
Therapy Medical Necessity Focus SNF The services must be: considered under acceptedstandards of medical practice reasonable and necessary forthe patientreasonable and necessaryTherapy Documentation Requirements SNFA physicianorder toEvaluate andTreat isrequired priorto the firsttreatmentInitial evaluation and plan ofcare need to be completedincluding:DiagnosisDocumentationneeds to supportreasonable andnecessaryrequirements andskilledLong Term Goals (LTG)Interventions,frequency andduration16
Therapy Documentation Requirements SNFMinutes recorded to theMDS need to be supportedby documentation as skilledminutesModes of therapy need tobe recorded and supportedas per requirementsMinutes need to berecorded as “actual”minutes, not roundedHome Health (HH)17
Conditions of Payment - HH Be confined to the home Required for Medicare, not for Medicaid, varies by plan forMedicare Advantage, commercial payors Defined as:a) needing assistance to leave the home, or medicallycontraindicated to leave the home ANDb) normally unable to leave, and doing so requires asignificant effortConditions of Payment - HH Be confined to the home Under the care of the physician Physician certifies the need for home health and the plan ofcare Physician orders obtained for any changes to the plan of care A face-to-face visit 90 days before or 30 days after admission(Medicare & Medicaid) Physician recertifies the need for home health and the plan ofcare every 60 days18
Conditions of Payment - HH Be confined to the home Under the care of a physician Require intermittent skilled nursing or PT/SLPservices or continuing OT servicesConditions of Payment - HH Be confined to the home Under the care of a physician Require intermittent skilled nursing or PT/SLPservices or continuing OT services Therapy reassessments at least every 30 days tojustify the need for continued services19
Conditions of Payment - HH Be confined to the home Under the care of a physician Require intermittent skilled nursing or PT/SLPservices or continuing OT services Timely submission of OASIS assessmentTherapy Medical Necessity Focus - HH The skills of a therapist are necessary Restorative The patient’s condition will improve materially in a reasonableand generally predictable period of time, as evidenced byobjective successive measurements. Maintenance Establish or update a maintenance program Carry out a maintenance program if the patient’s conditionwarrants the skills of a therapist to do so20
Each Visit NoteTherapy Documentation Requirements - HHThe history and physical exam pertinent to the day’s visit,including the response or changes in behavior to previouslyadministered skilled servicesThe skilled services applied on the current visitThe patient/caregiver’s immediate response to the skilledservices providedThe plan for the next visit based on the rationale of priorresults.Therapy ReassessmentsTherapy Documentation Requirements - HHPerformed by a licensed therapist (not assistant)Functionally reassess the patient and comparethe resultant measurement to prior assessmentmeasurements.Document measurement results along with thetherapist’s determination of the effectiveness oftherapy, or lack thereof.21
Part B Therapy in Home HealthAgency has a Part Bprovider numberPatient no longermeets criteria for HHservices (Dischargedfrom Home Health)Patient continues torequired skilledtherapy22
Outpatient/Part B (OP)Conditions of Payment - OP Services required are based on individual needs Services are under a Plan of Care Patient must be under the care of a physician or NPPThese conditions are considered to be met when thephysician or NPP certifies the outpatient plan of care23
Medical Necessity Focus OPPatient specific is a KEY focus Services must meet accepted standards of practice Services must be specific and effective for the patient’scondition The services as documented support that the skills of aqualified therapist are necessary The documentation supports the clinician’s assessmentwith changes based on their clinical judgmentDocumentation Requirements OPNo physician’sorder is requiredInitial Evaluationand Plan of CareCertification of thePlan of Care-takersplace of orderMust be signed assoon as possibleor within 30 daysof the evaluationDelayedCertification isallowed24
