Transcription
4/12/2018Diabetes management in liver and kidneydiseaseEpidemiology1
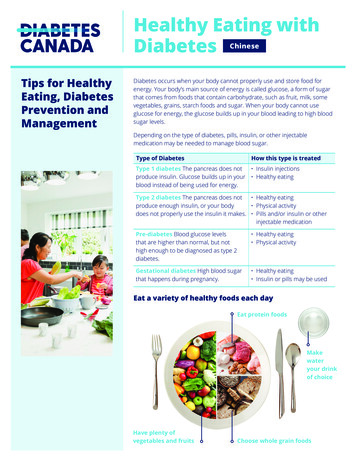
4/12/2018Clinical caseA 59 year old man with alcoholic cirrhosis; portal hypertension;mild encephalopathyFasting plasma glucose - 103, March 2016; 101, July 2017HbA1c 5.4 % Feb 2017Random plasma glucose - 212, March 2017; 220, September 2016QuestionsDoes he have diabetes?Should he take metformin?CategoryFPGNormalIFGIGTHigh riskDM 100100-125----- 1262hPG 140--140-199--- 200HbA1c 5.7----5.7 – 6.5 6.5 %A diagnosis of diabetes needs to be confirmed on a separate dayWHO cutoff for normal fasting plasma glucose is 110 mg/dl (6.1 mmol/l);& lower cutoff of 6% for HbA1cNo need to test if hyperglycemic crisis or symptoms of hyperglycemiaand glucose 200 mg/dL2
4/12/2018HbA1c levels may be lower in cirrhosis because ofincreased red cell turnover due to hypersplenismHbA1c levels may lower in ESRD due to anemia &Erythropoietin therapyKanda et al J Jpn Diabetes Soc 1993:36:84756 patients with cirrhosis were screened for diabetes with75g OGTT; WHO criteria22 (39%) – normal (FPG 110; 2hr glucose 140)13 (23 %) – impaired glucose tolerance (140-199) ; impairedfasting glucose (110-125)13 (23 %) – FPG 110; but 2hr glucose 2008 (14 %) - FPG 126 and 2hr glucose 200Nishida et al Am J Gastroenterol 2006: 101:703
4/12/2018Prevalence of diabetesCirrhosisDM35%IGT28 %Normal37 %glucosetoleranceHep CRNA veHep CHep BAbs veNo viralinfection18%15%12.5%11.4%9932 subjects; FPG 126 (Taiwan)Huang et al Am J Gastroenterol 2007; 102 :1237Nishida J Endo Soc 2017; 1: 886Nonalcoholic fatty liver disease (NAFLD) Hepatic steatosis Non alcoholic steatohepatitis (NASH) - hepaticsteatosis with hepatocyte injury (ballooning) &inflammation NASH cirrhosis - cirrhosis due to steatohepatitisChalasani et al Hepatology 2012 55:2005 (Guideline)4
4/12/2018Prevalence NAFLD; NASH (ultrasound & liver biopsy study inmiddle aged population without known liver disease)NAFLDWholecohort(n 328)DiabeticN 54Non H40(12.2%)NASH with 9stage 2-4 (2.7 %)fibrosisWilliams et al Gastroenterol 140: 124 (2011)Age standardized prevalence of obesity, DM, NAFLD ina Chinese populationMaleFemale2007(n 17192013(n 602P value2007(n 19172013(n 757P valueObesityBMI 2815.8219.41 0.0113.1818.77 0.01Diab6.379.23 0.014.418.48 0.01HTN38.138.6 0.0533.0433.01 0.05Dyslipid53.4665.5 0.0141.9654.7 0.01NAFLD(by US)23.4844.31 0.0117.5643.06 0.01Wu et al Scientific Reports 2017; 7: 415185
4/12/2018Summary - liver disease and diabetes(hepatogenous diabetes) Up to 35 % of patients with cirrhosis have diabetes Up to 18 % of patients with hepatitis C infection have diabetes Obesity increases the risk of diabetes and NAFLD. Extrapolation of NHANES data suggests that 400,000 people inUS have NASH cirrhosis and 4 million have NAFLD associatedadvanced fibrosis 11Kabbany et al Am J Gastroenterol 2017; 112: 5812007 - 2012 NHANES data; single sample marker CKD13.6 % of pop ( 30 million) CKD;3.9 % of pop CKD DM ( 8 on/healthstatistics/kidney-disease6
