Transcription
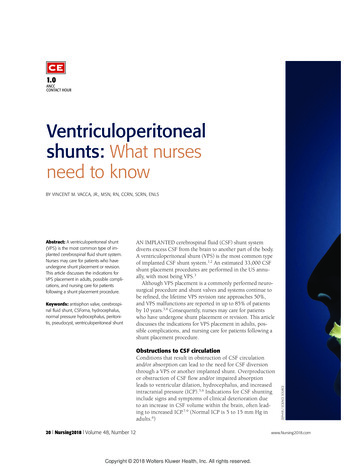
1.0ANCCCONTACT HOURVentriculoperitonealshunts: What nursesneed to knowBY VINCENT M. VACCA, JR., MSN, RN, CCRN, SCRN, ENLSKeywords: antisiphon valve, cerebrospinal fluid shunt, CSFoma, hydrocephalus,normal pressure hydrocephalus, peritonitis, pseudocyst, ventriculoperitoneal shuntAN IMPLANTED cerebrospinal fluid (CSF) shunt systemdiverts excess CSF from the brain to another part of the body.A ventriculoperitoneal shunt (VPS) is the most common typeof implanted CSF shunt system.1,2 An estimated 33,000 CSFshunt placement procedures are performed in the US annually, with most being VPS.3Although VPS placement is a commonly performed neurosurgical procedure and shunt valves and systems continue tobe refined, the lifetime VPS revision rate approaches 50%,and VPS malfunctions are reported in up to 85% of patientsby 10 years.3,4 Consequently, nurses may care for patientswho have undergone shunt placement or revision. This articlediscusses the indications for VPS placement in adults, possible complications, and nursing care for patients following ashunt placement procedure.Obstructions to CSF circulationConditions that result in obstruction of CSF circulationand/or absorption can lead to the need for CSF diversionthrough a VPS or another implanted shunt. Overproductionor obstruction of CSF flow and/or impaired absorptionleads to ventricular dilation, hydrocephalus, and increasedintracranial pressure (ICP).5,6 Indications for CSF shuntinginclude signs and symptoms of clinical deterioration dueto an increase in CSF volume within the brain, often leading to increased ICP.7-9 (Normal ICP is 5 to 15 mm Hg inadults.6)20 l Nursing2018 l Volume 48, Number 12Copyright 2018 Wolters Kluwer Health, Inc. All rights reserved.ZEPHYR / SCIENCE SOURCEAbstract: A ventriculoperitoneal shunt(VPS) is the most common type of implanted cerebrospinal fluid shunt system.Nurses may care for patients who haveundergone shunt placement or revision.This article discusses the indications forVPS placement in adults, possible complications, and nursing care for patientsfollowing a shunt placement procedure.www.Nursing2018.com
www.Nursing2018.comDecember l Nursing2018 l 21Copyright 2018 Wolters Kluwer Health, Inc. All rights reserved.
Hydrocephalus, described as bothan active and progressive dilation ofthe ventricular system, occurs whenCSF production exceeds the absorption rate (see Go with the flow: Normalanatomy and physiology).5,6 Considered a clinical syndrome, it can resultfrom CSF overproduction, obstruction of CSF circulation, or decreasedCSF reabsorption.5Hydrocephalus can be subdividedinto noncommunicating or communicating hydrocephalus.5,10,11 In noncommunicating or obstructive hydrocephalus, the flow of CSFbetween the ventricles is obstructedor blocked. In adults, brain tumors,especially intraventricular tumors,are a common cause of noncommunicating hydrocephalus.6 Communicating hydrocephalusoccurs when there is a defect in thesites of absorption of CSF.6 Thisform is called communicating becauseCSF can still flow between the ventricles. Most cases of communicatinghydrocephalus are due to subarachnoid hemorrhage (SAH) or infectionsuch as meningitis or gradual dysfunction due to aging.6 Debris fromblood breakdown in SAH or exudateassociated with meningitis can obstruct the arachnoid villi and prevent them from absorbing CSF normally.5 Signs and symptoms of hydrocephalus are variable, dependingon the patient’s age and type of hydrocephalus (see Signs and symptomsof hydrocephalus in older children andadults).A subset of communicating hydrocephalus seen in older adults isnormal pressure hydrocephalus(NPH), another indication for VPS.This is defined by cerebral ventricular dilation seen on brain imagingand normal CSF pressure on lumbarpuncture. It is associated with theclinical triad of gait disturbance, cognitive impairment, and urinary incontinence.12 NPH may be idiopathicor develop as a complication of SAH,head trauma, infection, or a tumor.6,11 An estimated 700,000 Americans have NPH, but the actual number may be much higher because thedisorder is often underdiagnosed.6A useful diversionVentricular shunting is used to manage hydrocephalus by routing excessCSF to another part of the body.The peritoneal cavity is the mostcommon extracranial site for distalshunt catheter termination because itis easy to access and provides theGo with the flow: Normal anatomy and physiology5The major source ofCSF is secretions fromLateral (first and second)ABthe choroid plexus, aventricles in leftcauliflower-like strucand right hemispheresture located in portionsThird ventricleof the lateral, third, andfourth ventricles. TheAqueductchoroid plexus is a colFourth ventriclelection of blood vesselsCentral canalCcovered with a thincoating of ependymalLateral ventriclecells. CSF is constantlyInterventricular foramensecreted from these(of Monro)surfaces. It is estimatedThird ventriclethat the amount of CSFproduced daily by theA: Lateral aspect of the left cerebral hemisphere showing the contour of the lateral ventricles and their relation tochoroid