Transcription
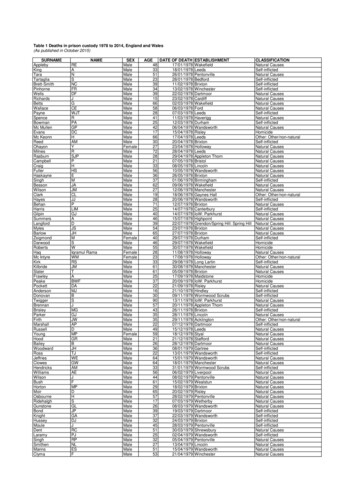
1Clinical Summary GuideStep-by-Step:Male Genital ExaminationExamination of male genitals and secondary sexual characteristics.Testicular volumeTesticular volume is assessed using an orchidometer; a sequentialseries of beads ranging from 1 mL to 35 mL (see Image 1).Testicular volume is measured using the following steps:1. Conduct the examination in a warm environment, with thepatient lying on his back2. Gently isolate the testis and distinguish it from the epididymis.Then stretch the scrotal skin, without compressing the testis3. Use your orchidometer to make a manual side-by-sidecomparison between the testis and beads (see image 2)4. Identify the bead most similar in size to the testis, whilemaking allowance not to include the scrotal skin.Normal testicular volume rangesChildhoodPubertyAdulthood 3 mL4-14 mL15-35 mLImage 1 – OrchidometerWhy use an orchidometer?Clinical notes Asymmetry between testes is common (e.g. 15 mL versus20 mL) and not medically significantTesticular volume is important in the diagnosis of androgendeficiency, infertility and Klinefelter syndrome. Asymmetry is sometimes more marked following unilateraltesticular damage Testes are roughly proportional to body size Reduced testicular volume suggests impaired spermatogenesis Small testes ( 4 mL) from mid puberty are a consistent featureof Klinefelter syndromeExamination of secondary sexual characteristicsGynecomastia Gynecomastia is the excessive and persistent developmentof benign glandular tissue evenly distributed in a sub-areolarposition of one or both breasts (see image 3)Image 2 – Example of 30 mL and 4 mL adult testis Can cause soreness and considerable embarrassment Common during puberty, usually resolves in later adolescence Causes include marijuana, androgen abuse, abnormalliver function Distinguish glandular tissue from sub-areolar fat inobese subjects Rare secondary causes include hypothalamic/pituitary andadrenal/testis tumours (oestrogen excess) Rapidly developing gynecomastia may indicatetesticular tumour In contrast to gynecomastia, breast cancer can be locatedanywhere within the breast tissue and feels firm or hardOnset of puberty Average onset is 12-13 yearsVirilisation Facial and body hair development Muscle development Penile growthImage 3 – Gynecomastia(Photo courtesy of Mr G Southwick, Melbourne Institute ofPlastic Surgery)
Examination of testis and scrotal contentsTestisEpididymisGently palpate the testisbetween your thumb andfirst two fingers.If a testis cannot be felt, gentlypalpate the inguinal canal to see iftestis can be ‘milked’ down.Examine the testis surface forirregularities. It should be smooth, witha firm, soft rubbery consistency.Note: Atrophic testes areoften more tender to palpation than normal testes.Note: Testis retraction can be causedby cold room temperature, anxietyand cremasteric reflex.Note: A tumour may be indicated by deepor surface irregularity, or differences inconsistency between testes.Locate the epididymis,which lies along theposterior wall of the testis.It should be soft, slightlyirregular and non-tender totouch. Tenderness, enlargement or hardening can occur as a result of obstruction(vasectomy) or infection. This can be associated with obstructive infertility. Cysts in the epididymis are quite common. These are something mistaken fora testicular tumour.Locate the vas deferens,a firm rubbery tubeapproximately 2-3 mm indiameter.Nodules/thickening around the vas deferens endsmay be apparent after vasectomy.The vas deferens shouldbe distinguished from theblood vessels and nerves ofthe spermatic cord.Absence of the vas deferens is a congenital conditionassociated with low semen volume and azoospermia.Vas deferensVaricocelePerform examinationwith the man standing.A Valsalva manoeuvre orcoughing helps delineatesmaller varicoceles.Indicators include: Palpable swelling of the spermaticveins above testis Swelling is usually easy to feeland can be compressed withoutdiscomfort Nearly always on left side Associated with infertilityPenisSpermaticveinTestes(Photo courtesy of Prof. D de Kretser)Examination of penile abnormalitiesHypospadiasPeyronie’s diseaseAbnormal position ofmeatus on the undersideof the penile shaft. Maybe associated with anotched penile head.Fibrous tissue, causingpain and curvature ofthe erect penis.Check for tendernessor thickening.MicropenisPhimosisUrethral strictureMay indicate androgendeficiency prior topuberty.The foreskin cannotbe pulled back behindthe glans penis. Can benormal in boys up to 5-6years.Abnormal urethralnarrowing, which altersurination. Can be causedby scar tissue, disease orinjury.HypospadiasPeyronie’s DiseasePosition of urethral openingGlans penisGlanularCorpuscavernosumSubcoronalFibrous plaquePenileScrotalPerinealUrethra(Photo courtesy of Dr M Lowy, Sydney Centre for Men’s Health)Date reviewed: March 2018 Healthy Male (Andrology Australia) 2007
