Transcription
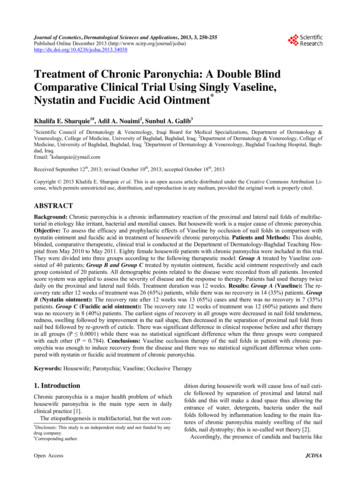
Volume 25, Issue 3December 2009active metabolites stimulate sebaceous gland activity,leading to an increase in sebum production. When hyperkeratinization occurs during the natural sloughingprocess, sebum mixes with clumped keratinocytes.This clumping leads to plugging of the follicle, thuswidening the follicle and producing a favorable environment for bacteria, such as Propionibacterium acnes.Subsequently, primary acne lesions form, appearing asblackheads, also known as open comedos. After development of a blackhead, trauma or inflammation to thefollicles may ultimately lead to the formation of closedcomedos, or whiteheads.1,3 A variety of factors increase the risk for acne vulgaris (Table 1).MANAGEMENT OF ACNEVULGARIS: A REVIEWJennifer D. Billman, Pharm.D. CandidateAcne vulgaris is a common skin disorder causedby abnormal hyperkeratinization and overproduction of sebum by the sebaceous gland.Acne first presents early in adolescence and often continues into early adulthood, negatively affecting quality of life. This article will review the current treatment options for acne vulgaris.1TREATMENT OF ACNEVarious therapies are available for the treatmentof acne vulgaris, including topical and oral agents Preferred therapies differ based on the severity of diseasepresentation.EPIDEMIOLOGYMild-to-Moderate Acne: Topical AntibioticsTopical antibiotics including erythromycin andclindamycin, are effective and well tolerated for thetreatment of acne vulgaris. However, because antibiotics may potentially decrease sensitivity of P. acnes, theuse of these agents should be limited.4 Erythromycin isused alone for inflammatory acne or in combinationwith zinc, which helps the antibiotic penetrate into thepilosebaceous units. Clindamycin inhibits P. acnes andAcne may be psychologically impacting in late adolescence, leading to depression and diminished qualityof life. In the United States, acne affects about 40-50million people1 – impacting nearly 80% of the population between 12-25 years – without gender, ethnicityor race prevalence differences. The onset of acne vulgaris varies within age groups, but is more prevalentduring the onset of puberty, and can continue to be aproblem throughout early adulthood.2ETIOLOGY & PATHOPHYSIOLOGYINSIDE THIS ISSUE:The origin of acne vulgaris is complex, but atleast four primary factors are associated with its development, including increased sebum production,sloughing of keratinocytes, bacterial growth and colonization, and inflammation and immune system response. At puberty, stimulation of androgens, especially testosterone, is enhanced. Testosterone and itsPharmaNoteMANAGEMENT OF ACNE VULGARIS: A REVIEWDRONEDARONE: A NEW OPTION FOR ATRIALFIBRILLATION1Volume 25, Issue 3December 2009
Table 1: Risk factors for acne vulgaris.Environmental Factors:High-humidityProlonged sweatingIncrease in skin hydrationExposure to dirt or vaporized cooking oil or certain chemicalslike petroleum derivativesCosmetic Use:MoisturizersTanning oilsCocoa butterHormonal Factors:MenarcheHigh-androgenic progestin birth controlEmotional Factors:Severe/prolonged period of stressPhysical Factors:Occlusive clothingHeadbandsHelmetsFriction-producing devicesMedication deSteroidsAzathioprineQuinineRifampinAdapted from Haider A, et. al.3possesses comedolytic and anti-inflammatory properties.1Topical antimicrobial combination therapy is moreeffective than monotherapy.1,4 A randomized, parallel,vehicle-controlled trial by Lookingbill and colleaguesevaluated 334 patients over an 11-week once-nightlypreparation study. Evaluation was performed onweeks 2, 5, 8 and 11 for lesion counts, global responserate and irritant effects of clindamycin plus benzoylperoxide gel, benzoyl peroxide alone, clindamycinalone or vehicle gel.5 The combination of clindamycin/benzoyl peroxide significantly improved patient globalresponse and reduced inflammatory