Transcription
1 of 95(https://www.aetna.com/)Number: 0050Policy*Please see amendment for Pennsylvania Medicaid at the endofthis CPB.I. Aetna considers the following procedures medicallynecessary for treatment of varicose veins when thefollowing criteria are met: great saphenous vein or smallsaphenous vein ligation / division / stripping, radiofrequencyendovenous occlusion (VNUS procedure), and endovenouslaser ablation of the saphenous vein (ELAS) (also known asendovenous laser treatment (EVLT)).Last Review03/09/2018Effective: 11/20/1995Next Review: 01/10/2019Review HistoryDefinitionsA. Incompetence at the saphenofemoral junction orsaphenopopliteal junction is documented by recent(performed within the past 6 months) Doppler or duplexultrasound scanning, and all of the following criteria aremet:1. Ultrasound documented junctional reflux duration of500 milliseconds (ms) or greater in thesaphenofemoral or saphenopopliteal vein to betreated; and2. Vein size is 4.5 mm or greater in diameter measuredby ultrasound immediately below the saphenofemoralClinical Policy Bulletin Notes
2 of 95or saphenopopliteal junction (not valve diameter atjunction); and3. Saphenous varicosities result in any of the following:a. Intractable ulceration secondary to venous stasis;orb. More than 1 episode of minor hemorrhage from aruptured superficial varicosity; or a singlesignificant hemorrhage from a ruptured superficialvaricosity, especially if transfusion of blood isrequired; orc. Saphenous varicosities result in either of thefollowing, and symptoms persist despite a 3‐monthtrial of conservative management* (includinganalgesics and prescription gradient supportcompression stockings):i. Recurrent superficial thrombophlebitis; orii. Severe and persistent pain and swellinginterfering with activities of daily living andrequiring chronic analgesic medication.*Note: A trial ofconservative management is notrequired for persons with persistent orrecurrent varicosities who have undergone priorendovenous catheter ablation procedures orstripping/division/ligation in the sameleg because conservative management isunlikely to be successful in this situation.B. Surgical ligation (including subfascial endoscopicperforator vein surgery (SEPS)) or endovenous ablationprocedures are considered medically necessary for thetreatment of incompetent perforating veins with veindiameter measured by recent ultrasound of 3.5 mm orgreater with outward flow duration of 500 millisecondsduration or more, located underneath an active or healedvenous stasis ulcer (also known as CEAP C5 or C6) (see
3 of 95Appendix).C. Endovenous ablation procedures are consideredmedically necessary adjunctive treatment of symptomaticaccessory saphenous veins for persons who meet medicalnecessity criteria for endovenous ablation above and whoare being treated or have previously been treated by oneof the procedures listed above for incompetence (i.e.,reflux) at the saphenofemoral junction orsaphenopopliteal junction and anatomically relatedpersistent junctional reflux is demonstrated after thegreat or small saphenous veins have been removed orablated.Note: Initially, endovenous ablation therapy of the first veinand of the second and subsequent veins in each affectedextremity is considered medically necessary when criteriaare met. (Note: Thus one primary code and one secondarycode for each affected leg are considered medicallynecessary for initial endovenous ablation treatment.)Additional endovenous ablation therapy is consideredmedically necessary for persons with persistent or recurrentjunctional reflux of the greater saphenous vein, lessersaphenous vein following initial endovenous ablationtherapy. (In order to authorize additional endovenousablation, there should be documentation that the membercontinues to have symptoms and ultrasound showingpersistent junctional reflux.) Additional endovenousablation therapy may also be necessary for treatment ofaccessory saphenous veins as noted above. Theseprocedures are considered experimental and investigationalfor treatment of varicose tributaries and accessory veinsother than the accessory saphenous vein. These proceduresare considered cosmetic for all other indications.Note: Doppler or duplex ultrasound studies are considerednecessary prior to varicose vein treatment to assess theanatomy and to determine whether there is significant refluxat the saphenofemoral or saphenopopliteal junction