2Clinical Summary GuideMale Child and AdolescentGenital ExaminationExamination of male genitals and secondary sexualcharacteristics in children and adolescence.When should I perform an examination?A physical examination including male children and adolescentsis vital for the detection of conditions such as testicular cancer,Klinefelter syndrome, penile and hormonal abnormalities.How do I approach an examination with youngpatients?Good communication can assist the process of physicalexaminations with children and adolescents. Communicate with both the patient and his parents, usingsimple language and visual aids if available Explain why you need to perform the examination and ask forpermission to proceed Allow the patient to ask questions and express any discomfortbefore/during the examination When it seems appropriate, humour can be used (particularlywith children) to reduce anxiety, foster rapport and improvecooperation before or during the examination If you refer the patient to another specialist, take the time toexplain why, and what may be involvedChildhood history and examinationPresentation with acute testicular pain Testicular torsion Refer immediately for evaluation for possible surgeryHistory Undescended testes (increased risk of testicular cancer,and associated with inguinal hernia) Inguinal-scrotal surgery or hypospadiasTesticular examination Undescended testes Testicular volume: Normal childhood (pre-pubertal) range oftesticular volume is 3 mLPenile examination Hypospadias MicropenisWhen is it best to perform an examination?1. Part of a standard health check-up with new or existingpatients2. On presentation of relevant disorders or symptoms, including:Risk FactorAssociated disorderUndescended testes as an infantTesticular cancerDelayed pubertyAndrogen deficiencyGynecomastiaAndrogen deficiency,Klinefelter syndrome,Testicular cancerPast history of testicular cancerTesticular cancerAcute testicular - groin painTesticular cancerTesticular pain or lumpsTesticular torsionAdolescent history and examinationPresentation with acute testicular pain This is a medical emergency Later follow up review (e.g. epididymo–orchitis)History Undescended testes Pubertal development Testicular trauma, lump, cancer Gynecomastia Prior inguinal-scrotal surgery or hypospadiasTesticular examination Testicular volume-- Normal pubertal range is 4-14 mL-- 4 mL by 14 years indicates delayed or incomplete puberty-- Small testes ( 4 mL) may suggest Klinefelter syndrome-- Adult testis size is established after completion of puberty Scrotal and testicular contents-- Abnormalities in texture or hard lumps (tumour or cyst)Penile examination Hypospadias Micropenis Infections (STI) or inflammation Foreskin: balanitis, phimosisExamination of secondary sexual characteristics Gynecomastia: excessive and/or persistent breast development Delayed puberty (average onset is 12-13 years). Indicators:-- Short stature compared to family, with reduced growthvelocity-- Absent, slow or delayed genital and body hair developmentcompared to peers-- Anxiety, depression, school refusal, or behaviour change inschool years 8-10 (age 14-16 years)
Puberty: delayed onset or poor progressionTesticular massPresentationPresentation Short stature compared to family Painless lump Absent, slow or delayed genital development Self report, incidental Anxiety, depression, school refusal, behaviour change Past history undescended testes (cancer risk)( ) Other features Consider possibility of epididymal cyst Headache/visual change (CNS lesions)Primary investigations Inability to smell (Kallmann’s syndrome) Testicular ultrasound Behavioural or learning difficulty (47,XXY)Treatment and specialist referral Unusual features (rare syndromes) Refer to uro-oncologistPrimary investigations Offer pre-treatment sperm cryostorage Growth chart in context of mid parental expectation(velocity, absolute height)Refer to Clinical Summary Guide 6: Testicular Cancer Penile size (standard growth chart)Penile abnormality Testicular volume ( 4 mL: puberty