Transcription
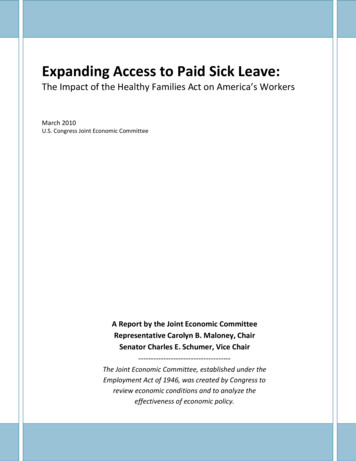
HUNTINGTONSTUDYGROUP.ORGHUNTINGTON DISEASEFA L L 2 0 2 0Also in this issue4 INEQUITY IN HDHEALTH ACCESS INLATIN AMERICA4 PREEMPTING ILLEGALBEHAVIORS ANDINCARCERATION4 AT-RISK “YOGI”SQUARES OFFAGAINSTCHRONIC PAINExpanding Access to CareTHEHUNT INGT ONS T UDYGROUP
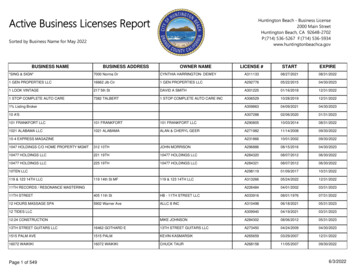
INSID E THI S I S S U E4 VOLUME 24Features10COVER STORYExpanding Carefor HD PatientsLessons from COVID-1916Preempting IllegalBehaviors andIncarcerationHelping to prevent people with HDfrom taking troubled pathways2226Forgotten HDPopulationsA Factor-HPerspectiveA Small but RelentlessFoundation Puts PuertoRico on the MapInequity in Health AccessAmongst HD Families in LatinAmericaDEPARTMENTS6834CLINICALCOORDINATOR’S CORNERInsights on clinical experiencesHD RESEARCHProfiles on current HD research4243HD CLINICAL TRIALSStatus of HD clinical trialsHD THERAPEUTICPIPELINEStatus of HD treatmentsSPOTLIGHTStories of resilienceHD INSIGHTS PODCASTThe HD Insights Podcast is designed as a long form,one-on-one interview format. Our goal is the same as withthe print publication: to promote, disseminate, and facilitateresearch and science education in HD by producinginformative content that will be valuable to the globalcommunity of HD researchers in academia and industry.See page 4.AVAI L A B L E O N L I N EApple iTunes: HTTP://BIT.LY/HSG-HDINSIGHTSGoogle Play: HTTP://BIT.LY/HDINSIGHTSPOD
HUNTINGTON DISEASEFALL 2 0 2 0HUNTINGTONSTUDYGROUP.ORGImproving disparities of careo say that 2020 has been a difficult year would be a wild understatement.I cannot begin to summarize the events over the last nine months, butcan perhaps suggest that there is a great need for hope. We are living ina time where there is a strong momentum to improve disparities in thecare received by people throughout our country and world. How exciting!I believe Huntington disease is an important part of this story.In this edition, we address disparities evident in HD. As you probably know, ourpodcast has received quite a following now, and one of the recent highlights was theinterview with Dr. Munoz-Sanjuan (affectionately known to many as ‘Nacho’). ForHD Insights, Nacho has written a provocative article, which brings together a theme oflooking back at the early work in Venezuela, and forward to the ongoing needs in SouthAmerica. Zoé Cruz-Gil also shares her story of determination and grit in identifying andhelping HD patients across the island of Puerto Rico. Please consider supporting FactorH and Fundación Huntington Puerto Rico.We also address the issues of healthcare disparities in the U.S., highlighting twoarticles regarding telehealth for HD, and emphasizing the challenges to psychiatriccare in a third piece. I’m sure all of us have had to adapt in new ways as we deliver carein novel platforms, but I hope these stories resonate with you. Finally, we are fortunateto discuss an inspirational story of hope and healing in HD.I must apologize that while some of this edition may come across as slightly Tennesseecentric, it is largely because my life has been in Tennessee. I am certain you all have storiesof resilience and hope that