Transcription
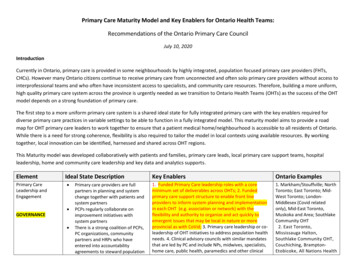
Primary Care Maturity Model and Key Enablers for Ontario Health Teams:Recommendations of the Ontario Primary Care CouncilJuly 10, 2020IntroductionCurrently in Ontario, primary care is provided in some neighbourhoods by highly integrated, population focused primary care providers (FHTs,CHCs). However many Ontario citizens continue to receive primary care from unconnected and often solo primary care providers without access tointerprofessional teams and who often have inconsistent access to specialists, and community care resources. Therefore, building a more uniform,high quality primary care system across the province is urgently needed as we transition to Ontario Health Teams (OHTs) as the success of the OHTmodel depends on a strong foundation of primary care.The first step to a more uniform primary care system is a shared ideal state for fully integrated primary care with the key enablers required fordiverse primary care practices in variable settings to be able to function in a fully integrated model. This maturity model aims to provide a roadmap for OHT primary care leaders to work together to ensure that a patient medical home/neighbourhood is accessible to all residents of Ontario.While there is a need for strong coherence, flexibility is also required to tailor the model in local contexts using available resources. By workingtogether, local innovation can be identified, harnessed and shared across OHT regions.This Maturity model was developed collaboratively with patients and families, primary care leads, local primary care support teams, hospitalleadership, home and community care leadership and key data and analytics supports.ElementPrimary CareLeadership andEngagementIdeal State Description GOVERNANCE Primary care providers are fullpartners in planning and systemchange together with patients andsystem partnersPCPs regularly collaborate onimprovement initiatives withsystem partnersThere is a strong coalition of PCPs,PC organizations, communitypartners and HRPs who haveentered into accountabilityagreements to steward populationKey EnablersOntario Examples1. Funded Primary Care leadership roles with a coreminimum set of deliverables across OHTs; 2. Fundedprimary care support structure to enable front lineproviders to inform system planning and implementationin each OHT (e.g. association or network) with theflexibility and authority to organize and act quickly toemergent issues that may be local in nature or moreprovincial as with CoVid; 3. Primary care leadership or coleadership of OHT initiatives to address population healthneeds. 4. Clinical advisory councils with similar mandatesthat are led by PC and include NPs, midwives, specialists,home care, public health, paramedics and other clinical1. Markham/Stouffville; NorthToronto; East Toronto; MidWest Toronto; LondonMiddlesex (Covid relatedonly), Mid-East Toronto,Muskoka and Area; SouthlakeCommunity OHT2. East Toronto,Mississauga Halton,Southlake Community OHT,Couchiching, BramptonEtobicoke, All Nations Health
health initiativesCross SectoralGovernance & SharedAccountability GOVERNANCE Relationships between PCorganizations and providers providefor an organized, accountablenetwork of careRelationships and clear governancestructures between PC, patientsand local health and communityprovidersAll organizations have access to thesame data to plan and monitorservice provisionleaders where appropriate1. Primary care leadership is supported and enabled tohave a prominent role at the OHT leadership level; 2.There is primary care representation in all aspects of OHTplanning and governance; 3. Data on primary carepractices (including CHCs and NPLCs) such as patientenrolment, provider FTEs, and health care utilization areavailable to primary care providers and regional primarycare leadership; 4. Shared accountability* of allorganizations of each OHT to support primary caredelivery aligned with population needs; 6. Key data forplanning and research is available centrally and integratedacross providers at a patient level.Partners, Mid-West Toronto3. above North York;*1.&2.Many internationalexamples (e.g. UK,Switzerland, Sweden,Germany, Australia)1. & 2. Couchiching; AllNations; Guelph; EastToronto; Mississauga Halton;Brampton-Etobicoke;Muskoka and Area; LondonMiddlesex; North Toronto;Hamilton.*Accountability is defined as shared vision/purpose to create a coalitionof the willing.Primary CareAttachment OPERATIONS All patients who want or need aprimary care provider are attachedThere is an easily accessibledatabase that enables full healthsystem awareness of PCattachmentPCPs consistently report theirintentions to change practice totheir local system partners (e.g.retire, take extended leave, changefocus)1. Processes in place in all organizations to identifypatients' primary care provider, level of attachment andpatients without a primary care provider; 2. Single accesspoint for patients looking for a PCP in each OHT withfacilitated attachment through connectors when needed;3. Easily accessible database enables full health caresystem awareness of the rates of PCP attachment in aneighborhood and OHT; 4. A common agreement on howto prioritize and distribute patients between PC providersfor attachment, including managed entry of FHO positions;5. Virtual care solutions are equitably available, integratedwith EMR systems and enabled across Ontario (withreliable internet access) together with standards onappropriate use of virtual care; 6. Primary care providerhuman resource management planning process in all OHTsensure primary care is matched to population needs andsuccession planning addresses the issue of physicianretirement/leaves to ensure patients have continuity of2. Health Care Connectors inOHT regions; 6. HHR Modeldeveloped by University ofOttawa with the TC –LHIN.