imminent)Presentation Bone age HypospadiasSpecific investigations Micropenis LH/FSH (may be undetectable in early puberty, but if raised canbe useful) Phimosis Total testosterone level (rises with onset of puberty) Karyotype (if suspicion of 47,XXY)Treatment and specialist referral Refer to urologist for investigation and treatment planGeneral investigations Refer to paediatric endocrinologist for investigation ofmicropenis U&E, FBE & ESR, coeliac screen, TFTGynecomastiaTreatment and specialist referralPresentation in adolescence If all normal for prepubertal age, observe for 6 months Excessive and/or persistent breast development Refer to paediatric endocrinologist if patient is 14.5 yearswithout pubertal onset and/or a specific abnormalityClinical notes: Precocious puberty (very rare) is indicated bypremature/early onset of pubic hair and testes 4 mL before 10years. Refer to paediatric endocrinologist.Klinefelter Syndrome (47,XXY)Presentation Small testes 4 mL characteristic from mid puberty Presentation varies with age, and is often subtle Behavioural and learning difficulties Gynecomastia (adolescence) Poor pubertal progression (adolescence)Investigations Total testosterone level (androgen deficiency) LH/FSH level (both elevated) KaryotypeTreatment and specialist referral Refer to paediatric endocrinologist Refer for educational and allied health assistance if neededRefer to Clinical Summary Guide 10: Klinefelter SyndromeDate reviewed: March 2018 Healthy Male (Andrology Australia) 2007 More prominent in obesity Often normal, resolves over monthsRare secondary causes: Hypothalamic pituitary lesions Adrenal/testis lesions (oestrogen excess)Treatment and specialist referral If persistent or acute onset, refer to paediatric endocrinologist
3Clinical Summary GuideMale AdulthoodGenital ExaminationExamination of male genitals and secondary sexual characteristics in adults.When should I perform an examination?Adulthood history and examination1. As part of a standard health check-up with new or existingpatientsPresentation with acute testicular pain2. 45-49 year old health assessment (MBS) (Note, Aboriginal andTorres Strait Islander men are eligible at younger ages) Testicular torsion3. Prior to initiation of drug treatment (e.g. testosterone, PDE5inhibitors) or investigation of conditions such as infertility orprostate disease4. On presentation of relevant risk factors and symptoms (below) This is a medical emergency Refer immediately for evaluation for surgery Later follow up review (e.g. epididymo–orchitis)History Fertility in current and past relationships Testicular trauma, cancer, STIRisk FactorAssociated disorderUndescended testes as an infantTesticular cancer Symptoms of androgen deficiencyPast history of delayed pubertyAndrogen deficiency Systemic treatment for malignancy, immunosuppression,organ transplant (for possible testicular damage)GynecomastiaAndrogen deficiency,Klinefelter syndrome,Testicular cancerInfertilityAndrogen deficiency,Testicular cancer Inguinal-scrotal surgery (undescended testes, childhood hernia) Gynecomastia Occupational or toxin exposureTesticular examinationTesticular volume Normal range of adult testicular volume: 15-35 mLErectile dysfunction (ED)Co-morbiditiesPast history of testicular cancerTesticular cancerGynecomastiaAndrogen deficiency,Klinefelter syndrome,Testicular cancer Abnormalities in the texture or hard lumps: suggests tumour orcystAndrogen deficiency,Male infertility VaricocelePituitary disordersOsteoporosis andatraumatic fracturesAndrogen deficiencyHaemochromatosisAndrogen deficiency,Male infertility Small testes 4 mL suggests Klinefelter syndromeScrotal and testicular contents Enlargement, hardening or cysts of the epididymides Nodules or absence of vas deferensPenile examination Hypospadias Peyronie’s disease MicropenisSymptomsAssociated disorder Urethral strictureTesticular pain or lumpsTumour or cyst Foreskin: balanitis, phimosisReduced libido, hot flushes, fatigue,gynecomastia, ED, mood changes,reduced beard or body hair, poor orreduced muscle developmentAndrogen deficiency Evidence of infection (STI) or inflammationSecondary sexual characteristics ofandrogen deficiency Reduced facial, body and pubic hair GynecomastiaHow do I best approach an examination withmy patient? Posters or pamphlets in your clinic can raise awareness aboutmen’s health examinations and convey that patients candiscuss reproductive health concerns with you Explain why you need to perform the examination and ask forpermission to proceed Allow the patient to ask questions and express any discomfortbefore/during the examination Ask specific questions during history-taking, to assist thosepatients reluctant to raise sensitive problems Reduced or poor muscle developmentProstate and other examinations In suspected prostate disease, digital rectal examination maybe considered, or an initial referral to urologist If prostate enlargement, tenderness or nodularity is found, referto urologist G eneral medical review of erectile dysfunction.Focus on cardiovascular risk (BP, pulses) & diabetes (includingneuropathy)