you would like to share. Please send them to our deputyeditor, Margy Rockwood, at margaret.rockwood@vumc.org.Thanks to our supporters of this periodical, and to the HSG for giving us this platformto tell these stories.I hope to see you soon (and in person),PUBLICATION STAFFMargaret RockwoodDeputy EditorChristina Ullman, MSJArt Director,Ullman DesignEDITORIAL BOARDDaniel Claassen, MDEditorVanderbilt UniversityDonald Kennedy, PhDStanford UniversityNobuyuki Nukina, MD, PhDRiken BrainScience InstituteRodrigo OsorioAgrupación Chilenade HuntingtonRalf Reilmann, MD, PhDGeorge Huntington InstituteHUNTINGTONSTUDY GROUPLauren FalangaManager, ClinicalCollaborationsKevin GregoryDirector, Education,Communicationsand OutreachShari Kinel, JDExecutive DirectorDANIEL CLAASSEN, MDAssociate Professorof NeurologyVanderbilt UniversityJanine MercandettiManager, Projectsand ContractsKristin StrazdinsManager, Financeand Special ProjectsAnne Van Dusen, CHCDirector, Operations
IN BRIEF4 NEWS HIGHLIGHTSFirst Two Patients Treated in uniQurePhase I/II Clinical Trial of AMT-130Milestone Marks the First-in-HumanAAV Gene Therapy Trial for Huntington’s DiseaseUJune 19, 2020 Press ReleaseniQure N.V., a leading gene therapy companyadvancing transformative therapies for patients withsevere medical needs, has announced that the firsttwo patients in the Phase I/II clinical trial of AMT-130for the treatment of Huntington’s disease have beentreated. The Phase I/II study is a double-blind, randomized clinical trialbeing conducted in the United States, with now one patient treated withAMT-130, and one patient who received the imitation surgery. 04 / H D I N S I G H T S“For years, uniQure has had anunwavering commitment to advancethis first-in-human AAV gene therapyfor Huntington’s disease into clinicaltesting, and this moment marks animportant milestone for our companynow that we have two AAV gene therapycandidates in clinical development,” saidMatt Kapusta, chief executive officerof uniQure. “With the first two patientstreated in this trial, we have taken asignificant step forward in advancingAMT-130 closer to our goal of developinga therapy that inhibits the productionof the mutant huntingtin protein. Weare delighted to be working with leadingexperts in the field to evaluate thispromising candidate.”The Phase I/II clinical trial of AMT-130for the treatment of Huntington’s diseasewill explore the safety, tolerability, andefficacy signals in 26 patients withearly manifest Huntington’s diseaserandomized to treatment with AMT-130or an imitation (sham) surgery. Thefive-year, multi-center trial consistsof a blinded18- month core studyperiod followed by unblinded long-termfollow-up. Patients will receive a singleadministration of AMT-130 through MRIguided, convection-enhanced stereotacticneurosurgical delivery directly intothe striatum (caudate and putamen).Additional details are available onwww.clinicaltrails.gov (NCT04120493).The first two patients will be observedfor an initial period of 90 days, followed bya meeting of the Data Safety MonitoringBoard (DSMB). The DSMB will review thedata on the first two patients and make adetermination about continued dosing ofthe next patients.