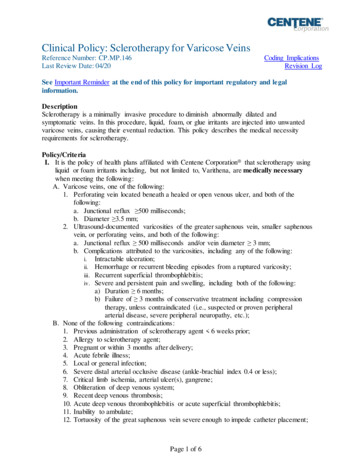
4 of 95requiring surgical repair, and after completion of thetreatment to determine the success of the procedure anddetect thrombosis. Ultrasound guidance is inclusive of theVNUS or ELAS procedures.Note: The term endovenous catheter ablation (EVCA) is anon‐specific term that refers to the several catheter basedminimally invasive alternatives to surgical stripping such asradiofrequency endovenous occlusion (VNUS procedure)and endovenous laser ablation of the saphenous vein(ELAS). In assessing the medical necessity of EVCA,reference should be made to the specific technique that isbeing employed.II. Aetna considers liquid or foam sclerotherapy (endovenouschemical ablation) (e.g., Varithena) medically necessaryadjunctive treatment of symptomatic saphenous veins,varicose tributaries, accessory, and perforator veins 2.5 mmor greater in diameter, measured by recentultrasound, for persons who meet medical necessity criteriafor varicose vein treatment in section I above and are beingtreated or have previously been treated by one or more ofthe procedures noted in section I above for incompetence(i.e., reflux) at the saphenofemoral junction orsaphenopopliteal junction. Varithena has not been proven tobe more effective than other methods of foamsclerotherapy.Sclerotherapy is considered experimental and investigationalfor treatment of reflux of the saphenofemoral junction orsaphenopopliteal junction the because sclerotherapy hasnot been proven to be effective for treatment of junctionalreflux. Sclerotherapy alone has not been shown to beeffective for persons with reflux at the saphenofemoral orsaphenopopliteal junctions; under established guidelines,individuals with reflux should also be treated withendovenous ablation, ligation or division of the junction toreduce the risk of varicose vein recurrence. Sclerotherapy isconsidered cosmetic for treatment of veins less than 2.5 mm
5 of 95in diameter and for all other indications.Note: Since ultrasound‐monitored or duplex‐guidedtechniques for sclerotherapy have not been shown todefinitively increase the effectiveness or safety of thisprocedure, these tests are only considered medicallynecessary when initially performed to determine the extentand configuration of varicose veins. Ultrasound‐ orradiologically guided or monitoring techniques are of noproven value when performed solely to guide the needle orintroduce the sclerosant into the varicose veins.Note: The number of medically necessary sclerotherapyinjection sessions varies with the number of anatomicalareas that have to be injected, as well as the response toeach injection. Usually 1 to 3 injections are necessary toobliterate any vessel, and 10 to 40 vessels, or a set of up to20 injections in each leg, may be treated duringone treatment session. Initially, up to two sets of injectionsof sclerosing solution in multiple veins in each affected leg(i.e., a total of four sets of injections if both legs are affected)are considered medically necessary when criteria are met.(Note: A set of injections is defined as multiple sclerotherapyinjections during a treatment session.) Additional sets ofinjections of sclerosing solution are considered medicallynecessary for persons with persistent or recurrentsymptoms.III. Aetna considers ambulatory phlebectomy ortransilluminated powered phlebectomy (TriVex System)medically necessary adjunctive treatment of symptomaticsaphenous veins, varicose tributaries, accessory, andperforator veins 2.5 mm or greater in diameter for personswho meet the medical necessity criteria for varicose veintreatment in section I above and who are being treated orhave previously been treated by one or more of theprocedures noted in section I above for incompetence (i.e.,reflux) at the saphenofemoral junction or saphenopoplitealjunction. Ambulatory phlebectomy or transilluminated