Androgen deficiency (AD)Penile abnormalityPresentationPresentation Symptoms of AD in men of any age Hypospadias Following testis surgery, torsion, trauma, cancer treatment Peyronie’s disease Incidental findings of small testes Micropenis In association with infertility Urethral stricturePrimary investigations Phimosis Total testosterone level (two morning fasting samples) and LH/FSH levelTreatment and specialist referralInvestigations if low total testosterone withnormal or low LH/ FSHTesticular mass Serum prolactin (prolactinoma) MRI pituitary (various lesions) Olfactory testing (Kallmann’s syndrome) Refer to urologist for investigation and treatment planPresentation Painless lump Self report, incidental Iron studies (haemochromatosis) Past history undescended testes (cancer risk) Also commonly seen with co-morbidities (obesity, depression,chronic illness): focus on underlying condition Confirm lump is in testis rather than epididymal cystPrimary investigationsOther investigations Testicular ultrasound SHBG/calculated free total testosterone (selected cases, e.g.obesity, liver disease) Treatment and specialist referral Bone density study (osteoporosis) Offer pre-treatment sperm cryostorage Semen analysis (if fertility is an issue)Refer to Clinical Summary Guide 6: Testicular Cancer Karyotype (if suspicion of 47,XXY)Treatment and specialist referral Refer to uro-oncologistGynecomastia Testosterone Replacement Therapy (TRT)*Contraindicated in prostate and breast cancer*Withhold treatment until investigation completePresentation in adulthood (common) In general, TRT is not justified in older men with borderlinelow testosterone levels and without underlying pituitary ortesticular disease Chronic liver disease Low-normal total testosterone is common in obesity orother illness and may not reflect AD. Address underlyingdisorders first. Consult a specialist to plan long term management: Excessive and/or persistent breast development Androgen deficiency Hyperprolactinaemia Adrenal or testicular tumours Drugs (e.g. spironolactone), marijuana, sex steroids Distinguish from ‘pseudogynecomastia’ of obesityPrimary investigations-- Refer to endocrinologist Total testosterone level, estradiol, FSH/LH-- Refer to fertility specialist as needed LFTs, iron studies (haemochromatosis)Refer to Clinical Summary Guide 4: Androgen DeficiencyKlinefelter syndrome (47,XXY)Presentation Small testes 4 mL characteristic from mid puberty. Infertility(azoospermia) or androgen deficiency Serum prolactin (pituitary tumour) Karyotype (if suspicion of 47,XXY) βhCG, αFP, ultrasound (testicular cancer)Treatment and specialist referral Refer to endocrinologist Other features vary, and are often subtle. These includetaller than average height, reduced facial and body hair,gynecomastia, behavioural and learning difficulties (variable),osteoporosis and feminine fat distribution Refer to plastic surgeon (after evaluation) if desiredPrimary Investigations Failure to conceive after 12 months of regular (at least twiceweekly) unprotected intercourse Total testosterone level (androgen deficiency) LH/FSH level (both elevated) Karytope confirmationOther investigations Bone density study (osteoporosis) Semen analysis (usually azoospermic) TFT (hypothyroidism) Fasting blood glucose (diabetes)Treatment and specialist referralMale infertilityPresentation Consider early evaluation if patient is concerned and/oradvancing female age an issue( )Other features: Testis atrophy (androgen deficiency) Past history undescended testis (cancer risk) Psychosexual issues (primary/secondary) Past history STI (obstructive azoospermia)Primary investigations Develop a plan in consultation with an endocrinologist Semen analysis: twice at 6-week intervals. Analysis atspecialised reproductive laboratory if abnormalities Refer to endocrinologist, as TRT is almost always needed FSH: increased level in spermatogenic failure R efer to fertility specialist as appropriate, for sperm recoveryfrom testis (occasionally) or donor sperm Testicular ultrasound (abnormal physical examination, pasthistory of undescended testes)Refer to Clinical Summary Guide 10: Klinefelter Syndrome Total testosterone and LH (small testes 12 mL or features ofandrogen level)
