Transcription
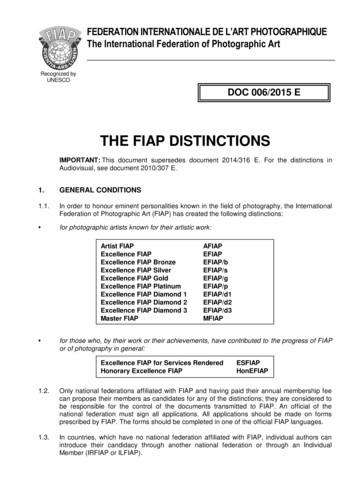
PURSUIT OF EXCELLENCEPUBLISHED FOR THE NURSING STAFF OF MIAMI CHILDREN’S HOSPITALVolume 9 Issue 22008 MCH Nurse of the Year2008 MCH Nurse Unit WinnersJanice Serrano, RN, BSNRookie of the YearEmily Zubira, RN, BSNCICUTeresa SanchezLPN of the Year (Now RN)Joanne Nieves, MSN, ARNP Alison Scheflow, RN, BSN, CCRNEvidence Based Practice WinnerResearch WinnerResearch WinnerReyna AmadorSupport Staff of the YearRochelle Gabas, RN, BSN2EMonica Brown, RN, MSN, CPN2 NEVivian Gimon, RN, CPN3EClaudia Alfonso, RN3SMonica Hawkins, RN, BSNAfter HoursIrene Bowers, RNAmbulatoryDavid Pastor, RN, BSN, CPNER/Rapid CareLisa Morgan, RN, MSNFloat/SREnio Ortega, RN, BSNORMaria Ojeda, RNPACUSandra Wiley, RN, BSNPICUAlicia Lue, RNIV TeamNova Franklin-Bremmer, RNPsychViviana Gonzalez, RN, BSNNICUCharity Zayas, RNQuality/URAdam Fader, RN, BSN3 NEPat Thorpe, RN, BSNLeader of the YearTracee Smith, RN, BSN3NMargot Sarratea, RN, CPN Carmen Rodriguez, RN, BSN, CPN Jane Salvaggio, MSN, ARNPSouth DadeNursing Support Dept.MRI/RadiologyDeDe Lichtman, RN, BSNPCC
From the Desk of Jackie GonzalezDear Nursing Team:I cannot fully express how proud I am of this nursing staff. I received the news along with many of you in theauditorium that MCH received its first redesignation as an ANCC Magnet facility. The process was rigorous andthe standards continue to be set higher, but you all demonstrated very clearly to the appraisers why MCH is truly a“magnet” destination for nurses to practice. What we did not find out that day, but received in our written report, isthat we had no deficiencies! Not only that, but we received 10 citations for exemplary practice in the following areas: Force 2 - Organizational Structure -“embraces everyone to do a good job ” Force 3 - Management Style - “continually strives to keep nurses engaged and stimulated in their nursing practice by setting highquality standards.” Force 4 - Personnel Policies & Programs - “direct care nurses are extremely involved in recruitment and retention activities” Force 5 - Professional Models of Care - “ strong examples of innovations by the direct care nurses Family centered care modelincluding bedside report NICU breast feeding room ED quiet room.” Force 6 - Quality of Care - “demonstrates its commitment to safety for the patients, families and staff Force 8 - Consultation & Resources - “ professionalism of the nurses reaches out much farther than the walls of the [hospital].Their impact on pediatric nurse is felt by many throughout the nation as well as worldwide.” Force 10 - Community & the Health Care Organization - “hosts over six camps throughout the year for special needs andchronically ill children and the families which facilitates camaraderie,support and resources.” Force 11 - Nurses as Teachers - “The organizatio n’s innovative, creative and effective academic practicum program is an exemplar.” Force 12 - Image of Nursing - “brought pride and recognition of nursing to all parts of the organization ”How incredibly positive and strongly written this was about all of you! I know you are as proud of your practice as I am and mostimportantly, the children and their families deserve our best and nothing less, which you give every day.On another note, while I know September and December seem far away at the moment---please watch for the Pediatric Conferenceand a special December celebration event! We have a lot to celebrate.Have a wonderful summer and enjoy your family and friends as you spend the time with them! Thank you for all you do for thenursing profession and for MCH.Jackie Gonzalez, ARNP, MSN, CNAA, BC, FAANSenior Vice President / Chief Nursing OfficerCongratulations on Renewed ‘Magnet’ DesignationBy Debbie Hill RodriguezThe nurses at Miami Children’sHospital have done it again! TheAmerican Nurses CredentialingCenter’s (ANCC) MagnetRecognition Program for excellence innursing services has once again designatedMiami Children’s as a Magnet hospital.According to the ANCC, the leadingnursing credentialing organization in theUnited States, Magnet designation iswidely accepted as the gold standard ofpatient care. Only 3 percent of hospitalsnationwide have achieved Magnetdesignation. Miami Children’s Hospitalfirst achieved Magnet recognition in 2004.“The nursing staff at Miami Children’shas a long-standing tradition of leadership, clinical excellence, collaboration andconcern for our patients and their safety.Our nurses are the heart and spirit of thishospital and Magnet recognition is a genuine reflection of their concern for the wellbeing of the children entrusted to our care,”said Jackie Gonzalez, MSN, ARNP, SeniorVice President and Chief Nursing Officer.2The Magnet Recognition Program recognizes excellence and professionalism innursing. Applicants undergo an extensiveevaluation, and members who are awardedMagnet status must continue to maintainrigorous standards as part of their four-yeardesignation.To reapply for and receive Magnetstatus for an additional four years is confirmation of the hospital’s resolve to deliverthe highest level of care in nursing today.Research shows that Magnet hospitals aremore effective at attracting and keepingquality nurses.
Celebrating Nurses WeekBy Bing Wood, ARNP, MSNChair, Recognition CouncilAMiami Children’s Hospital committee of 35 staffmembers worked hard for eight months to plan anelaborate program of Activities for the staff to enjoyduring the May 4-10 Nurses Week celebration.The special event also provided an opportunity to recognizestaffers whose contributions to the nursing profession havemade an impact in Miami Children’s Hospital. More than 200nominations were received, and after reviewing all nominations,the committee chose the following winners for the year:2008 MCH Nurse of the YearEmily Zubira, RN, BSNCICU2008 MCH Nurse Unit WinnersRochelle Gabas, RN - 2 EMonica Brown, RN - 2 NEVivian Gimon, RN - 3 EAdam Fader, RN - 3 NETracee Smith, RN - 3NClaudia Alfonso, RN - 3SMonica Hawkins, RN - After HoursIrene Bowers, RN - AmbulatoryDavid Pastor, RN - ER/Rapid CareLisa Morgan, RN - Float/SRAlicia Lue, RN - IV TeamViviana Gonzalez, RN - NICUEnio Ortega, RN - ORMaria Ojeda, RN - PICUNova Franklin-Bremmer, RN - PsychCharity Zayas, RN - Quality/URMargot Sarratea, RN - MRI/RadiologyCarmen Rodriguez, RN - South DadeJane Salvaggio, MSN, ARNP - Nursing Support Dept.Diane Lichtman, RN - PCCJanice Serrano, RN - Rookie of the YearTeresa Sanchez - LPN of the Year (Now RN)Pat Thorpe, RN - Leader of the YearJoanne Nieves, MSN, ARNP - Research WinnerAlison Scheflow, RN, BSN, CCRN - Evidence Based PracticeWinner, Research WinnerReyna Amador - Support Staff of the Year MCH Nurse of the year award was presented to Emily Zubiria,staff RN from Cardiac ICU. This individual consistently displaysdedication to excellence in an area of expertise beyond the scope ofany job or specific endeavor through commitment to the professionof nursing and a sense of community service. She serves as aninspiration to others in an effort to improve the quality of healthcare and discover new ways to assist those in need and displaysMCH nurses on the field at the May 3 Florida Marlins baseballgame in honor of Nurses Week. From top to bottom are JohnyMok, our 2007 Nurse of the Year; Lillian Bell, 3NE manager;and Vicki Rosenfeld 3East manager.continued on page 123