Primary Care andSpecialist Access OPERATIONS Continuity of Care OPERATIONS Centralized intake and e-referralprocesses are in place and easilyaccessed for specialists andspecialized clinicsA coordinated integrated accesspoint for a suite of services (SCOPE)is implemented in all geographiesAll patients have timely access toPC including in the home whenrequiredHome care coordinators are fullyaligned and integrated with PCCommunity and hospital providersroutinely connect with PC to meetpatient needs in a timely mannerAppropriate post dischargeappointments are booked atdischarge and information is sharedwith PCPsWarm handovers facilitatecontinuity of care for patients withcomplex needs at all transitionpointsPCPs have one number to call toaccess community care resourcesand servicesprimary care.1. All primary care physicians/NPs have timely and easilyfacilitated access to specialists, diagnostic, hospital andcommunity resources to meet patient needs (e.g. SCOPEplatform) in all OHTs for real-time and virtual resources aswell as an organized scaffold to nimbly respond to urgentand ongoing primary care needs; This includes rural accessto specialty care in urban centres. 2. Centralized intakeand referral processes for all specialties and subspecialties are in place and easily accessed by all PCproviders; 3. Specialist directory that is up to date andeasily accessible by all PCPs. 4. Comprehensive primarycare outreach is available for vulnerable populations whohave difficulty accessing office-based and/or virtual care eg. homebound patients, those residing in shelters andsupportive housing.1. Care coordinators are aligned and attached to primarycare practices; 2. There is one portal to access all healthcare records for both patients and their providers. 3.Patients have access to information about providerselectronically for communication and self-booking needs;4. After hours primary care is coordinated across all PCproviders regardless of their model of care, and 24/7 careis available for vulnerable homebound patients and peopleliving in congregate spaces, long term care and palliativecare; 5. Walk-in clinics/virtual walk-in clinics are part of theOHT and have organized and integrated linkages with PCPsincluding access to relevant PCP records and timelyreporting back to the responsible PCP ; 6. CCPs areavailable electronically by all providers in the circle of carethrough a dynamic platform that can both be updated andcommunicated within and across providers; 7. Hospitaldischarge summaries are received within 48 hours ofdischarge with a contact number for clarification ifrequired: 8. PODS are expanded for all dischargedpatients; 9. HRM is full implemented by all facilities andprimary care providers with e-Notification; 10.There is onenumber to call for patients to provide timely linkages backto care providers and one number to call for warm handoffs between providers.1. Mid-West Toronto is thelead for SCOPE, now availablein Mid-East Toronto, WestToronto, East Toronto, NorthToronto, London,Scarborough, BramptonEtobicoke; 2. Centralizedintake for selected specialtiesin central Toronto (Addictionmedicine, low back pain,others in progress)4. North Toronto, Mid-EastToronto, East Toronto(Hubsn’n MUMs model).1. FHTs/CHCs in centralToronto regions 10. Hypercarein East Toronto facilitates postdischarge communicationbetween PC and specialists.