Treatment and specialist referral Healthy lifestyle, cease smoking Advice on natural fertility timing Identification of treatable factors (often unexplained and nospecific treatment) Refer to an endocrinologist as necessary Refer to a fertility specialist (ART widely applicable)Refer to Clinical Summary Guide 5: Male InfertilityDate reviewed: March 2018 Healthy Male (Andrology Australia) 2007
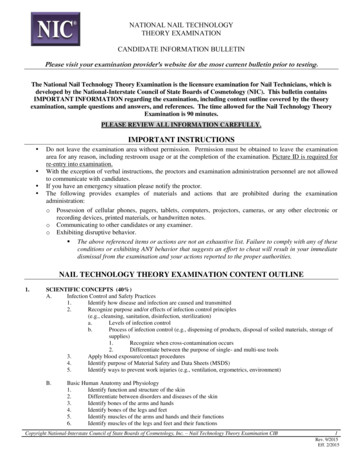
4Clinical Summary GuideAndrogen DeficiencyDiagnosis and managementAndrogen deficiency (AD)* Pituitary disease, thalassaemia, haemochromatosis. Androgen deficiency is common, affecting 1 in 200 men under60 years** AD is an uncommon cause of ED. However, all men presentingwith ED should be assessed for AD The clinical presentation may be subtle and its diagnosisoverlooked unless actively consideredExamination and assessment of clinical features of ADThe GP’s role GPs are typically the first point of contact for men withsymptoms of ADPre-pubertal onset – Infancy Micropenis Small testes The GP’s role in the management of AD includes clinicalassessment, laboratory investigations, treatment, referraland follow-upPeri-pubertal onset – Adolescence Note that it in 2015 the PBS criteria for testosteroneprescribing changed; the patient must be referred for aconsultation with an endocrinologist, urologist or member ofthe Australasian Chapter of Sexual Health Medicine to beeligible for PBS-subsidised testosterone prescriptions Failure of enlargement of penis and skin of scrotum becomingthickened/pigmented Late/incomplete sexual and somatic maturation Small testes Failure of growth of the larynx Poor facial, body and pubic hair GynecomastiaAndrogen deficiency and the ageing male Poor muscle development Ageing may be associated with a 1% decline per year in serumtotal testosterone starting in the late 30sPost-pubertal onset – Adult However, men who remain in good health as they age may notexperience a decline in testosterone Mood changes (low mood, irritability) The decline may be more marked in obese men Low energy (lethargy) Some estimates suggest that AD affects up to 1 in 10 men over60 years Hot flushes and sweats Acute and chronic illnesses result in decreased serumtestosterone and may present with AD-like symptoms Reduced beard or body hair growth The role of testosterone replacement therapy (TRT) in oldermen with modest declines in serum testosterone remainscontroversial The most consistent effects of TRT are on: Regression of some features of virilisation Poor concentration Decreased libido Low semen volume Gynecomastia Reduced muscle strength Fracture (osteoporosis)-- body composition and bone Erectile dysfunction (uncommon)-- selected aspects of mood and cognitionRefer to Clinical Summary Guide 6: Testicular Cancer-- libido Most studies of men with age-related AD have not shown anysignificant improvement in sexual function (erectile function)with TRTLaboratory assessment of AD Normal range serum total testosterone 8-27 nmol/L (but mayvary according to the assay used) The use of TRT for ageing men who do not meet the establishedcriteria (PBS guide) is not recommended Two morning fasting samples of serum total testosterone*,taken on different mornings Older men treated outside of guidelines should be informedthat long-term risks/benefits are not yet documentedGuidelines for the diagnosis of AD (PBS criteria):DiagnosisMedical history Undescended testes Surgery of the testes Pubertal development Previous fertility Genito-urinary infection Co-existent medical illness* Change in general well-being or sexual function** Degree of virilisation Prescription or recreational drug use1. AD in a patient with an established pituitary or testiculardisorder2. For men aged 40 :-- Testosterone 6 nmol/L**OR-- Testosterone between 6 and 15 nmol/L and LH greater than1.5 times the upper limit of the eugonadol reference range foryoung men*** If a second total testosterone sample is indicated, a LH levelshould also be ordered.** These criteria apply to men without underlying pituitary ortesticular pathology, to be eligible for PBS subsidy.