plexus isthe cerebral lobes.25 mL/h, or 500 to 600 B: Lateral outline of the four ventricles.C: Frontal (coronal) section of the lateral and third ventricles at the level of the dotted line (B), showing their commL per day.municating interventricular foramen.CSF is formed bychoroid plexuses in the two lateral ventricles and flows through several structures, including the third ventricle and the cerebral aqueduct of Sylvius, before it enters the subarachnoid space. Most of the CSF produced daily is reabsorbed into thearachnoid villi, which are projections from the subarachnoid space into the venous sinuses of the brain. Arachnoid villi arevery permeable and allow CSF, including protein molecules, to exit easily from the subarachnoid space into the venoussinuses, including the superior sagittal sinus.CSF flows in one direction through the arachnoid villi (most of which are located in the subarachnoid space of the cerebrum), which have been compared with pressure-sensitive valves. When CSF pressure is greater than venous pressure, CSFleaves the subarachnoid space. As pressures are equalized, the valves close.22 l Nursing2018 l Volume 48, Number 12Copyright 2018 Wolters Kluwer Health, Inc. All rights reserved.www.Nursing2018.com
most reliable absorption of the diverted CSF.3 Another less commonCSF shunt option may be chosen if aVPS is contraindicated (for example,because of recent or impending abdominal surgery, recent peritonitis,or multiple abdominal adhesions).6Other CSF shunt options includelumbar-peritoneal, ventriculo-atrial,ventriculo-pleural, or ventriculogallbladder shunting.13VPS systems have four basic components: the proximal (primary orinflow) catheter, the reservoir, a oneway valve, and the distal (terminal oroutflow) catheter.5,6,8,13 The proximal catheter, which drainsCSF from the ventricle, typicallyoriginates in one of the two lateralcerebral ventricles. The proximal catheter connects toa reservoir in the overlying subcutaneous tissue. Although not alwaysused, a reservoir provides support tothe proximal catheter, which can prevent kinking as it curves exiting theskull. It is also useful as an access toobtain CSF samples and for ICPmonitoring. From the reservoir, a one-way valvecontrols CSF flow into the distalcatheter. The distal catheter is tunneled subcu-Signs and symptomsof hydrocephalus inolder children andadults28 headacheincreased ICPanorexialethargy or restlessnessdeteriorating mental statusdifficulty walkingdiplopiaincontinenceirritabilitynausea and vomitingseizures.www.Nursing2018.comThe shunt valve isengineered to controlICP over a range ofpostural positions andpressures.taneously and commonly terminatesin the peritoneal cavity via a separateincision. Shunted CSF is then absorbed by the peritoneal cavity.To prevent infection associatedwith shunt placement, antibioticimpregnated shunt systems areincreasingly being used.14CSF shunt valve typesand functionWithin the shunt system, the valvefunctions as a flow-resistance mechanism and is engineered to controlICP over a range of postural positions and pressures. Most shuntvalves operate on the difference between the pressure at the proximalcatheter tip and the pressure at thedrainage end. This pressure gradientis called differential pressure (DP).15CSF shunt valves have either fixedor programmable (adjustable) pressure settings. Fixed shunt valves,which are not programmable, haveopening and closing pressures set bythe manufacturer and are not adjustable. They function as a pop-offvalve and have fewer parts and arepotentially associated with fewercomplications. However, if the CSFdrainage rate needs to be adjusted, afixed valve cannot be reprogrammedand the patient will need anothersurgical procedure.6,8,15With programmable valves, theopening and closing pressures can beadjusted without the need for a surgical procedure. Using a transdermalmagnetic device, a low-pressure setting can be changed noninvasively toa medium-pressure setting. Althoughthe programmable valves are moreexpensive than fixed valves, theymay be associated with fewer surgeries as the programmable valve can beadjusted based on changes in thepatient’s clinical status.6,8,18CSF flow dynamicsSiphoning of CSF is a posture-related“suction” effect on CSF flow dynamics through the shunt system causedby increased hydrostatic pressurewith the patient in the upright position. Siphoning can cause rapid overdrainage of CSF from the brain. Asdiscussed below, overdrainage cancause collapse of the ventricles andtear blood vessels.2,16,17 Based on theresults of the Study of IdiopathicNormal Pressure Hydrocephalus onNeurological Improvement (SINPHONI)and more recently SINPHONI-2 trials,the programmable DP antisiphonvalve is commonly recommended asthe first-line shunt valve to preventoverdrainage.17,18Shunt valve designs include slit,miter, diaphragm, and spring-loadedball-in-cone. Shunt valves can be setat a fixed opening and closing pressure or can be externally programmed using magnetic tools.16This is useful for the patient whoseDecember l Nursing2018 l 23Copyright 2018 Wolters Kluwer Health, Inc. All rights reserved.