4/12/2018US 2015 data 468,000 have ESRD and 250,000 have diabetes 193,000 have functioning kidney transplant andabout 24 % of this population have diabetesPathophysiology7
4/12/2018Peripheral hyperinsulinemiain cirrhosisAUC 0-180 min76 15 vs 22 4 pmol/LLetiexhe et al J. Clin End Metab 1993; 77:1263Liver Tx normalizes insulin resistance76543210M valuemg/[kg.min]Perseghin et al. Hepatology 2000; 32:6948
4/12/2018Hepatitis C infection increases peripheral insulin resistance(minimal fibrosis - score F2; BMI 25.7 3.3; Caucasian men)Milner et al Gastroenterology 2010; 138:932Successful Rx of Hepatitis C can improve glucose control in T2DPre hepC RxHbA1cPostChange in % usinghep C HbA1c *insulinRxBeforeHbA1ctreatment% usingInsulinaftertreatmentChange in% oninsulin **7.277.08-0.1949.8%51.0% 1.2Patient7.20cured(n 2180)6.82-0.3741.3 %38%- 3.3Patientnotcured(n 255)Examined 1 year after Rx* Mean difference HbA1c drop cured vs not cured – 0.18; p 0.03** Mean difference in % on insulin cured vs not cure -4.5 %; p 0.04Hum et al. Diabetes Care 2017 40: 11739
4/12/2018Summary Insulin resistance occurs in cirrhosis and in hepatitis C patientswithout cirrhosis In cirrhotic patients, liver transplant will improve resistance &those with sufficient beta cell reserve will be cured of their diabetes Treating hepatitis C successfully may improve glucose controlTreating hyperglycemia in liver and kidney disease10
4/12/2018Grade A – 5 to 6Grade B – 7 to 9Grade C -10 to 15Pugh et al Brit J Surg /02/KDIGO 2012 CKD GL.pdfHepatorenal syndromeFunctional renal failure due to effective hypovolemia & intrarenalvasoconstriction263 cirrhotic patients with moderate or tense ascites followedfor 40.9 2.6 months5 year probability of hepatorenal syndrome was 11.4 %1 year survival of type 21 hepatorenal syndrome was 38.5 %1type2 – steady or slowly progressive renal failurePlanas et al Clin Gastroenterol Hepat 2006;4:138511
4/12/2018Hypoglycemia in liver diseaseCirrhosis – 156 patients : 6 patients had glucose levels 60; 2 patients 50Zimmerman et al Arch Int Med 1953; 91:577ADA/EASD algorithm 20156 classes of drugs:MetforminGLP1 receptor agonists/DPP 4 inhibitorsSulfonylureas ( other secretagogues)PioglitazoneSGLT2 inhibitorsInsulinMetforminMetformin anotherMetformin 2 othersMore complexinsulin regimensIn making therapeutic decision take into account efficacy; hypoglycemia risk;effect on weight; major side effects; cost12
4/12/2018Contraindications can damage your health—is metformin a case inpoint? Pooled data- 206 comparative trials – no cases of fatal or nonfatallactic acidosis in 47,846 patient years of metformin use, or in 38,221patient years of non-metformin use Old age is not an absolute contraindication May be safe at estimated GFR as low as 40ml/min Stable heart failure (NYHA 1 & II) not a contraindication Metformin is cleared by the kidney and half life is less than 5 hoursCochrane review: Diabetologia 2005; 48:24542016 FDA recommendationseGFR 60 ml/min/1.73 m2 – no metformin dose adjustment45 to 60 - more frequent monitoring30 to 45 – not recommended but can continue if taking. Consider50% dose reduction with renal monitoring every 3 months 30 – do not use13