stuniQure HD Insight ad 031220 outline.pdf 1 3/12/2020 5:21:07 PMAMT-130 is uniQure’s first clinicalprogram focusing on the central nervoussystem (CNS) incorporating its proprietarymiQURE platform.“There is an urgent need for diseasemodifying options to treat Huntington’sdisease, and we’re excited to have aninvestigational gene therapy now availablefor HD patients,” stated George Yohrling,chief scientific officer and chief missionofficer at Huntington›s Disease Societyof America. “Based on the promisingpreclinical data presented on AMT-130over the years, we are optimistic aboutits potential to alter the course of thisdevastating disease.”CMYCMMYCYA B O UT U N I QUR ECMYKuniQure is delivering on the promiseof gene therapy — single treatmentswith potentially curative results. We areleveraging our modular and validatedtechnology platform to rapidly advancea pipeline of proprietary gene therapiesto treat patients with hemophilia B,hemophilia A, Huntington’s disease, Fabrydisease, spinocerebellar ataxia Type 3 andother diseases.Learn more at: www.uniQure.comFA L L 2 0 2 0 / . 05
IN BRIEF4 C L I N I C A L C O O R D I N AT O R ’ S C O R N E RChallenges HD Patients and CaregiversFace During the COVID-19 PandemicBY DANIELLE BUCHANANAND KATHERINE MCVAYThis year marks an unprecedented era in healthcare accessibility and availability that iscurrently affecting the lives of HD patients and families. As a result of the coronavirusdisease 19 epidemic and the social isolation that has followed, HD patients are facedwith new barriers to care. While there had been a trend towards telemedicine and othertechnologically savvy forms of healthcare delivery prior to the pandemic, COVID-19 hasmade remote medicine a necessary recourse for care, as opposed to a luxury.The clinical research team at Vanderbilt’s HDSA Center of Excellence recently conducted a studyduring the “stay-at-home” orders between April and May 2020. The team contacted HD patientsand either spoke with the patient or their caregiver over the phone to answer open-ended questionsabout the ways in which the pandemic has affected them. The questions addressed issues suchas economic hardship, their current access to medication, and their current utilization of remotehealthcare such as telemedicine appointments and online support groups.The results from this study reveal some of the specific weaknesses within the current healthcareinfrastructure. These can be addressed to create improvements in HD clinical care from the start ofdiagnosis to the continued management of symptoms and monitoring of both mental and physicalhealth as the disease progresses.Self-isolation during the pandemic can create new anxieties for the families of HD patients. In ourstudy, 20 percent of the caregivers were parents of the HD patient while around 10 percent wereoffspring. For HD caregivers, the issues that they face during this time are multifaceted. Family unitsin self-isolation nationally are dealing with the stress of a global pandemic, the economic and mentalburden of Unemployment, and the loss of a daily routine. All of these affect mental health and wellbeing. Family members with HD are dealing with all these issues while also managing care, with lessaccess to important healthcare services.In the wake of these new issues, it is important for individuals in the caregiving role to haveaccess to helpful resources. It is essential for providers during a pandemic to be consistent andthorough in providing information for families dealing with HD during this time. Clinical teamsshould be addressing the well-being of the entire family unit. As an example, one family followed atthe Vanderbilt’s HDSA Center of Excellence has their own small business screen printing t-shirts,and relied on orders for large group events and family gatherings. With the pandemic, this patientand their entire family lost the majority of their business and continue to suffer from the loss ofIt is essential for providersduring a pandemic tobe consistent and thorough inproviding information for familiesdealing with HD during this time.”DANIELLE BUCHANANDanielle Buchanan is a clinical translational research coordinator at the Vanderbilt Huntington Disease Center of Excellence,which cares for over 400 HD patients in the southern region of the United States. 06 / H D I N S I G H T Sincome. This lost income results inincreased stress for the patient andcaregiver, and may even impair theirability to receive valuable resourcesneeded for their care.Around 50 percent of therespondents in this study indicatedan interest in a virtual support group,which would be a very productive wayto engage with these problems andbuild a strong sense of togetherness.Some families could potentially benefitfrom the Family and Medical Leave Act,which provides unpaid leave to providecare for their ailing family member. HDfamilies could also benefit from supportgroups in which they can connectwith other families regarding problemsthey face caring for a loved one withHD, dealing with a recent diagnosis orthe genetic status of an at-risk familymember during the global pandemic.While telehealth offers a quicksolution to the lack of face-to-faceclinical care during the pandemic,around 25 percent of respondentsindicated that they were unable toparticipate in regular telemedicineappointments. The survey did not revealthe reasons for this unwillingness,but anecdotally, we gleaned that theyfeel unable to access telehealth callsfor either technological of financialreasons, or are generally disinterestedin virtual engagement. This revealsthat a healthcare system based entirelyon telehealth could neglect onefourth of our HD patient population.Telemedicine requires technologysuch as smart phones and computersthat not every family can access. Forthose that are not as tech savvy, it canbe difficult to navigate the telehealthplatforms that are currently used. Last,many patients and families mightnot consider communication viathe internet a viable alternative toin-person communication and care.