6 of 95powered phlebectomy is considered experimental andinvestigational for treatment of junctional reflux as theseprocedures have not been proven to be effective for theseindications. Ambulatory phlebectomy and the TriVex systemis considered cosmetic for veins less than 2.5 mm indiameter and all other indications. Note: Transilluminatedpowered phlebectomy has not been proven to be superiorto other methods of varicose vein removal. Therefore, theTriVex procedure should be billed as any other varicose veinremoval procedure.Note: Initially, up to two multiple stab phlebectomy incisionsin each affected extremity (i.e., a total of four multiple stabincisions if both legs are affected) are considered medicallynecessary when criteria are met. Additional multiple stabphlebectomy incisions are considered medically necessaryfor persons with persistent or recurrent symptoms. (Note: Aset of stab phlebectomy incisions is defined as multiple stabphlebectomy incisions during a treatment session.)IV. Aetna considers photothermal sclerosis (also referred to asan intense pulsed light source, e.g., the PhotoDermVascuLight, VeinLase), which is used to treat small veins suchas small varicose veins and spider veins, cosmetic becausesuch small veins are cosmetic problems and do not causepain, bleeding, ulceration, or other medical problems.V. Aetna considers transdermal laser treatment experimentaland investigational for the treatment of large varicose veinsbecause it has not been proven in direct comparative studiesto be as effective as sclerotherapy and/or ligation and veinstripping in the treatment of the larger varicose veinsassociated with significant symptoms (pain, ulceration,inflammation). Note: Although transdermal Nd:YAG laserhas been shown to be effective for the treatment oftelangiectasias and reticular veins, treatment of these smallveins is considered cosmetic.VI. Aetna considers endomechanical or mechanicochemical
ablation (MOCA) (e.g., ClariVein) experimental andinvestigational for varicose veins because it has not beenproven to be as effective as established alternatives.VII. Aetna considers Asclera polidocanol injection as cosmetic;although Asclera has been approved by the Food and DrugAdministration (FDA) for the treatment of telangiectasiasand reticular veins less than 3 mm in diameter, treatment ofthese small veins is considered cosmetic.VIII. Aetna considers valvular reconstruction medically necessaryfor chronic venous insufficiency.IX. Aetna considers micronized purified flavonoid fraction forthe treatment of varicose veins experimental andinvestigational because its effectiveness has not beenestablished.X. Aetna considers the VeinGogh Ohmic Thermolysis Systemexperimental and investigational because of insufficientevidence of its effectiveness.XI. Aetna considers the medical adhesive (also referred to ascyanoacrylate superglue, n‐butyl‐cyanoacrylate) (e.g.,VariClose Vein Sealing System, VenaSeal Closure System) forthe treatment of varicose veins experimental andinvestigational because its effectiveness has not beenestablished.XII. Aetna considers polymorphism genotyping of matrixmetalloproteinases genes (e.g., MMP1, MMP2, MMP3, andMMP7) as markers of predisposition to varicose veinsexperimental and investigational because the effectivenessof this approach has not been established.XIII. Aetna considers synthetic matrix metalloproteinasesinhibitors for the treatment of varicose veins experimentaland investigational because its effectiveness has not beenestablished.7 of 95
8 of 95For endoluminal cryoablation (also referred to as cryofreezing,cryostripping, cryosurgery, cryotherapy) for varicose veins, seeCPB 0100 ‐ Cryoablation (./100 199/0100.html).BackgroundVaricose veins are a common condition. In adult westernpopulations visible varicose veins are present in 20 to 25 % ofwomen and 10 to 15 % of men. In most persons, varicose veinsdo not cause symptoms other than poor cosmesis. Varicosevein surgery is one of the most commonly performed cosmeticprocedures in the United States.Most varicose veins do not require medical treatment (Tapleyet al, 2003). In some cases, however, the circulation may behindered enough to cause swelling of the foot and ankle,discomfort, a tingling sensation, or a feeling of heaviness. Formost people with varicose veins, wearing specially fitted elasticstockings is all that is needed. The stockings should be carefullyfitted to the individual, providing the most pressure in thelowest part of the leg. The stockings should be put on whenfirst arising in the morning, preferably before getting out of bed.Exercise such as walking or cycling also helps promotebetter circulation from the