Functional Reporting CodesDocumentation Requirements - OPG CodesC ModifiersRequired to be used on the initialevaluation, every progress update,recertification and dischargeDocumentation Requirements OPProgress update onor before every 10thvisitDaily documentationto support codesbilled each sessionRecertification perplan of care or perpatient needDischarge Summary25
Documentation Requirements OPThere is no longer a “therapycap” for Medicare patientsUse of the KX Modifier StillRequired Applied when the patient hasexceeded the old cap amount and thetreatment is still medically necessaryHospice (HOS)26
Conditions of Payment - HOS Beneficiary election of hospice benefit – NOE Certification of terminal illness – CTI Plan of care established and periodically reviewed and updated by the IDGFace-to-face at 3rd benefit period and eachsubsequent benefit periodMedical Necessity Focus - HOSServices inaccordance withthe plan of careHospice servicesare reasonable andnecessary formanagement of theterminal condition andrelated illness27
Documentation Requirements - HOSNo Medicare-specificdocumentationrequirementsTherapy provided toaddress the terminalillness and relatedconditionsGoals and interventionsfocused on symptommanagement ormaintenance offunctional abilitiesDocumentation Requirements - HOSPart B Therapy ProvidedOutside the Hospice Benefit Clear documentation that the servicesprovided are NOT related to the terminalillness and related conditions28
Critical Medicare Focus AreasCompare and ContrastOrders Required for Therapy EvaluationsOrders for Evaluation RequirementsInpatientNoOutpatientOrder is not required BUT plan of care must be CERTIFIED by physicianIRFOrder must be written prior to the evaluationSNF-Part AOrder is required prior to evaluation; skilled therapy must be includedSNF-Part BOrder is not required BUT plan of care must be CERTIFIED by physicianHome HealthPhysician order required prior to evaluationHospiceSpecific order is not required, but need for therapy must be on the POCLTACHOrder should be written prior to the evaluation29
Compare and ContrastMedicare Billing for Therapy EvaluationsBillableIRFOutpatientHome HealthHospiceNot BillableSNFCompare and ContrastMedicare Documentation FrequencySettingReassessmentProgress Note/Tx NotePhysician RecertInpatientNoneEvery visitNoneOutpatientEvery 10 visitsEvery visitPer POC; Maximum 90 DaysIRFWeekly PNEvery visitSNF – Part APer POC or as neededFrequency not specifiedInitial cert; 14 days after admission; every 30days thereafterSNF – Part BEvery 10 visitsEvery VisitPer POC: Maximum 90 DaysHome HealthEvery 30 daysEvery visitEvery 60 day from episode startHospiceNo requirementFrequency not specifiedRecertification of terminal illnessLTACHPer POCEvery visitPer POC30
Compare and ContrastTherapy Session Prep and Documentation Time(Medicare & Medicaid)SettingInpatientTimes not tracked for billingOutpatientAll direct patient time counts for calculating unitsIRFAll direct patient time counts for calculating minutesSNF – Part AOnly hands-on therapy counts towards RUG minutes. Non-skilled documentation is disallowedSNF – Part BAll direct patient time counts for calculating unitsHome HealthAll activities during patient visit can be counted towards visit timeHospiceAll activities during patient visit can be counted towards visit timeLTACHBilled as units; all patient time countsSpecial Issues31
Modes of TherapyIndividualConcurrentGroupCo-TreatmentOne therapisttreating one patient.One therapist isworking with morethan one patientdoing differentactivitiesTherapist working withmore than one patientwho are doing similaractivities.Two therapists (orassistants) fromdifferent therapydisciplines to 1 patientat the same time.Compare and Contrast Modes of tInpatientOKOKOKOKOutpatientRecommendedNot allowedBilled per code &definitions2 therapists must split totaltimeIRFRequirespreponderanceLimited & Reported Week1&2Limited & ReportedWeek 1 & 2Limited & Reported Week 1&2SNF – Part ARecommendedCounted 50% of minutes 25%Supporting doc requiredSNF – Part BRecommendedNot allowedBilled per codes2 therapists must split totaltimeHome HealthOKn/an/aNot addressedHospiceOKn/an/aNot addressedLTACHOKOKOKOK32