All of these reasons and more must beaddressed with the patient and theirfamily in order to provide properclinical care to the HD population.It is important for clinical teamsto work with families that are notinterested in traditional telehealthplatforms to ensure no serious declinein care during the pandemic.Financial barriers affect more thanjust accessibility to telemedicine callsand appointments. Of the total surveyrespondents, 25 percent were eitheruninsured or on Medicaid. Beyondthe lower likelihood of these patientsutilizing telemedicine portals, thispopulation is at an even greater riskof not obtaining treatment for anyworsening HD symptoms during thispandemic. This risk is the result ofdelay in care, inability to pay for visitsor medications, and a general lackof resources, all of which are furtherexacerbated by the pandemic.The delay of care for the uninsuredand Medicaid-covered HD populationis also worsened by the Medicaidwaiting period between diagnosis and25%The number of patientsin the survey experiencedfinancial barriers to care by eitherbeing uninsured or on Medicaid.coverage — currently, 24 months.The Huntington’s Disease Parity Actof 2019 is a bill that would waivethis waiting period for HD patients.If passed, HD patients could receivecoverage earlier in their diagnosis,which is critical in managing earlysymptoms and the progression ofHuntington’s disease.During this time, HD families withadequate resources still struggle tomanage care. While virtual solutionslike telemedicine can help alleviatemany barriers, HD families with greaterhardship and financial strain from thepandemic are not as likely to benefitfrom these short-term solutions. It isvital that clinical teams address thesepopulations and determine the bestways to overcome the barriers thepandemic has created. We need toacknowledge the weaknesses in ourhealthcare system and advocate forthe HDPA bill and others that wouldhelp level the playing field for HDfamilies. Our study underlines the needfor clinical teams to be particularlyflexible, resourceful and, as always,empathetic in addressing the wellbeing of the entire HD family unitsas they navigate the difficulties ofHD in a global pandemic.FA L L 2 0 2 0 / . 07
HD RESEARCHprofilesBY LISE MUNSIE, PH.D.Dr. Munsie is Senior Development Manager and Project Leader,Pluripotent Stem Cell Therapies at CCRM, a Canadian, not-forprofit group that is focused on developing and commercializingregenerative medicine, cell and gene therapy technologies.2Understanding HDin Neurodevelopment1The natural history of Huntington’s disease has largelyfocused on Caucasian people of European descent. Bestpractice treatments are largely reserved for populations inareas of economic stability, due to the costs associatedwith genetic testing and other treatment options. Thisalso means that genetic treatments focused on allelespecific silencing are tailored to these populations. Theseissues are being acknowledged by scientists.Correspondence in The Lancet brought up theproblem of identifying HD in low/middle incomecountries like Bangladesh, where doctors willoften misdiagnose HD due to lack of funding andavailability of genetic testing.1 This hinders research on actual prevalence, and meanspatients in these areas are not getting the required resources.In Caucasian European populations, the mutant huntingtin gene (HTT) is associated withhaplogroup A, which is the target of many allele-specific silencing efforts, whereas populationdata in other areas of the world suggests association with other haplotypes.A family from Oman with several generations of HD were the subject of a recent study by theHayden group. This family tree had eight generations and represented the largest known HDcluster in the Middle East.2 The study found the oldest African family ancestor had a C6xC9haplotype associated with this cluster, supporting the hypothesis that mutant HTT has arisenspontaneously and independently in different geographical locations. These studies shed lighton the initial spread of HD through different populations as well as indicate how therapies needto be targeted to serve different genetic backgrounds.In order to expedite therapies, the FDA uses the Clinical Data Interchange Consortium(CDISC) standards. Clinical data standardization will lead to a faster path to regulatory approvalfor urgently needed new therapies for patients. Therapeutic Area User Guides (TAUG) describeCDISC standards and are