DAISY AwardWinnersApril Winner for 2008Vivian Gimon, RN3 EastMay Winner for 2008Arsenio LatorrePICUJune Winner for 2008Rico Trespico2 EastJuly Winner for 2008Christina ForcinePICUChild Passenger Safety WeekBy Candace Pineda, RN, BSN, CPNWith the excitement of school beginingagain, comes the increased morningand afternoon traffic, as well as theincrease risk for injury and death amongchildren riding unrestrained in vehicles.According to Safe Kids Worldwide:“Riding unrestrained is the single greatestrisk factor for death and injury among childmotor vehicle occupants. Among children ages14 and under killed in motor vehicle crashes asoccupants in 2002, 50 percent were not usingsafety restraints at the time of the collision.Misuse is common. An estimated 85percent of children who are placed in childsafety seats and booster seats are improperlyrestrained.Misuse includes, but is not limited to,using an inappropriate seat for a child’s age andsize, placing an infant under 1 year or under20 pounds in a forward-facing seat, not securingthe seat tightly in the vehicle and not securingthe child correctly in the seat.The back seat is safest. It is estimated thatchildren ages 12 and under are up to 36 percentless likely to die in a crash if they are in a rearseat of a passenger vehicle. “Florida laws support child passenger safetywith the recent passing of the HB 619-ChildRestraint Requirements. This new law changesthe age requirement of children from 5 to 7years of age or younger who must use crashtested, federally approved child restraint deviceJoin the Squeaky Clean TeamSqueaky Clean is a program topromote hand washing and handsanitizing among staff and visitorsto optimize patient care and wellbeing. It is designed to address a NationalPatient Safety Goal. Here’s how it works:MCH caregivers and staff are reminded to model hand hygiene by washinghands or using hand sanitizer wheneverentering a patient’s room, exam room orother care area. When approaching a patient, caregivers/staff members should say,“I am cleaning my hands for your safety.Please remind others to do the same.” Thisthat is appropriate for height & weight of child.It also adds child booster seat as option forchildren aged 4 through 7.To increase injury prevention and awarenessfor parents and families, SafeKids Worldwidehas designated a week in September as ChildPassenger Safety Week. This years eventswill be held September 21-27, 2008. SafeKidsMiami-Dade County, together with MCH’sTrauma Services department, will be holdingcar seat inspections on the following datesand times:9/19/2008 from 1:00 p.m. to 3:00 p.m.Toy R Us8789 SW 117 Ave., Miami FL, 331839/20/2008 from 11:00 a.m. to 3:00 p.m.Potamkin Chevrolet16600 NW 57 Ave., Hialeah FL, 330149/27/2008 from 11:00 a.m. to 3:00 p.m.Miami Children’s Hospital3100 SW 62nd Ave., Miami, FL 33155During the events, Child Passenger SafetyTechnicians will check the car seats for defects,recalls, installation, and fit. For more information or for any questions on child passengersafety or injury prevention, please contact theTrauma Services Department at (305)663-6800.Correctionrole modeling will encourage families andvisitors to practice hand hygiene as well.The program empowers our inpatientchildren. When a patient sees a caregiveror other staff member practicing hand hygiene, the patient can award the employeea ticket from the Squeaky Clean bookletgiven to each child after admission.Employees turn in award tickets totheir manager or supervisor. Prizes willbe presented to employees who achievespecific “Squeaky Clean” goals. Thanksfor being part of the Squeaky Clean Team!4In our last issue, thewrong author was noted forone of the articles. “Did youKnow? A Solution to Enhancethe Knowledge of Nurses”was written by AlisonScheflow, RN, MS, CCRN.We apologize for the error.