Other investigations SHBG/calculated free testosterone (selected cases - obesity,liver disease) Semen analysis (if fertility is an issue)ManagementAssessment of treatment indications Karyotype (if suspicion of Klinefelter syndrome, 47,XXY)PBS-approved indications for the prescription of testosteroneare:Investigations if low total testosterone with normal orlow LH/FSH: Micropenis, pubertal induction, or constitutional delay of growthor puberty, in males 18 years Serum prolactin (prolactinoma) Iron studies (haemochromatosis) MRI (various lesions) Olfactory testing (Kallmann’s syndrome)Causes of hypogonadism (AD)Testicular (primary) Chromosomal: Klinefelter syndrome (most common cause) Undescended testes AD in males with established pituitary or testicular disorders AD (confirmed by at least 2 morning fasting samples, both 6 nmol/L) in males aged 40 who do not have establishedpituitary or testicular disorders other than ageingTestosterone replacement therapy (TRT)Clinical note: Dosing ranges are provided below as dosageshould be titrated according to clinical response and serumtestosterone levelsT formulationUsual (starting)dosageDosage range Surgery: bilateral orchidectomyInjections (IM) TraumaSustanon ,Primoteston 250 mg every 2 weeks10 to 21-dayintervalsReandron 1000 mg every 12 weeksfollowing loading dose at6 weeks (i.e. 0, 6, 18, 30weeks)Longer term: 8 to16-week intervals Infection: mumps orchitis Radiotherapy/chemotherapy/drugs (spironolactone,ketoconazole) Systemic disease: haemochromatosis, thalassaemia, myotonicdystrophyTransdermal patchHypothalamo-pituitary (secondary)Androderm Idiopathic hypogonadotrophic hypogonadism: Kallmann’ssyndrome2.5 mg and 5.0 mg preps:5 mg applied nightlyTransdermal gel Pituitary microadenoma ( 1 cm) or macroadenoma ( 1 cm)- functional or non-functional: in men typicallymacroprolactinomaTestogel Other causes of hypothalamic pituitary damage: surgery,radiotherapy, trauma, infiltrative disease such ashaemochromatosisTransdermal creamKlinefelter syndromeOral undecanoate Is the most common genetic male reproductive disorder(1 in 550 men)AndriolTestocaps Is the most common cause of hypogonadism Reproductive features: small testes 4 mL, infertility, failureto progress through puberty, gynecomastia, eunuchoidalproportions, diminished or absent body hair, decreased skeletalmuscle mass2.5 to 5 mg dailyAndroForte 51%: 50 mg in 5 g sachetor pump pack dispenser;applied daily2.5 to 10 g gel (25mg to 100 mg T)daily5% (50 mg/mL): 2 mL (100mg) applied to the torsoonce dailyReview levels in 1month, up to 4 mLdaily40 mg capsule: 160 to 240mg in 2 to 3 doses daily80 to 240 mg daily* Sustanon is not available on the Australian PharmaceuticalBenefits Scheme (PBS)Follow-upMonitoring TRT is essential Other: learning difficulties & behavioural problems, particularlyin adolescence Testosterone levels: results should be interpreted in context ofthe treatment modality being usedRefer to Clinical Summary Guide 10: Klinefelter Syndrome Prostate: PSA, as per standard guidelinesClinical notes and contraindications Absolute contraindications to TRT are known or suspectedhormone-dependent malignancies (prostate or breast) orhaematocrit 55% Relative contraindications include haematocrit 52%,untreated sleep apnoea, severe obstructive symptoms of BPHand advanced congestive heart failure Fertility: Exogenous testosterone results in suppression ofspermatogenesis in eugonadal men. For men with secondarycauses of AD, and in whom fertility is desired, gonadotropintherapy should be instituted Low-normal serum testosterone common in obesity or otherillness may not reflect AD. Address underlying disorders first Withhold treatment until all investigations are