used to document efficacy in clinical trials. A TAUG for HD hasrecently been established in conjunction with HD Regulatory Science Consortium.3 This will beused in validating treatments for HD and acting as an example for the development of TAUG forother rare and orphan diseases.Identifying HDin Low IncomeCountries1Islam, Z et.al. (2020) Huntington’s Disease in Bangladesh. Lancet Neurology 19(8):644-645Huntington’s disease is well-known to be neurodegenerative disorder, but it is also hypothesized tobe a neurodevelopmental disorder. Understanding ifand how mutant huntingtin (mtHTT) is involved inneurodevelopment will have consequences for treatment.Imaging studies can look at brain morphology relatedto the development process. An imaging study involvingwhole-brain anatomical MRI acquisition of adult earlystage HD patients and looking at sulcal morphometrywas recently performed.1 Sulcal length is related todevelopment. Most of the degeneration found in thisstudy could be related to atrophy, however the length ofthe Sylvian fissure was abnormal and strikingly lackingin symmetry between brain hemispheres. These changesare indicative of abnormal neocortical development asthe Sylvian fissure appears in utero.Another imaging study using resting state functionalMRI (fMRI) looking at neurodevelopmental problemsassociated with mtHTT was performed on childrenbetween the age of 6-18.2 Asymptomaic youth at risk forcarrying mHTT were consented for the study and theirgene status was kept confidential. The findings fromthis study support the neurodevelopmental theory ofneurodegeneration. The study showed hyperconnectivityof the striatum to cerebellum following the loss ofconnectivity over time, specific to the children carryingmHTT. These connectivity issues are noted years beforepredicted motor onset.One additional study on the field of neurodevelopmentin HD examined tissue from 13 week gestational fetusesthat were carrying mHTT. Imaging studies showedmislocalization of mHTT in the ventricular zone whichwould disrupt the polarity of the neuroepithelium.3This was recapitulated in HD mouse models. Usingthe mouse models, the study goes on to probe themechanism of this neurodevelopmental hindrance andfinds issues with endosome secretion, abnormal cellcycle and altered neurogenesis may contribute to theseearly defects.The understanding of HTT role in neurodevelopmentmay explain outcomes from HTT lowering and othertherapeutic strategies.1Mangin, Jean-Francois et.al (2020) Neocortical morphometry in Huntington’sdisease: Indication of the coexistence of abnormal neurodevelopmental andneurodegenerative processes. NeorImage:Clinical 26:1022112Squitieri, F et.al. (2020) Tracing the mutated HTT and haplotype of the African ancestor who spread Huntington Disease into theMiddle East. Genet Med. 10.1038/s41436-020-0895-12Tereshchenki, A.V et.al (2020) Abnormal development of cerebellar-striatalcircuitry in Huntington disease. Neurology 94:e1908-e19153Mullin, A et.al (2020) Standardized data structures in rare disease: CDISC user guides for Duschenne Muscular Dystrophy andHuntington’s Disease. Clinical and Translational Science. Doi.org/10.1111/cts.128453Barnat, M et.al (2020) Huntington’s disease alters human neurodevelopment.Science 6506:787-793. 08 / H D I N S I G H T S
3The Roleof ImmuneResponsein HDThe mechanism of cell selectivity in Huntington’s disease (HD)is often traced back to transcription changes leading to alterationsin the immune response in the vulnerable cell populations.Discovering the mechanisms of these changes and the genes andproteins responsible could lead to therapeutic pathways.A report in Neuron uses single nuclear RNA sequencing(snRNA-seq) and translating ribosome affinity purification (TRAP)to examine cell-type specific alterations to gene expression inHD.1 The group uses the TRAP assay to assess different striatalsubpopulations in a series of HD mouse models. The groupadditionally used snRNA-seq on post-mortem brain tissue fromHD patients to confirm their findings. Results showed a releaseof mitochondrial RNA specific to the spiny projection neurons,leading to an immune response, and a combination of non-celltype and cell-type specific responses contributing to the selectivevulnerability of these cell types. Regulating transcription andsuppressing the immune response could therefore be a targetfor HD therapy.Regulating transcription and suppressing the immuneresponse could be a target