Pat Dean – Epilepsy Foundation’s Volunteer of the YearPat Dean, MSN, ARNP, MCHclinical nurse specialist and boardpresident of the Epilepsy Foundation of Florida was recognizedas Volunteer Leader of the Year at thefoundation’s fourth annual LeadershipConference in September. The award isgiven to an individual who has made anoutstanding contribution to the epilepsyfield through volunteer time or fundraising. Pat has made many contributions,and is an integral part of epilepsy sessions at camp and knows firsthand thelife-changing impact Camp Boggy Creekhas on the children who attend. “Pat isone of the most energetic, passionate andcommitted supporters we have,” said JuneClark, Camp Boggy Creek ExecutiveDirector. “She is well-deserving of thisaward. Kudos, Pat!”What’s Bubbling in the NICU?By Joy Ortiz, RNAnyone floating to NICU these daysor just “passing through “ mayfind something new and interesting. Containers of bubblingwater are now placed next to some of oursmallest babies following clinical information from the Morgan Stanley Children’sHospital of New York (MSCHNY).Prior to this, the main type of ventilatory assistance offered to our babiesincluded INCA nasal CPAP, conventionalmechanical ventilation and high frequencyoscillation. However, recently the neonatologists in the NICU were introduced to anew type of bubble CPAP, gentle enoughfor even the most extreme premature infants. At MSCHNY, preferential CPAP hasbeen associated with lower incidence ofchronic lung disease in premature infantsthan in units that prefer modalities primarily utilizing endotracheal intubation.The bubble CPAP device may be usedon many infants with differing diagnoses,including respiratory distress syndrome,transient tachypnea of the newborn, PDA,pulmonary edema and apnea of prematurity, among others. Additional uses by allinfants for respiratory support aftermechanical ventilation have also beenshown effective in the recovery period.Benefits include increase in transpulmonary pressure and functional residualcapacity. The bubble CPAP device hasbeen shown to prevent alveolar collapse, decrease intrapulmonary shunt andincrease lung compliance. It conservessurfactant in the newborn and decreasesthe work of breathing. It also preventspharyngeal wall collapse and stabilizes thechest wall, splinting the diaphragm andstimulating lung growth. Due to the gentlerhythmic bubbling action, the bubbleCPAP device has a high frequencyventilation (HFV) effect.5To begin bubble CPAP, the physicianindicates to the nurse that bubble CPAP isneeded for that patient. Orders are writtenfor bubble CPAP with a particular pressuresetting specified as cmH2O, usually 5 to 7cm H2O. The nurse notifies the respiratorytherapist, who commences set up at thebedside. After oxygen tubing is connectedto a flow meter and blender, the tubingis connected to a heated humidifier. Thehumidifier is turned on and a second corrugated tube is placed into a water-filledoutlet container, usually 5 to 7 cm belowthe water surface, depending on the cm ofH2O CPAP pressure the infant requires. Asair flows through the water into the tubing,it creates a gentle bubbling sensation forthe infant. The nurse verifies the CPAP isworking by observing for continued bubbling in the outlet bottle.Bubble CPAP is one more way theNICU is committed to bringing the verybest care to the tiniest children.
Cancer Survivors Day PicnicBy Sarah Taylor, RN, BSN, CPONNurse Manager, Hematology/OncologyOn June 1, Miami Children’sHospital joined other institutionsaround the nation to celebrateNational Cancer Survivors Day.Nearly 200 patients and their familiesenjoyed food, carnival style games, facepainting and the opportunity to throw piesat one of their doctors (Dr. Khatib).Participating cancer survivors rangedfrom 15 years to 1 month old. It was agreat opportunity for our nursing staff andpatients to interact in a fun and pain-freeenvironment. It is always refreshing andre-energizing for the nurses to see that wecan make a difference, especially in thelives of patients and their families facingthe diagnosis of cancer.Changes by the Florida Board of NursingBy Linda BrunsonDirector, CE BrokerThe Florida Board of Nursing hasmade several changes that affectCNA in-service renewal requirements. Half of the CNAs wererequired to renew for a 3-year certificationperiod. The Florida Board of Nursingrenewal fee was 80 instead of the normal 55 for two years. This was done to splitup the 140,000 CNAs into two CNArenewal periods. Starting December 2009,all CNAs will not renew on the same date.The in-service renewal requirement(64B9-15.001 F.A.C.) for this onethree-year certification period is: 12 in-service hours each calendaryear Each of the seven required topicsmust be fulfilled within the three-yearcertification periodFollowing this one-time three-yearcertification period, the CNA in-servicewill align with his/her Florida Board ofNursing certification period.6CNAs with the three-year certificationperiod will have four transcripts in CEBroker – one for each of the three calendaryear 12-hour requirements and one for therenewal required topics.To view CNA renewal requirements onthe Florida Department of Health website,please go to http://www.doh.state.fl.us/Mqa/cna/cna ceu.html.If you have any questions, please call1-877-434-6323 (877-i-find-CE).