and noninflammatory response compared to clindamycinalone, benzoyl peroxide alone, or the vehicle gel.Monotherapy with clindamycin or benzoyl peroxidecompared to the vehicle gel resulted in significant improvement in patient global response and a reductionin inflammatory and non-inflammatory response. Allof the treatment options were well tolerated.5 Table 2summarizes the clinical studies of various productsused to treat acne vulgaris, including topical antibiotics.most effective when used in combination with topicalantibiotics or benzoyl peroxide (Brevoxyle ).1A meta-analysis by Leyden and colleagues, evaluating topical tazarotene in mild to moderate acne, foundthat tazarotene was well tolerated and effective for thetreatment of acne vulgaris, regardless of patientspecific factors, including acne severity, skin type, sexor ethnicity. Six comparative, multicenter, doubleblind, randomized studies of monotherapy with tazarotene 0.1% gel or cream were analyzed, encompassing 468 patients who exhibited moderate to complete clearing at 12 weeks. Both inflammatory and non-inflammatory lesion counts declined substantiallywith both formulations over the treatment period.Furthermore, both formulations were well-tolerated.8In a 3-way retrospective, investigator blinded, photographic review, investigators evaluated the efficacy oftazarotene 0.1% gel, adapalene 0.1% gel, tretinoin0.1% microsponge, and tretinoin 0.025% gel for thetreatment of inflammatory acne. The authors concluded that all formulations showed significant clinicalimprovements compared to tazarotene 0.1% cream(vehicle).7Mild-to-moderate Acne: Topical RetinoidsThe available topical retinoids used for acne vulgaris include tretinoin (Retin-A ), adapalene(Differin ) and tazarotene (Tazorac ) (Table 3).These agents work by reducing obstruction within thefollicle.4,6,7 Such products are considered first-line forthe treatment of mild-to-moderate inflammatory acneand comedonal acne.2 Additionally, these agents arepreferred for maintenance therapy of acne in order topreserve the use of antibiotics.4 Topical retinoids areMild-to-moderate Acne: Combination therapyRecent guidelines suggest that combination therapy with topical retinoids and antimicrobial agentsachieves significantly greater and faster clearing ofacne compared with antimicrobial therapy alone.2Combination therapies utilize agents with complimentary mechanisms of action to target multiple etiological factors simultaneously.2,8Gollnick and colleagues recently conducted a randomized, double-blind, placebo-controlled study toPharmaNote2Volume 25, Issue 3December 2009
Table 2. Clinical studies summary.STUDYMETHODSSTUDY GROUPSRESULTSLookingbill, etal.3(1997)11-week, RCT, PL(n 334)Study groups:Clindamycin BPO gelBPO gelClindamycin gelPlacebo (vehicle gel)Leyden, et al.9(2004)6-comparative MC, DB, Rstudies evaluated 468patients with mildmoderate acneTazarotene 0.1% gelTazarotene 0.1% creamLeyden, et al.5(2005)3-way RS, IB, photographic review evaluating efficacy of topicalretinoidsGollnick et al.8(2009)DB, RCT evaluatingsafety and efficacyTazarotene 0.1% gelAdapalene 0.1% gelTretinoin 0.1% microspongeTretinoin 0.025% gelTazarotene 0.1% creamAdapalene 0.1% BPO 2.5% gelAdapalene 0.1%Adapalene 2.5%BPO 2.5%Vehicle gelClindamycin BPO showed SS (P 0.001) good/excellentPGR, ß in inflammatory and non-inflammatory response and was significantly superiority to clindamycin,BPO, or vehicle gel alone.Clindamycin and BPO alone were SS (P 0.001) vs. vehicle gel in PGR, ß in inflammatory and non-inflammatoryresponse.Both groups showed:Moderate clearing after 12 weeksStatistical ß in inflammatory and non-inflammatorylesionsWell toleratedAll formulations showed significant clinical improvements in inflammatory acne vs. to vehicle.Meta-analysisAdapelene BPO was SS more effective (P 0.001) atweeks 8, 12, and end-point than monotherapy and SSmore effective (P 0.05) at weeks 2 and 4 than vehicleonly.A significant difference in lesion counts from baselineas early as the 1st week.Equal tolerability in all groups.More AEs with adapalene-BPO early in therapy, butonly transient.Krunic, et al.1227 females 18-43 withSpironolactone 30mcg EE/3mg85% subjects had complete clearing of lesions or excel(2008)severe papular or NCDRSPlent improvementfacial acne7.4% had mild improvement7.4% had no improvement.Palombo-Kinne, MN, MC, 3-arm, DB, RCT, Completed 6 cycles of either:EE/DNG was superior to PL and non-inferior to EE/CPAet al.13women 16-45 with mildEE/DNG,(P 0.05).