Special Issues: Group Therapy Across the Continuum Part B/Outpatient: treatment of 2 patients by one clinician whomay or may not be doing the same activities. Each patient is billedthe total time of the group using the group therapy code (97150) SNF: treatment of 4 patients with same or similar goals; totalminutes divided by 4. Max of 25% total min/week IRF: One therapist treating 2-6 patients at the same time who areperforming the same or similar activities. Minutes are counted asfull minutes for each patient, but the reason for the group, andappropriateness for the patient must be documented.Reference: Medicare Benefit Policy Manual, Ch 15, Section 230, Medicare Billing rapyServices/Downloads/11 Part B Billing Scenarios for PTs and OTs.pdfSpecial Issues: Concurrent Therapy Across the Continuum SNF: No more than 2 patients treated at the same time by one therapist,doing same or different tasks. Total time is divided 50% for each patientand this must be documented. IRF: The provision of therapy services by one licensed or certified therapist(or licensed therapy assistant, under the appropriate direction of alicensed or certified therapist) treating 2 patients at the same time whoare performing different activities. Time is recorded at 100% time. Part B/Outpatient: Under Medicare Part B there is no concurrent therapy;instead the treatment of two or more individuals simultaneously who mayor may not be performing the same activity is considered group therapyunder Part B.33
Special Issues: Co-Treatment Across the Continuum IRF: Requires documentation to support the specific benefit to the patient. Cannot be used to support staffing schedulesSNF: Per the RAI MDS 3.0 Manual, Chapter 3, Section O,documentation must support the reason for co-treatmentPart B/Outpatient: The total time billed between thetherapists must be equal to the exact duration of thetreatment sessionHome Health: Not addressed in regulations; each clinician’svisit must be reasonable and necessarySpecial Issues - Maintenance TherapyRationale - Patient has a risk for deterioration ordecline, and requires the skills of a therapist to providecare to prevent or slow deterioration in functionExamples: Parkinson’s Disease, MS, rheumatoidarthritis, ALSReference: ter.html34
Maintenance TherapyTherapy AssessmentRestorative / RehabilitativeTherapyMaintenance TherapyMaintenance TherapyMaintenance TherapyTherapy AssessmentRestorative / RehabilitativeTherapyServices Delivered byTherapistHome ProgramDeveloped &Updated by TherapistProgram Carried Outby Patient orCaregiverMaintenance TherapyProgramDevelopedby TherapistProgramDevelopedby TherapistProgramCarried outby TherapistProgram Carried Outby Patient orCaregiver35
Maintenance Therapy - DocumentationEvaluation Clearly define the medicalconditions that are resulting in therisk for decline in function Interventions address minimizingfunctional decline Establish appropriate reassessmentintervals based on patient’scondition and rate of functionaldeclineOngoing Document changes to the program toaccommodate patient’s functionaldecline Reassessment intervals adjusted basedon patient’s condition and rate offunctional decline If the therapist is going to deliver themaintenance program, documentationmust demonstrate why the uniqueknowledge & skills of a therapist arerequiredSpecial Issues: State-Specific IssuesEvaluate and provide treatment without physician orders Unrestricted Patient AccessPatient Access with ProvisionsLimited Patient AccessUSVirginIslandsDistrict ofColumbia HawaiiAlaskaLevels of Patient Access to Physical Therapist Services36
Special Issues: State-Specific IssuesSupervisory RequirementsVary by disciplineMay vary by setting even within adisciplineSpecial IssuesPayor Specific Requirements37
Cross Setting Therapist UtilizationSHAREOpportunities for Sharing Therapists Across SettingsFewer FTEs lower salarycost, lowerassociatedbenefit costsImprovedutilizationof existingstaffImprovedpatientsurgecapacity38
Opportunities for Sharing Therapists Across Settings Professional growth anddevelopment Improved therapistsatisfaction due to feeling ofstability; working full hoursSharing Therapists Across Settings39