complete Certain adverse effects must be prospectively sought,especially in older men, including polycythaemia and sleepapnoea, however the testosterone preparations discussed donot cause abnormal liver functionDate reviewed: March 2018 Healthy Male (Andrology Australia) 2007 Cardiovascular risk factors: blood pressure, diabetes, lipids, asper guidelines Osteopaenia/osteoporosis (fractures): bone density-DEXA Polycythaemia: haemoglobin and haematocrit, pre-treatment,at 3 and 6 months, and annually thereafter Sleep apnoea: clinical assessment for presence of sleep apnoea(polysomography)Specialist Referral It is a requirement for PBS-subsidised testosterone that thepatient is referred for a specialist consultation (endocrinologist,urologist or member of the Australasian Chapter of SexualHealth Medicine) and the name of the specialist must beincluded in the authority application Refer to an endocrinologist to plan long-term managementof AD Refer to a fertility specialist as needed Refer to a paediatric endocrinologist if 14.5 years old withdelayed puberty
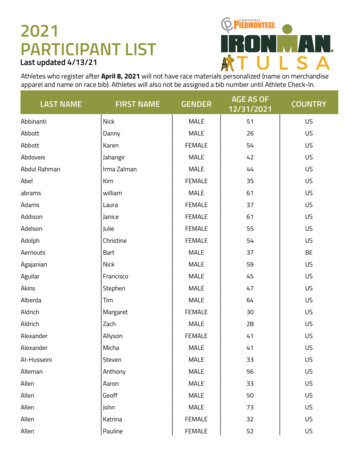
5Clinical Summary GuideMale InfertilityDiagnosis and managementPhysical ExaminationThe GP’s role Do not wait before beginning assessments GPs can begin with simple, inexpensive and minimally invasiveinvestigations Infertility needs to be assessed and managed as a couple, andmay require several different specialists See Healthy Male’s Male Fertility Assessment tool toaccompany this guide on our website.DiagnosisBrief assessment and pre-pregnancy adviceAgeWhat age is the couple?Fertility historyHow long have they been trying to conceive, andhave they ever conceived previously (together/separately)? Do they have any idea why theyhave not been able to conceive?ContraceptionWhen it was ceased, and the likely speed of itsreversibilityGeneralexaminationAcute/chronic illness, nutritional statusGenitalexaminationRefer to Clinical Summary Guide 1:Step-by-Step Male Genital ExaminationDegree ofvirilisationAndrogen Deficiency / Klinefelter SyndromeProstateexaminationIf history suggests prostatitis/STIInvestigationsSemen analysis is the primary investigation for maleinfertility.Key points Men should abstain from sexual activity for 2–5 days beforesample collectionFertile timesWhether the couple engage in regularintercourse during fertile times Two semen analyses should be performed at 6 week intervals.In men whose initial test is poor, the second test should ideallybe performed in a specialised laboratoryFemale riskfactorsAged 35 , irregular menstrual cycles, obesity,painful menses, or concomitant medicalconditions Semen analysis provides guidance to fertility; it is nota direct test of fertility. Fertility remains possible even inthose with severe deficitsFemale healthScreening for rubella and chicken pox immunity,Cervical Screening Test (25 years or older)Normal ranges for semen analysis (modified WHO, 2010)Lifestyle:femaleDiet, exercise, alcohol, smoking cessation andfolate supplementationLifestyle: maleDiet, exercise, alcohol, smoking cessationReproductive historyVolume 1.5 mLpH 7.2Spermconcentration 15 million spermatozoa/mLMotility 40% motile within 60 minutes of ejaculationAssess the male for:Why?Vitality58% or more live, i.e. excluding dyePrior paternityPrevious fertilityWhite blood cells 1 million/mLPsychosexual issues (erectile,ejaculatory)Interference with conceptionSperm antibodies50% motile sperm with bindingPubertal developmentPoor progression suggestsunderlying reproductive issueA history of undescended testesRisk factor
Examination of male genitals and secondary sexual characteristics. Step-by-Step: Male Genital Examination Clinical Summary Guide Testicular volume