High PerformingInterprofessionalTeams OPERATIONS Primary CareInformationManagement andCommunication DIGITAL All people in all geographic areaswho need interprofessional carehave an identifiable, cohesiveinterprofessional team aligned totheir needsCore team compositions are alignedwith health and social needs ofpopulations being servedInterprofessional team resourcesare equitably allocated andprioritized by population need andavailable resourcesChronic disease management andprevention is organized and easilyaccessed locallyDecisions about how care isdelivered are made using ethicalprinciples and valuesVirtual team consultations areaccessible for patients withmultimorbidity and their familyphysiciansAll PCPs have access to and useclinical information through centralrepositories (that includelaboratory, hospital, home care anddiagnostic information) for optimalpatient outcomes with efficient useof health care resourcesEMR systems are interoperablewith all health care informationplatforms with a common log inAll PCPs use secure provider toprovider and provider to patientcommunicationsPractice and geographic populationhealth data is available and usedregularly for service deliveryplanning and evaluationPractice and geographic population1. Establish & implement shared health and social needsbased criteria for access to interprofessional team care forall Ontario residents; 2. Establish a minimalinterprofessional team standard tailored to the patientroster needs for all practices (teams could be co-located,intermittently co-located or virtual aligned with patientneeds and contexts) and includes public health and homecare; 3. Establish a set of standardized performancemeasurements (common key performance measures KPMs) to track access to interprofessional care, efficientuse of IP team resources and patient experience measures(such as patient activation in self-management and PatientReported Experience Measures -PREMs) within and acrossOHTs; 4. Establish a provincial community of practice forinterprofessional team-based primary care to identify andspread best practices of efficient models and contribute toevidence-base in IPC team care.1.and 2. Guelph; 2. NorthToronto mobile IP Teams;North York mobile IP Team;West SR IPC Team; SCOPEPlatform as a scaffold foraccessing chronic diseasemanagement and communityresources andinterprofessional teams. 3.Central Toronto (West, MidWest, Mid-East, East , North)established common IP teamperformance metrics andinitiated a community ofpractice for IP teams.1. Primary Care providers have EMR systems that provideconsistent and efficient access to patient information andthere are clear expectations for EMR vendors to respondto identified deficiencies in timely and efficient access toavailable patient information; 2. Access to a shared patientrecord that is common and available as clinicallyappropriate between the hospital, PC providers, homecare, paramedics, public health, community careproviders, and includes laboratory and diagnosticimaging/test results; 3. EMR systems are interoperablewith all health care information platforms with a commonsingle log in; 4. All EMR systems, communications andrepositories, and integrated virtual care solutions areavailable to all PCPs with no financial burden. 5. HospitalEHR systems across an OHT and within an OHT referralnetwork are on a common platform to enable easieraccess by PCPs; 6. All PCPs have access to a SecureProvider-Patient communications platform allowing3. and 5. South GeorgianBay;4. Partial example: ONE IDBundle roll-out centralToronto; 6. MyChartexpansion; 7. Hypercare inEast Toronto
Patient Experience COMMUNITYENGAGEMENT Provider Experience OPERATIONS health data is available and usedregularly for service deliveryplanning and evaluation (includingregistries of vulnerablepopulations)Patients contribute their knowledgeand experience to co-design howcare is delivered and evaluated atthe organizational levelPatients inform their own care andare able to be a full member oftheir care team.Patients experience care that isconnected and coherent over timeefficient two-way communication where appropriate. 7.All PCP and specialists use a secure platform that allowssecure and in-time communication about patient care.All PCPs are part of identifiable,cohesive interprofessional teamsand are able to easily access theresources required to meet theneeds of their patientsPCPs have the supports required tocare for their patients and managetheir practices efficiently1. PPE procurement is organized across the OHT andinvolves the hospital, PCPs, community providers, longterm care, congregate care settings, paramedics as well asdental and optometry with shared procurement solutions; 4. Ontario Primary CareThis should be expanded to include other needed supplies. Council2. Primary care is supported by local Infection Prevention& Control teams to operate safely during the Covidpandemic and on an ongoing basis; 3. Coordinated primarycare led assessment centres are available for symptomaticpatients to reduce the burden on individual practices andpreserve PPE 4. Existing interprofessional teams areexpanded and new teams created with existingorganizations to ensure each PCP has interprofessionalproviders to meet the needs of their patients; 5. Primarycare Primary care providers have a provincial council tobring forward challenges and inform viable solutions toensure primary care is well supported across the province.The Ontario Primary Care Council:1. Patient & family advisory groups co-design how care isdelivered within primary care and between primary careand other sector; 2. Patients actively participate in careplanning in primary care and with other members of theirhealth care team;1. North Toronto PFAC; SCOPEPatient Advisory group; MidWest Toronto - OHT co-designwith patients with livedexperience; Mid-West SCOPEPatient Advisory Committee;Brampton-Etobicoke;2.Telemedicine IMPACT Plusfor virtual patient-presentinterprofessional careplanning;- West Toronto, MidWest Toronto, Mid-EastToronto, East Toronto, NorthToronto.3. Guelph OHT (functionsbased approach); Couchiching;
Jocelyn Charles, Mira Backo-Shannon, Yoel Abells, Loredana Di Santo, Larry Erlick, Cathy Faulds, Curtis Handford, Brian Klar, Emilie Lam, David Makary, David Mathies,John McKee, Kim McIntosh, Pauline Pariser, Dan Pepe, Paul Preston, Jillie Retson, Harpal Singh, Don Smith, Rebecca Stoller, Greg Stevens, Shane Teper, Kevin Workentin; TiaPham, Tammy Packer; Nadine Laraya; Cathy Ridson; Scott Wooder.
the first step to a more uniform primary care system is a shared ideal state for fully integrated primary care with the key enablers required for diverse primary care practices in variable settings to be able to function in a fully integrated model. this maturity model aims to provide a road map for oht primary care leaders to work together to