4/12/2018Metformin use improves survival in cirrhosisRetrospective study 250 patients -172 continued metformin and 78 discontinuedafter diagnosis of cirrhosisMedian survival 11.8 vs 5.6 yrsSubgroup analysis – benefit withNASH induced cirrhosisNo cases of lactic acidosisZhang et al Hepatology 2014;60:2008Metformin use in T2D patients with HCV cirrhosis reduces risk of hepatocellularcarcinoma and liver-related death and transplant5yr incidenceHCC5.9 % vs 17.4%No Met - treated with diet, secretagogues; insulinNkontchou et al JCEM 2011; 96:260114
4/12/2018MetabolismDuration Durationof action of actionin CKDRecommendationGlyburide 1Liver; activemetabolites;excreted bile &urineUp to 24hrsIncreasedAvoid if GFR 60Avoid in liver failureGlipizide(Glucotrol)Liver 90%10 % excreted inurine6-12 hrsUnaffectedCan be used in CKDAvoid in liver failureGlimepiride 2(Amaryl)Liver but activemetabolitesUp to 24hrsIncreasedReduce dose (1mg) in renalfailureAvoid in liver failureRepaglinide 3,4(Prandin)Liver;metabolitesexcreted in bile3 hrsUnaffectedCan be used in CKDUse cautiously in liver diseaseNateglinide 5,6(Starlix)Liver;metabolitesexcreted in urine2 hrsUnaffectedCan be used in CKD & liverdisease1.Jonsson et al. Eur J Clin pharmacol 1998 53: 429. 2 Rosenkranz et al Diabetologia 1996 39: 16173. Marbury et al. Clin pharmacol ther 2000 67:7.4. Hatorp et al J Clin Pharmcol 2000;40:1425. Devineni et al J Clin Pharmacol 2003; 43:1636. Gangopadyay et a. Ind J End Metab 2017; 21:341Pioglitazone (Actos) Reduces microalbuminuria and hyperfiltration Beneficial effect on NAFLD; NASH Metabolized by liver; safe in CKD15
4/12/2018Pioglitazone or Vitamin E for NASHImprovement inNASHTotal NAFLDactivity scorePlacebo Vitamin E19 %43 %(p 0.001)Pioglitazone34 %(p 0.04)-0.5-1.9(p 0.001)-1.9(p 0.001)P values 0.025 considered statistically significantSanyal et al N Engl J Med 2010 362: 1675Adverse effects of pioglitazone Weight gainHeart failureFracture riskMacular edemaBladder cancer16
4/12/2018GLP-1 receptor enal sisReduce dose to 5 mcg BIDstage 3 CKD. Do not usefor GFR 30No dose changeProteolysisNo dose changeProteolysisNo dose changeRenal excretionNo dose change for eGFR 30Liraglutide reduce progression from microalbuminuriato macroalbuminuria161 vs 215Mann et al N Engl J Med 2017;377:839 (Leader trial)17
4/12/2018Effect of liraglutide on NASH after 48 week RxLiraglutide PlaceboP value1.8 mg(n 26)(n 26)9/232/22 (9%) 0.019(39 %)Resolutionof NASH(biopsy)Progression 2/23of fibrosis(9%)8/22(36 %)0.0430% had diabetes; liraglutide improved glucose levels & promoted weight lossJames Armstrong et al Lancet 2016;387:679FDA report of acute kidney injury with exenatideand liraglutide- thought to be due to vomiting, diarrhea & dehydration18