for HD therapy.Immune activation is hallmarked bythe release of cytokines. Interleukin-6(IL-6) upregulation has been notedin HD but whether this upregulationis beneficial or pathological remainsunknown. A recent study crossesthe R6/2 HD model with a mousemodel deficient in IL-6 and examinesthe phenotypic outcomes on mousebehaviour: rotarod, open field assay,rearing and climbing and gripstrength. Knocking out IL-6 led toan increase in severity in almostall behaviours, indicating that theincrease in IL-6 is likely beneficial.This increase in phenotypic severityseems to be a consequence ofdysregulation of synaptic transmissionand neurotrophin signaling causedby the IL-6 knockout, indicatingthat elevating IL-6 levels at certaintimepoints in the course of HD mayhave beneficial effects.2Further evidence to supportinflammation as a cellular responsein HD comes from another study thatidentifies cGMP-AMP synthase (cGAS),with known activity in regulatingautophagy and inflammation, asupregulated in HD striatum.3 As withthe other groups, evidence of thisupregulation is found both in mousemodels, where there is a high occupanyof cGAS at the ribosome, and inhuman tissue, where an upregulationof cGAS regulated genes was noted. Itis hypothesized that inhibiting cGASduring the course of HD may helpalleviate symptoms associated with theinflammation response.Lee, H et al (2020) Cell Type-SpecificTranscriptomics Reveals that Mutant Huntingtin Leadsto Mitochondrial RNA Release and Neuronal innateImmune Activation. Neuron 107: 1-181Wertz, M.H. et al. (2020 Interleukin-6 deficiencyexacerbates Huntington’s disease model phenotypes.Molecular Neurodegeneration. 15:292Sharma, M et.al (2020) Cyclin GMP-AMP synthasepromotes the inflammatory and autophagy responsesin Huntington disease. PNAS 117(27) 15989-159993IMMUNE RESPONSEImmune activation is hallmarked by therelease of cytokines. Interleukin-6 (IL-6)upregulation has been noted in HD butwhether this upregulation is beneficial orpathological remains unknown.FA L L 2 0 2 0 / . 09
HD IN S I G HTS4 C O V E R S T O RYThe pandemic has forcedhealthcare workers to reassessthe traditional office visitmodel, and regulators to loosenrestrictions on telehealth. 10 / H D I N S I G H T S
B Y JE N N I F E R K L APPER,K AV I T H A M U R A L I D H A R A N , A N D I A N SI GAL ,ExpandingCarefor HD PatientsLessons from COVID-19As social distancing has become the norm duringthe coronavirus pandemic, Huntington’s disease(HD) patients, already facing the burdens oftheir disease, have been forced to endure theadditional hardships brought on by isolation.Medical professionals have also faced novelchallenges as they have adapted their practice patterns in response toclinic closures. The pandemic has forced healthcare workers to reassessthe traditional office visit model, and regulators to loosen restrictionson telehealth.As two fourth-year medical students and nurse coordinator ofa Huntington’s Disease Center of Excellence, we had the valuableopportunity to experiment with this and other new models of deliveringcare to the HD community. Our experience during the pandemic hasshown us that online virtual appointments allow us to deliver careand maintain therapeutic relationships with patients. It is clear to usthat telehealth will play a role in caring for HD patients beyond thepandemic, especially as we strive to improve access to multidisciplinarycare to the HD community. We are happy to be sharing some of thequestions we had going into this initiative and the answers we foundafter four months of working with patients with HD.FA L L 2 0 2 0 / . 11
HD IN S I G HTS4 C O V E R S T O RYComprehensive patient careHow does the healthcare system promote orprevent physicians from reaching patients,particularly in the context of HD?including physical therapy and on-site psychiatry notoffered at general neurology offices are available atHD Centersof ExcellenceHD Centers of Excellence provide comprehensive andmultidisciplinary care for Huntington’s patients, butare not accessible to all. HD is a rare disease, and asa consequence, HD centers are few and far between. Outsideof Philadelphia, the only HD Center of Excellence in thestate of Pennsylvania is at the University of Pittsburgh. Theseinstitutions may be accessible to some patients living in majormetropolitan areas, but for many living outside of cities, theseservices are several hours away and functionally out of reach.Even for patients who live