(2009)to-moderate facial acneEE)/ CPA, orRates of ß in inflammatory lesions were -65.6 /-29.9%PLfor EE/DNG, 64.6 /-31.2% for EE/CPA and 49.4 /-41.0%for PL.Percentages of pts with improvement of facial acnewere 91.9% for EE/DNG, 90.2% for EE/CPA and 76.2%for PL.Jones, et al.14RCT, 76 pts with severeIsotretinoin 0.1mg/kg/day to80% ß in total acne after 4 months.(1983)acne0.5mg/kg/day89% ß in total lesions when a 1.0mg/kg/day dose wasused.RCT randomized controlled trial; MN multinational; MC multicenter; DB double-blind; RS retrospective; IB investigator-blind; R randomized; SS statistically significant; PGR patient global response; NC nodulocytic; y/o years old; PL Placebo; Pts Patients.assess the safety and efficacy of adapalene 0.1% benzoyl peroxide (BPO) 2.5% combination gel and 0.1%adapalene, 2.5% BPO, or a vehicle gel. The authors reported that combination therapy was more effective(P 0.001) at weeks 8 and 12, and at study end compared with BPO monotherapy and a vehicle gel. Moreover, combination therapy was more effective(P 0.05) at weeks 2 and 4 compaed with vehicle-only.A significant difference in lesion counts from baselinewas reported as early as the 1st week. Adverse effectswere more prevalent in the early phase of treatmentwith combination therapy, but these effects were transient. This study showed that combination therapywas significantly better, synergistically efficaciousPharmaNotewith a faster onset, and had an equivalent safety profile when compared to the monotherapies.8Mild-to-Moderate Acne: Hormonal TherapyHormonal therapy produces anti-androgen effects,which leads to a decrease in testosterone circulating inthe body. Consequently, sebaceous gland stimulationis prevented, reducing sebum production.3,10 FDAapproved hormonal therapies consist of oral contraceptive agents that contain norgestimate with ethinylestradiol (Ortho-Tri-Cyclen ) and norethindrone acetate with ethinyl estrodial (Estrostep ), as well as theanti-androgenic agent, spironolactone (Table 4).4Anti-androgens, such as spironolactone or cypro3Volume 25, Issue 3December 2009
PharmaNote4Volume 25, Issue 3December 2009Inhibits bacterial DHFS, interferingwith FA synthesis, an essential component for bacterial developmentMechanism similar to sulfacetamide, but for dermatologicaldisorder; possible immunomodulatorBinds specific nuclear RAR, penetrating deep into hair follicles,modulating cell differentiation andkeratinization. Also has potent AIand comedolytic propertiesExact mechanism unknown: inhibitsmicrobial protein synthesis; BS atlower doses; BC at higher doses.Also direct AI and AK effectsReleases FR oxygen species oxidizesbacterial proteins. Also keratolyticactivityCetamide , Klaron ,Ovace , RE-10 wash , Rosula NS , Seb-Prev Aczone Differin Azelex , Finacea Finacea Plus , Finevin Acne-10 , Acne-5 Acneclear , Benoxyl Benoxyl , Benprox , Benzac ,Benzac , Benzagel , Benziq , Brevoxyl , ClearPlex ,Desquam EX , Fostex ,Inova Lavoclen , othersAvage , Tazorac Sulfacetamide(antibiotic)AdapeleneAzelaic AcidBenzoyl Peroxide0.1% (creams or gel)Apply a thin film on theaffected area in the evening.2.5% to 10% (creams, gelsor lotions)Apply once daily andgradually increase to fourtimes daily.Finacea 50gm: 140.99Azelex 50gm: 188.99(NO GENERIC)Contact dermatitis, erythema, hypertrichosis, infection, pruritus, rash(unspecified), skin