Be Prepared: Hurricane Season is HereHurricane season is here. Don’t becaught off guard. Whether youserve on the Alpha or Bravo shift,you should have a hurricane planand supplies in place so that you are readyin the event of a storm.To ensure that you are prepared, theFederal Emergency Management Agency(FEMA) has recommended that you havea family preparedness plan in place whichwill sustain your family for three days.Here are some guidelines from theNational Oceanic and AtmosphericAdministration (NOAA):Family Disaster Plan Discuss the type of hazards that couldaffect your family. Know your home’svulnerability to storm surge, flooding andwind. Locate a safe room or the safest areasin your home for each hurricane hazard.In certain circumstances the safest areasmay not be your home but within yourcommunity. Determine escape routes from yourhome and places to meet. These shouldbe measured in tens of miles rather thanhundreds of miles. Have an out-of-state friend as a familycontact, so all your family members havea single point of contact. Make a plan now for what to do withyour pets if you need to evacuate. Post emergency telephone numbers byyour phones and make sure your childrenknow how and when to call 911. Check your insurance coverage - flooddamage is not usually covered byhomeowners insurance. Stock non-perishable emergency supplies and a Disaster Supply Kit (see nextcolumn). Use a NOAA weather radio. Rememberto replace its battery every 6 months, asyou do with your smoke detectors. Take First Aid, CPR and disasterpreparedness classes.Disaster Supply Kit Water - at least 1 gallondaily per personfor 3 to 7 days Food - at least enough for3 to 7 days non-perishable packaged or canned food /juices foods for infants orthe elderly snack foods non-electric canopener cooking tools / fuel paper plates / plasticutensils Blankets / Pillows, etc. Clothing - seasonal / rain gear/sturdy shoes First Aid Kit / Medicines /Prescription Drugs Special Items - for babies and the elderly Toiletries / Hygiene items /Moisture wipes Flashlight / Batteries Radio - Battery operated and NOAAweather radio Telephones - Fully charged cell phonewith extra battery and atraditional (not cordless)telephone set Cash (with some small bills) and CreditCards - Banks and ATMs may not beavailable for extended periods Keys Toys, Books and Games Important documents - in a waterproofcontainer or watertight resealableplastic bag insurance, medical records, bank account numbers, Social Security card,etc. Tools - keep a set with you during thestorm Vehicle fuel tanks filled Pet care items proper identification / immunization records / medications ample supply of food and water a carrier or cage muzzle and leash7MCH Hurricane UpdatesDuring and after the approach of ahurricane, MCH employees should checkthe hospital’s Hurricane Hotline and/orPortal for updates on shift changes andother important details. The hotlinenumber is 305-667-1957. The MCH Portalcan be accessed from www.mch.com, byclicking on the physician and employeelogin link at the bottom of the home page.Your standard login identification andpassword will gain you access.Miami-Dade County Office ofEmergency ManagementContact Information: www.miamidade.gov/eoc will provideyou with the following: Evacuation zones Flood zones Law enforcement & firedepartment contact phone numbers Government Services Animal Shelters Registration for electricallydependant & oxygen dependantcommunity patients
Critical Thinking: What Would You Do?By Linda Nylander-Housholder, MSN, ARNP, CCRNYou are called to your patient’sroom by her mom. When youarrive, you note a 4-year-oldgirl with a tracheotomy who isagitated, cyanotic and has intercostal, aswell as supra and substernal retractions.Breath sounds are decreased bilaterallyand air entry is poor. Heart rate 200, BP110/78, R 67. She weighs 15 Kg and hasno known allergies.What should you do? ABCs- position open airway, give100% 02 to trach if no improvementthen suction, bag with 100% 02,prepare to change trach (Were there2 trachs with guides bedside 1 samesize, 1 smaller) Place on monitors, EKG and 02 sat Obtain IV access – send blood gasIf trach fell out and stoma was constricted so you were unable to replacetrach, what would you do now? ABCs prepare to BVM with 100 %02 while covering stoma Place small tube in ostomy andattempt to slide trach over tubing Ready for intubation Call anesthesiaDid you think airway and common causeof airway distress in trached patients ismucus plugging?Did you remember to preoxygenate and tooxygenate