CSF drainage needs will change overtime.Note that programmable shuntvalve settings must be checked andconfirmed following MRI, whichcould potentially redial a programmable shunt to an inappropriatesetting. If uncorrected, this couldlead to significant complicationsrelated to over- or underdrainageof CSF.19Perils of CSF over- andunderdrainageThe goal of cerebral ventricularshunting is to regulate the flow ofCSF in order to control the volumeof CSF, ventricular dilation, andICP.15 CSF overdrainage can result inthe cerebral ventricles shrinking orcollapsing, causing the meningesto pull away from the inner surface of the skull. Overdrainage cancause a condition called slit-ventriclesyndrome, which is more common inchildren and in young adults whohave had a shunt in place sincechildhood. Slit ventricle syndromecan cause severe but intermittentheadaches that are often relievedonly by lying down.20-22 In adults,overdrainage can tear arterial orvenous blood vessels, which canbecome a neurosurgical emergency.6CSF underdrainage causes thecerebral ventricles to enlarge in conjunction with signs and symptoms ofhydrocephalus. When underdrainageoccurs, the patient may need ashunt revision or, if the valve can beexternally adjusted, the valve settings can be interrogated and resetmagnetically.6,22VPS complicationsShunt malfunction and infection arethe most common VPS complications,according to the HydrocephalusAssociation.22 Obstructions causingshunt malfunction are often due toCSF protein or debris buildup. TheAlthough the risk ofshunt complicationsis highest in the firstyear following shuntplacement, they canoccur at any time.shunt can become obstructed at anysection of the system, from the ventricular catheter in the brain to thedistal catheter.22 Because a VPS obstruction leads to increased ICP, signsand symptoms include headache,vomiting, lethargy, irritability, andconfusion.23 The VPS can also malfunction if the catheter disconnects,migrates, or fractures.3Infection may develop when theshunt is colonized by skin flora.Staphylococci are the most commoncause.13,24 An estimated 8% to 10%of CSF shunts become infected, mostwithin the first 4 to 6 months afterplacement.13Shunt infection can lead to abscessformation or shunt occlusion. If thepatient develops an infection, theshunt will probably need to berevised.3Additional biologic complicationsinclude: abscess. When the patient with aVPS complains of abdominal pain,the patient must be assessed forformation of an abdominal abscess.Abdominal abscess can occur fromshunt contamination or from theshunt migrating into the bowel.3 pseudocyst. This develops when thebody walls off CSF around the terminal portion of the peritoneal catheter.An abdominal CSF pseudocyst, alsocalled CSFoma, is a hallmark ofshunt infection. The incidence ofpseudocyst formation is estimated at0.7% to 10%.13 It can necessitateremoval of the VPS and treatmentwith appropriate antibiotics prior toVPS replacement. A pseudocyst maydevelop at any time—within monthsof VPS placement or years later.3,25 subdural hematoma (SDH), a collection of blood between the dura andthe arachnoid membranes.3 peritonitis, which causes generalsigns and symptoms of infection inconjunction with abdominal pain.3 bowel perforation by the peritonealsection of the distal shunt catheter.3,6The complication rates followinginsertion of a shunt tend to be high,with up to half of patients experiencing some type of complication andrequiring shunt revisions. Thesecomplications often involve an overlap of both biological and mechanicalfactors.3,13Caring for a patient with a VPSImmediate postoperative care includes positioning, managing pain,ensuring proper function of theshunt device, monitoring the
A ventriculoperitoneal shunt (VPS) is the most common type of implanted CSF shunt system.1,2 An estimated 33,000 CSF shunt placement procedures are performed in the US annu-ally, with most being VPS.3 Although VPS placement is a commonly performed neuro-surgical procedure and shunt valves and systems continue toFile Size: 556KBPage Count: 7Explore furtherVentriculoperitoneal Shunt Placement (Inpatient Care .www.drugs.comAbout Your Ventriculoperitoneal (VP) Shunt Surgery .www.mskcc.orgHydrocephalus Nursing Care Planning and Management: Study .nurseslabs.comVentriculoperitoneal shunts: What nurses need to know .journals.lww.comVP SHUNT: CARE AT HOME - Nationwide Children'swww.nationwidechildrens.orgRecommended to you based on what's popular Feedback