lower part of the body. Resting withthe legs elevated will help promote circulation; in contrast,sitting with the legs crossed can aggravate the condition.Authorities have recommended 6 or more months as areasonable duration for a trial conservative management (NHS,2005).A substantial proportion of varicose vein symptoms respond toconservative management. A randomized controlled clinicaltrial compared surgery (n 124) to conservative management(n 122) of varicose veins (Michaels et al, 2006). Conservativemanagement consisted of lifestyle advice relating to exercise,leg elevation, management of weight and diet, and the use ofcompression hosiery. In the surgical arm of the trial patientsreceived the same lifestyle advice but also underwent surgicaltreatment, consisting of flush ligation of sites of reflux, stripping
9 of 95of the long saphenous vein and multiple phlebectomies, asappropriate. Although a greater proportion of patientsassigned to surgery plus lifestyle advice at relieving symptomsat 1 year, approximately one‐third of subjects assigned toconservative management reported some relief fromconservative management with compression hosiery. At 2years, there was no significant difference in symptomimprovement between groups assigned to conservativemanagement versus surgery. The authors posited that the lackof significant difference in symptomatology between groups at2 years may have been due to cross‐overs, with 7 patients inthe conservative management group opting for surgery in year1 and 37 patients opting for surgery in year 2. The study alsofound that persons assigned to surgery plus lifestyle advice hada greater improvement in cosmesis and quality of life thanpersons assigned to lifestyle advice alone, although it is notknown whether improvements in quality of life were primarilyrelated to improvements in cosmesis versus reductions insymptomatology. Weaknesses of the study included asubstantial loss to follow‐up in all groups. Fifteen of the 124patients assigned to surgery either refused surgery in favor ofconservative management or declined surgery due to fitness.Of the remaining 109 patients who underwent surgery, 43 werelost to follow up by the first year. Of subjects assigned toconservative treatment, 21 were lost to follow‐up by the firstyear. The authors observed that, although surgery was moreeffective at improving symptomatology at 1 year, a substantialproportion of patients assigned to conservative treatmentreported resolution or improvements in aching (26 %),heaviness (46 %), itching (56 %), and swelling (68 %). Inaddition, a substantial proportion of persons assigned toconservative management reported improvements incosmesis. "Indeed, 22 % of the latter reported that they nolonger had cosmetic concerns. These observations suggest asubstantial benefit from surgery but perhaps support the casefor careful evaluation of patients’ symptoms and problemswhen considering surgical treatment."An editorialist noted that the short follow‐up of subjects
assigned to surgery may result in an underestimate of the costsand an exaggeration of the benefits of surgery (van Rij, 2006).By the third year, only 40 % of subjects in the study by Michaelset al assigned to surgery were assessed. The editorialist noted,however, that most recurrences are diagnosed later than 3years. Focusing on the short‐term may lead to an under estimate of cost and an over‐estimate of benefit. Theeditorialist stated that prospective comparisons of durability upto 5 years and longer are infrequent and yet by this time therecurrence rate may be as high as 50 %.In patients with varicose veins, leg pain may be associated withsuperficial thrombophlebitis or venous leg ulcers. In evaluatingthe role of varicose vein surgery in treatment of theseconditions, the effectiveness of varicose vein surgery must becompared to conservative management.If the patient is suffering from superficial thrombophlebitis,conservative management is indicated. According to availableguidelines, uncomplicated superficial thrombophlebitis isusually treated symptomatically with heat, simple analgesia,non‐steroidal anti‐inflammatory drugs (NSAIDs), andcompression stockings (SCHIN, 2002). Treatment shouldcontinue until symptoms have completely subsided (usually 2 to6 weeks to subside but the thrombosed vein may be