Challenge #1: Diluted Expertise More general, less specialized expertise Increased risk of adverse events Potentially poorer clinical outcomes Examples Outpatient therapist uncomfortablemanaging ICU/CCU patients IP therapist not fully performingspecialized assessmentChallenge #2: Documentation Habits Therapists default to regulatory and documentation requirementswith which they are most familiar Examples: SNF/HH therapist documenting Part B patients the same asPart A OP/SNF therapist not documenting homebound status for HHpatients IP/OP therapist not documenting all minutes and meeting IRF3 hr. rule40
Challenge #3: Billing ErrorsExamples: OP therapist countingevaluation minutes in SNF HH/IP/IRF therapist notInappropriately counting time,resulting in billing errorscapturing minutesappropriately in OP therapy toaccurately bill CPT codes IRF therapist treatingconcurrently in an OP settingand billing a 1:1 therapyChallenge #4: Unfamiliar Documentation Tools Decreased familiarity with sitespecific EHR forms, processesExamples: Use of flow sheets (OP) Specific standardized testsper diagnosis (OP) or persetting (SNF) G codes (OP) vs G codes (HH) Capturing non-therapyrequirements (HH)41
Challenge #5: Accountability IssuesLack of ManagementAccountabilityExample: Lack of follow up withclinician when issues areidentified Unable toaccurately/completelyevaluate performanceChallenge #6: Maintaining Regulatory KnowledgeNot Included in Regular UpdatesExample: New/revised LCDs notcommunicated Changes indocumentationrequirements Changes in allowable CPTcodes42
Challenge #7: Decline in ProductivityUnfamiliarity With SettingExample: EHR navigation issues Site-specific equipmentusage Site-specific logistics Site-specific communicationexpectationsChallenge #8: Meeting Customer ExpectationsExample: Lack of progressdue toinexperiencedtherapist Uncomfortabletherapist perceivedas less trustworthy43
DENIALSIdentify The Root Cause of Denials Is there a system in place toidentify if there are denialsrelated to: Medical necessity or Technical errors Analyze the causesExample: Providing visitsbeyond orders44
Best PracticesChallengesValue To Share TherapistsRequired SupportDailyFrequency of OversightOccasionalas neededWeeklyRareFrequency of Practice45
Challenge #1: Diluted ExpertiseStrategies: Competency assessmentcompetency Site-specific case studiessupervisiontraining Mentor assignment Increased supervision and oversightChallenge #2: Documentation HabitsStrategies: Job aides/cheat sheets Use of EHR alerts/hard stopsmonitoringalerts Increased monitoring with follow up feedbackjob aids46
Challenge #3: Billing ErrorsStrategies: Job aides/cheat sheets Daily/weekly pre-billing reviewsspot checkdocumentationrequirementsChallenge #4:Unfamiliar Documentation ToolsStrategies: Laminated screen shotsmentor Mentor assignmentdocumentation Refresher training for problematic areas training Built in ALERTS in EHR for required documentation47
Challenge #5: Accountability IssuesStrategies: Collaborative evaluationscollaboration Site-specific evaluationsperformance Consistent performance expectations evaluationChallenge #6: Maintaining Regulatory KnowledgeStrategies: Send email updates to all coveringtherapistsALERTS Use Senior Therapists to promotecommunicationinformationpromote Develop NEW ALERTS across thecontinuum Keep a communications bulletin board ineach location48
Challenge #7: Decline in ProductivityStrategies: Provide job aids that clearlyoutline expectations Use schedules Try to develop Buddy Teams withregular covering therapists Investigate root causes of lowproductivityexpectationsBuddyschedulesChallenge #8: Meeting Customer ExpectationsStrategies: Strategic patient assignments Implement a Buddy System withSenior/Lead therapist on call forquestions Competency training forequipment use and clinicalexpectationsassignmentstrainingBuddy49
Sharing Therapists Across SettingsOther successful approaches?Q&A50
Thank You for Your AttentionKay Hashagen, PT, MBA, RAC-CTLW Consulting, Inc.KHashagen@LW-Consult.comCatherine Gill, MS, PT, MHAFranciscan VNS Home Care and FranciscanHospice CareCatherine.Gill@FranciscanAlliance.org51
services Need for rehab physician medical managemen t Interdisciplinary team approach for rehab Intensity of services needed Therapy services intensity Medical Necessity Requirements IRF The IRF stay will only be considered to be reasonable and necessary if, at the time of admission, documentation supports all of these