during suctioning procedure?Did you think how and when to attempttrach change-out?Did you think of possible complicationsof changing out trach, such as bleeding,pneumonia, malplacement, or perforationof trach?Did you remember what to do if you couldnot reinsert trach, and to cover stoma ifyou had to BVM the patient to prevent airleak via stoma?MCH Nurses Experience NTIBy Ingrid Gonzalez, RN, MSN, CPN and Carla Leblanc, RN, MSN, CPNDuring the first week of May,Miami Children’s nurses hadan opportunity to experienceAACN’s National TeachingInstitute and Critical Care Exposition (NTI) in Chicago. Nurses from bothPICU and CICU attended this prestigiousconference, which attracted an estimated9,000 acute and critical care nurses fromaround the nation. This conference provided a wide variety of resources to targetall types of learners. There were manypre-conference activities, such as reviewcourses, sitting for exams in your specialty(CCRN, CCNS, PCCN and ACNPC) orsub-specialty certifications. Therewas also a self-study pavilion withabout 60 computers that offeredonline modules for CE credits.There were also networking opportunities to assist participants inaccessing comprehensive resources designed to optimize theirpatient care outcomes.There were many vendorexhibitions that awarded nurseswith gifts such as pens if theywanted to learn about the products. Also, nurses were awardedCE credits for 30-minute sessionsreviewing clinical trials. The vastexhibition center was the lengthof three football fields.At mid-week, the expositioncenter and the poster sessionswere revealed to participants.The poster sessions were dividedinto two categories: researchand creative solutions. One of our MCHnurses, Alison Scheflow, presented hercreative solution poster presentation, titled8“Did You Know?” and there were manymore innovative ideas presented by otherinstitutions.After attending many different conferences, NTI was one of the most well organized venues by far. From the registrationprocess to the shuttle service from hotelsto the convention center, there was never adelay. In addition, our nurses were able todocument their contact hours online priorto leaving the conference. This is definitely an event that all critical care nursesshould experience at least once in theirprofessional careers.
New Changes to Central Line Heparin Flush DosingBy Lourdes Fernandez, RN, MSN and Carla Leblanc, RN, MSN, CPNAtask force at Miami Children’sHospital recently reviewed ourcurrent practices on heparin use inrelation to central venous accessdevices. The safety practices of heparinwere a topic of discussion at the Medication Safety Committee, where the idea ofa task force was originally formulated.Pharmacy and nursing collaborated to review literature and other hospital practicesin order to maximize patient outcomes anddecrease the risk of overdosing patientswith heparin.The first step taken to decrease theamount of heparin usage was to removeheparin from the override list in Pyxis. Itnow requires a physician order for withdrawal from Pyxis. Heparin was alsoadded to the inventory list that is checkedby charge nurses each shift.Heparin flush dosing changes weremade to the various central lines used atMCH. Most venous access devices willnow require 10 units/ml instead of the100/ml dose that was previously in use.These changes were formally approvedby the Pharmacy and Therapeutics Committee and Medical Executive Council inApril, 2008. A clinical practice alert wascreated by the Clinical Practice Committeeand in-services were done on each unit.To monitor the effectiveness of thischange, data on TPA usage prior to andafter the heparin dosing changes will bereviewed. This will help determine if thedosing changes impacted the patency of thevenous access devices. Studies have shownthat the best practice for flushing centrallines is to instill normal saline (instead ofheparin) vigorously using a 10 ml syringe,a practice that we hope to eventuallyimplement. Please review the Central Lineand PICC Line policy for specificinformation on the new guidelines.9