palpableand tender for months). More severe thrombophlebitis, asindicated by the degree of pain and redness and the extent ofabnormality, should be treated by bed rest with elevation of theextremity and application of hot, wet compresses.Leg ulcers arising from venous problems are called venous(varicose or stasis) ulcers. The main conservative treatment hasbeen to apply a firm compression garment (bandage orstocking) to the lower leg in order to help the blood return backup the leg. Cullum et al (2002) conducted a meta‐analysis ofthe literature on the effectiveness of compression bandagingand stockings in the treatment of varicose leg ulcers. Theauthors concluded that compression increases ulcer‐healingrates compared with no compression. The authors also found10 of 95
that multi‐layered systems are more effective than single‐layered systems. High compression is more effective than lowcompression but there are no clear differences in theeffectiveness of different types of high compression. In a meta‐analysis, Nelson et al (2002) found circumstantial evidence ofthe benefit of compression in reducing recurrence of varicoseulcers. The authors also noted that recurrence rates may belower in high compression hosiery than in medium compressionhosiery and therefore patients should be offered the strongestcompression with which they can comply.According to a systematic review of the evidence, pentoxifillinehas also been shown to be effective for treatment of venous legulcers (Nelson et al, 2002). According to the systematicevidence review, compression has been shown to preventvenous leg ulcers. The effectiveness of vein surgery forprevention or treatment of venous ulcers is "unknown" (Nelsonet al, 2002).Beyond conservative therapy, the treatment of varicose veins inthe lower legs includes injection/compression sclerotherapyand surgical stripping or ligation or a combination of theseapproaches depending upon the severity of the condition.Despite many years of experience, there is still a disappointinglyhigh recurrence rate of varices because many patients areinadequately investigated before treatment. As it has beenshown that physical examination alone is unreliable, pre treatment Doppler or Duplex ultrasound examination must beperformed for localization of the sites of incompetence to allowthe individualization of the treatment strategy for each patient.Photographs or office diagrams may be helpful in assessing thesize and extent of the varices.Under established guidelines, the basic tenet of successfultreatment is to eliminate the primary and secondary sources ofthe reflux. These sources are usually a nearby perforator, ormost often a major junction that causes redirected venousreturn through veins with intact valves.11 of 95
Sclerotherapy has been found to be more effective in patientswith dilated superficial or residual varicose veins, recurrentvaricosities or incompetent perforating veins of small tomoderate size (less than 6 mm) without vein reflux. Largevaricosities do not respond as well as small varicosities tosclerotherapy (Rosenberg, 2006; MSAC, 2011; MAS, 2011).Inadvertent intra‐arterial injection has been an untowardsequela of sclerotherapy. Almost all cases of painful varicositiesare associated with junctional reflux. When reflux at thesaphenofemoral and/or saphenopopliteal junctions is present,accepted guidelines provide that sclerotherapy should not beperformed until surgical ligation and division of the junction hasbeen done. The junctions themselves can not be adequatelytreated by sclerotherapy as junctional reflux must be addressedby endovenous ablation methods or surgical ligation orstripping (Jakobsen, 1979; MSAC, 2008; MSAC, 2011). Althoughvaricosities can occasionally be present in the absence or reflux,there is a lack of evidence from reliable clinical studies of theeffectiveness of sclerotherapy in relieving symptomaticvaricosities not associated with junctional reflux. The solerandomized controlled clinical trial (n 25) to address theefficacy of sclerotherapy in varicosities not associated withjunctional reflux (Kalhe and Leng, 2004)evaluated sclerotherapy efficacy in obliterating varicosities, butdid not address its effectiveness at relieving pain. Althoughsclerotherapy can be used to treat visible subcuticular veins(i.e., spider angiomas, and