4/12/2018DPP 4 via)80% renal clearance100 mg usual dose. 50 mg forGFR 30-50; 25 mg for 30Saxagliptin(Onglyza)CYP3A4/5 metabolism;active metabolite; 24 %renal excretion5 mg daily usual dose. 2.5 mg ifGFR 50 or if taking strongCYP/3A4 inhibitorsLinagliptin(Tradjenta)80 % eliminated via bileand gut; 5 % renalclearanceNo dose change in renal diseaseor liver diseaseAlogliptin(Nesina) 70% renal clearance25 mg daily usual dose. 12.5 mgfor GFR 30-60; 6.25 mg for 30Sitagliptin did not alter CKD outcomes (TECOS)Saxagliptin improved albumin creatinine ratiobut not eGFR (SAVOR –TIMI)Cornel et al. Diab. Care Oct 2016Mosenzon et al Diab Care Oct 201619
4/12/2018SGLT2 vokana)Liver; 33 %Lower efficacy CKD 3renal clearance Do not use if GFR 45Dapagliflozin(Farxiga)Liver & kidneymetabolismEmpagliflozin(Jardiance)Liver andkidney10 mg daily usual dose.Use 5 mg if liver disease.Do not use GFR 60Do not use if GFR 45Empagliflozin reduces albuminuriaCherney et al Lancet Diab Endocrinol 2017 5:61020
4/12/2018Explanation of benefit of empagliflozin Improved glucoseImproved BPReduced weightImproved intrarenal hemodynamics – supported byobservation that benefit lost when drug stopped. Animal data that drug may reduce glomerulosclerosis andtubulointersitial fibrosis.DrugKidneydiseaseLiver diseaseMetforminSafe to use eGFRgreater than30 ml/min/1.73m2Beneficial in NASH relatedcirrhosis; hepatitis C cirrhosis;may reduce risk for hepatocellularCA. No evidence that there is anincreased risk of lactic acidosis.Stop in decompensated liverfailurePioglitazoneSafeBeneficial NAFLD; NASH; OK in class Acirrhosis; not recommended LFTs 3times ULNOralUse glipizide,secretagogues repaglinide,nateglinide.Lower doseglimepiride.NateglinideRepaglinide (cautiously)21
4/12/2018DrugKidney diseaseLiver diseaseGLP1 receptoragonistsLiraglutide; albiglutide;dulaglutide. Cautiously –acute kidney injury in settingof vomiting & dehydrationBeneficial NAFLD;NASHOK in class A cirrhosisDPP4 inhibitorsLinagliptin no doseadjustment; others renaldosing. Safe to useSafe to use. OK in classA; cautious class B;avoid class C cirrhosisSGLT2 inhibitorsAvoid in CKD 3 to 5OK in class A;cautious class B; avoidclass C cirrhosisInsulinSafeSafeAlpha glucosidase Avoid acarbose in CKD 4inhibitorsMiglitol cleared by kidney do not useOK in class A, B. Avoidclass CUrineprotein 0.16mg/mgcreatUrineHbalbumin 12-15.5 30mg/gcreatHomeglucoselevelsHbA1c Fructosamine59 yearwomanwith renaltransplant10.88787412.3200s8.3%26752 yearwomanwithalcoholiccirrhosisand DM-- 511.9Am g/dL22
4/12/2018Renal failureIncreased red cell turnover and erythropoietin treatment canfalsely lower HbA1c by as much as 1.5%Liver failureDecreased red cell survival time due to hypersplenism canfalsely lower HbA1c by 0.5 to 2.2 % (mean 1.7)In these cases fructosamine may be a better estimate ofglucose controlInaba et al J Am Soc Nephrol 2007; 18:896Little et al Clin chim Acta 2013; 418:73Kanda et al J Jpn Diabetes Soc 1993:36:84723
Abs ve Hep B No viral infection 18% 15% 11.4% 12.5% 9932 subjects; FPG 126 (Taiwan) Huang et al Am J Gastroenterol 2007; 102 :1237 Prevalence of diabetes Nonalcoholic fatty liver disease (NAFLD) Hepatic steatosis Non alcoholic steatohepatitis (NASH) - hepatic steatosis with hepatocyte injury (ballooning) & inflammation