Join a Professional Organization in the NICUBy Debra S. Langer, RN, BSN, CLNC, BSWant to avoid that last minute rushfor CEUs before your RN licenseexpires? (And earn APEX pointsas well?) Become a member of aprofessional organization!We in the NICU have SEFANN – theSouth East Florida Association of Neonatal Nurses. In order to become a memberof SEFANN, there is a 15 membershipfee and one must first become a memberof NANN, the National Association ofNeonatal Nurses. I know, I know, 99 is achunk of change but, guess what.that is27 cents a day! Where else can you havedinner with friends (we all have at leastone commonality), listen to an area professional speak on a topic that you mightbe able to incorporate into your nursingpractice, and earn a CEU? All for about 27cents a day!SEFANN meets on the fourth Tuesday of every other month. That’s 6 CEUsearned per year, just for attending all themeetings (one CEU each). Attend the twoday SEFANN conference and you earn 15CEUs. Attend the NANN conference andthat is approximately 21.5 CEUs more!Now you need only worry about completing those requirements that the statemandates.NICU. At our meeting, I took a poll of thenurses from the area hospitals and learnedhow they were handling the matter. It wasthat easy.And think of the other benefits. FromNANN you receive: Advances in NeonatalCare: Official Journal of the National Association of Neonatal Nurses, NANN Central, a news poster, discounted admissionto the NANN conference, access to theNANN website, an opportunity to belongto a Specialty Interest Group (SIG), whichis a group of neonatal nurses who sharea specific interest and you are eligible tojoin your state/regional chapter.SEFANN is also all about communityinvolvement. Our members volunteerto help the March of Dimes launch theirevents and we are a corporate sponsorat the March for Babies event (formerlyknown as Walkathon). Each holidayseason we donate toys to an organizationhelping underprivileged children in theSouth Florida area. How happy we are tosee the “loot” we collect and realize thatwe have helped to put the smiles on manysmall faces.SEFANN is our regional chapter. Wehave members from Miami-Dade andBroward Counties, with past membersliving in Ft. Myers and even the state ofTennessee, still checking in to learn whatwe are up to. And so interesting for us tolearn what they are up to!That’s what I like about SEFANN. Thenetworking! I remember when we hadquestions about breastmilk storage in theSEFANN also offers three scholarships( 300 each) to active members to use forparticipation in either our local conferenceor for the national conference.Now does this not sound like a greatthing to do for yourself as a professionalindividual? And each nursing disciplinehas an organization similar to this. Findyours and join today!Use of Metered–Dose Inhalers (MDIs) in theEmergency DepartmentBy Debbie Salani, ARNP, MSN, Connie Chan, PharmD, and Javier Hernandez, RRTThe Emergency Departmentrecently embarked on a clinicalpractice change based on theevidence available when caringfor children with asthma. In collaborationwith the medical/nursing staff, pharmacyand pulmonology department, the usageof MDIs was introduced in theEmergency Department.Inhaled brochodilators are one of themost frequently prescribed medications forchildren hospitalized with respiratory conditions. For many years, the most common treatment for patients with asthmaand bronchiolitis were aerosol treatmentwith various bronchodilators. However,there is a large body of literature thatindicates that the metered dose inhalerswith valved holding chambers have beenshown to be equivalent to small volumenebulizers for the delivery of bronchodilators in children.In the past, it was assumed that youngchildren would be unable to use the MDIsbecause they could not coordinate theinhaler and these devices would not be effective in their treatment. However, nowthat we have valved holding chambersavailable in a variety of sizes, childrenwith asthma can effectively be treatedusing MDIs.10Currently, the Emergency Department is using the MDIs with children withrespiratory conditions who are 3 years ofage or greater. There are two aerochambersizes being utilized: medium for ages3 -12 and large for patients older than12 years.The MDIs/aerochambers are packagedtogether. Upon discharge, the ED staff willlabel the medication with the child’s nameand the dosage and send the family homewith the inhaler package. This has been agreat satisfier for patients and families.
The New Aquatic Facility at Miami Children’s HospitalDan Marino CenterBy Charina M. Desaulniers, PT, DPTRehab Supervisor and Doctor of Physical Therapy, Miami Children’s Hospital Dan Marino Cen
Diane Lichtman, RN - PCC Janice Serrano, RN - Rookie of the Year Teresa Sanchez - LPN of the Year (Now RN) Pat Thorpe, RN - Leader of the Year Joanne Nieves, MSN, ARNP - Research Winner Alison Scheflow, RN, BSN, CCRN - Evidence Based Practice Winner, Research Winner Reyna Amador - Support Staff of the Year