telangiectasias) less than 2.5 mm insize, these small veins do not cause symptoms and theirtreatment is purely cosmetic (MSAC, 2011).Doppler ultrasound is often used in conjunction with other non invasive physiologic testing to characterize the anatomy andphysiology of the varicose vein network prior to injection orsurgical intervention. However, duplex scans are alsosometimes utilized during the sclerotherapy procedure itself.Their purported usefulness in this regard includes thelocalization of deep or inaccessible injection sites, such as whenthere are extensive networks of large deep varicosities, areas ofsignificant reflux between superficial and deep systems, or risks12 of 95
to arterial structures. Ultrasound has also been used tomonitor the effectiveness of compressive sclerotherapy inobliterating the lumen of the target vein and reducingreflux/retrograde flow. However, these indications have notbeen scientifically validated. There is little evidence, in theform of randomized prospective clinical trials, to support thatultrasound makes a significant difference in optimizing outcomeor decreasing complications, from sclerotherapy for varicoseveins, when compared to non‐ultrasound‐guided techniques. Astructured evidence review conducted by the Alberta HeritageFoundation for Medical Research (AHFMR) (2003) concludedthat “the reviewed evidence does not adequately address thequestions; which sclerosant is superior and which techniquewith or without ultrasound guidance is most efficacious.”Venous reflux can be elicited manually by calf musclecompression and release, by the Valsava maneuver, or bypneumatic tourniquet release (Markovic & Shortell, 2014). Ifsaphenofemoral reflux lasting longer than 500 ms is present, thediameter of the great saphenous veins (GSV) is recorded 2.5cm distal to the saphenofemoral junction. The size of the veinhas been correlated with the presence of significant saphenousreflux. The compliant GSV adjusts its luminal size to the level oftransmural pressure, and measurement of its diameter hasbeen shown to reflect the severity of hemodynamiccompromise in limbs with GSV reflux. In a cohort study,Navarro, et al. (2002) evaluated the relationship of GSVdiameter determined in the thigh and calf to clinical severity ofreflux in 112 legs in 85 consecutive patients withsaphenofemoral junction and truncal GSV incompetence. Theauthors stated that they found that the GSV diameter proved tobe a relatively accurate measure of hemodynamic impairmentand clinical severity in a model of saphenofemoral junction andGSV incompete ce, predicting not only the absence of abnormalreflux, but also the presence of critical venous incompetence. AGSV diameter of 5.5 mm or less predicted the absence ofabnormal reflux, with a sensitivity of 78 %, a specificity of 87 %,positive and negative predictive values of 78 %, and an accuracyof 82 %.13 of 95
Ligation and division of the saphenofemoral and/orsaphenopopliteal junction is indicated in patients withsymptomatic varicose veins who have failed conservativemanagement, when reflux of greater than 0.5 seconds isdemonstrated by Doppler examination or Duplex scanning. Theliterature states that operative excision of varicose veins in theleg(s) should be reserved for those that are very large (greaterthan 6 mm), extensive in distribution, or occur in largeclusters. Ligation alone usually results in a high recurrence rateof the varicose vein, which may then require sclerotherapytreatment (MSAC, 2008). Stripping of the greater and/or lessersaphenous vein, performed in conjunction with ligation anddivision of their respective junctions, is indicated when thesaphenous veins themselves show varicose changes (usuallygreater than 1 cm in diameter). Varicose vein surgery and/orsclerotherapy during pregnancy is not appropriate becausedilatation of veins in the legs is physiologic and will revert tonormal after delivery, at which time a more accurate appraisalcan be made. Visible subcuticular veins (i.e., spider angiomas,and telangiectasias) less than 2.5 mm in size do not causesymptoms and their treatment is purely cosmetic.Ambulatory phlebectomy (AP) (also known asmicrophlebectomy) is a minimally invasive procedureperformed under local anesthesia, and is an acceptedoutpatient therapy for the removal of varicose veins. Thistreatment