within driving distance of anHD center, in-person visits can offer many barriers to care.HD patients become progressively reliant on their families fortransportation and day-to-day needs. Many caregivers of HDpatients are the sole working members of their families, and it canbe challenging for them to take a day off from work or sacrifice aday’s wages to bring a loved one to a clinic. Going to an in-personclinic visit requires both money and time to travel to the citycenter, to find parking, and to wait in the waiting area beforeseeing the physician. As such, it becomes an impossible task formany caregivers to bring HD patients to in-person appointments.Beyond that, as HD is a psychiatric as well as a neurologicillness, both irritability and apathy are prominent features of HD.The difficulties of getting to these appointments can be doublyfrustrating for HD patients. These barriers can disincentivizepatients from receiving necessary care.As a consequence, many of these patients rely on their localneurologists to manage their HD. Yet given that HD is sucha rare disease, very few general neurologists have significantexposure to this patient population. Moreover, general neurologyoffices cannot offer the breadth of services—such as physicaltherapy and on-site psychiatry—that are available at HD Centersof Excellence and are necessary for comprehensive patient care.Telehealth has offered a solution to many of these problems.Penn’s HD Center of Excellence (based out of Philadelphia)run by Pedro Gonzalez, MD, PhD, Tanya Bardakjian, MS,LCGC, and Jennifer Klapper, MSN, RN, CNS-BC, has beenable to care for patients from as far away as Pittsburgh, openingup opportunities for care to new patients. Telehealth has alsoaddressed many of the financial and emotional barriers tocare. In-person visits can now be held at the patient’s terms inthe location of their choosing, and the time and effort spenttravelling has been eliminated.Moreover, we have found that patients have enjoyed seeingtheir doctors from the comfort of their own homes. Manypatients are happier during telehealth appointments, making iteasier for us to get a sense of what patients truly look like in theirown environments. This, in turn, leads to a much more accurateestimation of functional capacity than could ever be obtained atthe office.How has the impact of COVID-19on families of patients with HDinformed views on telemedicine?Telehealth has made the substantial barriers patientsface to attend even simple outpatient visits evidentto us. One patient we met suffered with severedepression as a consequence of their HD. As a result, even asimple task like rising out of bed was a challenge, making it. 12 / H D I N S I G H T S
Telehealth has addressed many of the financial and emotional barriers tocare. In-person visits can now be held at the patient’s terms in the location oftheir choosing, and the time and effort spent travelling has been eliminated.extremely difficult for the patient to attend in-person visits.Once we switched to the telemedicine platform, our patientwas able to attend appointments far more consistently.HD-related depression is common in the HD community,and as a result many patients struggle to find the motivationto travel for their appointments. By reducing the “activationenergy” needed to attend appointments, telemedicine appointments help even those patients with crippling apathy to get thecare they deserve.Telemedicine has also shed light on the challenges of familymembers in bringing their loved-ones to appointments. One patientwe cared for struggled to make it to clinic for a new patient visitbecause their caregiver worked nights. It was not practical forthem to drive to the city and spend hours in clinic to be seenby a neurologist, psychiatrist, social worker, and therapist, onlyto drive straight back to work for the next night shift withoutany time to sleep. Using telehealth, we were able to shave threehours off this process, allowing them to become an establishedpatient in our clinic and connected with all of the resources wecould offer.Although the transition to telehealth at the onset
AAV Gene Therapy Trial for Huntington's Disease.04 / HD INSIGHTS U niQure N.V., a leading gene therapy company advancing transformative therapies for patients with severe medical needs, has announced that the first two patients in the Phase I/II clinical trial of AMT-130 for the treatment of Huntington's disease have been treated.