allows excision of almost all of the large varicoseveins except the proximal long saphenous vein, which is better‐managed by stripping. Non‐refluxing varicose veins on thesurface of the leg, not including the saphenous veins, may betreated as an outpatient procedure under local anaestheticusing ambulatory phlebectomy (MSAC, 2011). However,recurrence rates can be high if the source of the reflux is nottreated (MSAC, 2011). The junctions themselves can not betreated with simple phlebectomy as junctional reflux must beaddressed by endovenous ablation methods or rarely bysurgical ligation and stripping (MSAC, 2011; Weiss, 2007).Patients can ambulate immediately after AP. Complicationsassociated with AP include blister formation, localized14 of 95
thrombophlebitis, skin necrosis, hemorrhage, and persistentedema. The use of broad compression pads following APreduces hemorrhage and enhances resorption.The TriVex System (transilluminated powered phlebectomy) isan alternative method of providing ambulatory phlebectomy.This entails endoscopic resection and ablation of the superficialveins using an illuminator and a "powered vein rejector", asmall powered surgical device. In this procedure, veins aremarked with a magic marker. In order to enhance visualizationof the veins, a bright light is introduced into the leg through atiny incision. The powered vein rejector, which has a poweredoscillating end, is then introduced to cut and dislodge theveins. The pieces of vein are then gently retrieved by suctiondown a tube. Transilluminated powered phlebectomy is usuallyperformed in the hospital on an outpatient basis and undergeneral anesthesia or using local anesthesia with sedation.The manufacturer of the TriVex System states that the uniqueillumination feature allows the surgeon to quickly andaccurately target and remove the vein and then visually confirmits complete extraction. The manufacturer claims that this newprocess makes varicose vein removal more effective, completeand less traumatic for patients, by reducing the number ofincisions required to perform the procedure and the duration ofsurgery. The manufacturer also claims that this method notonly reduces the pain associated with varicose vein removal butalso reduces the potential for post‐operative infection. There isinadequate evidence, however, in the published peer‐reviewedmedical literature substantiating these claims. The potentialadvantages of the TriVex System over standard ambulatoryphlebectomy have not been proven. Therefore, the TriVexprocedure should be billed as any other varicose vein removalprocedure.The term endovenous catheter ablation (EVCA) has been usedto refer to the several new catheter based minimally invasivealternatives to surgical stripping, including laser ablation andradiofrequency ablation. Endovenous catheter ablation and15 of 95
surgical ligation/stripping are indicated for treatment of thesame general population: patients in whom the great and/orsmall saphenous veins have reflux or incompetence of 0.5seconds or longer demonstrated on duplex scanning, andvaricose vein symptoms significantly impinge on quality of life(MSAC, 2011). These patients have exhausted conservativetreatment measures, and sclerotherapy is considered unlikelyto provide successful results. Endovenous laser ablation andradiofrequency ablation are essentially identical except for theuse of different specialized equipment and catheters, withthermal energy delivered through either a radiofrequencycatheter or laser fiber (MSAC, 2011). The objectives of the twotreatments are the same, being the destruction or ablation of arefluxing vein or segment of vein via application of thermalenergy. The procedure to place the catheter within the vein isthe same for radiofrequency ablation and endovenous laserablation, also both procedures are conducted under duplexultrasonography guidance (MSAC, 2011). The physiologicalmechanism of vein ablation is also the same, with thermalenergy producing endot
Varicose vein surgery is one of the most commonly performed cosmetic procedures in the United States. Most varicose veins do not require medical treatment (Tapley et al, 2003). In some cases, however, the circulation may be hindered enough to cause swelling of the foot and ankle, discomfort, a tingling sensation, or a feeling of heaviness.