hypopigmentation, skinirritation, xerosis.Contact dermitis, erythema, pruritus, rash(nonspecific), skin irritation, xerosisDesquamation, burning/stinging, xerosis,erythema, pruritus, skin irritation, skinpain, fissuring, localized edema, and skindiscoloration.45gm tube (0.1%,0.3%): 203.99Erythema, burning, xerosis, skin irritation,photosensitivity, pruritus.297gm lotion:BPO 4% - 55.59BPO 8% - 57.5960gm tube cream:0.05% - 272.990.1% - 291.9960gm gel tube:BPO-10 - 29.09BPO-5 - 22.8960gm tube: 294.99RE-10 Wash: 87.99Hypersensitivity to sulfacetamide, whichmay progress to lupus like syndrome.Photosensitivity(Most problems are seen in leprosy patients)2% 60gm:Gel 34.99Soln 14.991% 60gm:AVP 48.67COSTPruritis, acute generalized exanthematouspustulosis, nausea, vomiting, diarrhea,and anorexia.Pruritis, acute generalized exanthematouspustulosis, burning, xerosis, erythema,oiliness, peeling.SIDE EFFECTS100gm tube gel:0.05% - 451.990.1% - 383.99TrentinoinAltinac , Atralin Binds to RAR, modifying gene ex0.025%, 0.04%, 0.05%, orBurning, stinging, xerosis, peeling, ery45gm tube:Avita , Renova , Retin-A ,pression, thus affecting protein0.1% (cream, liquid, gel)thema, and pruritus. Also, skin hyper- or0.01% gel - 96.59Trentin-X , Vesanoid synthesis, epithelial cell growth andApply to affected areahypo-pigmentation, photosensitivity.0.025% cream - 52.99differentiation. Also has AK effects.once daily at bedtime.0.025% gel - 85.990.05% cream - 101.990.1% cream - 85.59DHFS dihydrofolate synthetase; FR free radical; RAR retinoic acid receptor; BS bacteriostatic; BC bacteriocidal; AI anti-inflammatory; AK anti-keratinization; FA folic acid; AVP average variable priceTazoreteneExact mechanism unknown; Bindspecific nuclear RAR, and exertseffects on keratinocyte differentiation, proliferation, and inflammation.Inhibits 50s ribosomal subunit ofbacteria, which inhibits proteinsynthesisAkne Mycin , E-Mycin ,EMGEL , Ery-Pad , ErygelR Erythromycin(antibiotic)0.1% (cream or gel) &0.3% (gel)Apply to affected areasonce daily before bedtime.15%-20% (gel or cream)Apply to affected areastwice daily.1% (cream, solution,pads)Any topical applied onaffected area twice daily.1.5% - 2% (solution, gel,ointment)Any topical applied onaffected area twice daily.10% lotionApply on affected areatwice daily.5% gelApply on affected areatwice daily.Inhibits 50s ribosomal subunit ofbacteria, which inhibits proteinsynthesisCleocin T, Clindagel Clindesse , Clinda-derm ,Evoclin /DOSESMECHANISMBRANDSDRUGTable 3. Topical agents for the treatment of acne vulgaris.11,15
PharmaNote5Volume 25, Issue 3December 2009MonoNessa , Ortho TriCyclen Lo , OrthoCyclen , Ortho TriCylcen , Sprintec , TriSprintec , Previfem , Tri-Previfem , Trinessa Accutane , Amnesteem , Clavaris , Sotret Ethinyl Estradiol;NorgestimateIsotretinoinArestin , Cleeravue-M ,Dynacin Minocin ,Myrac , Solodyn rsibly binds to 30s subunitof bacteria, which blocks mRNAand tRNA function, thus blockingprotein synthesis.1mg/kg once dailygiven for 12 weeks100 mg twice dailyon day 1, then100mg once daily50-200 mg/day0.5-1 mg/kg/day intwo divided dosesfor 15-20 weeks.Shows reversible inhibition ofsebum production by reductionin sebaceous glands, and possible inhibition of follicular keratinization. Also might have AIeffects.Acts as an ARA, competitivelyinhibiting TT, a steroid that triggers secretion of oil by sebumglands, leading to acne. Inhibition leads to decrease in sebumproduction.Prolonged use ( 2-4 months) neededfor acne resolution.STRENGTH/DOSESSome have less/no androgenicactivity, thus preventing TT production, and are less likely tostimulate/aggravate sebaceousglands.MECHANISMAA, anorexia, dyspepsia, enterocolitis,glossitis, N/V/D, pancreatitis, pseudomembranous colitis, and stomatitis,asthma exacerbation, cough, dyspnea,bronchospasm, pneumonitis, bonediscoloration, photosensitivity, rash,nail discoloration alopecia, vaginal,rectal, or oral candidiasis,Diarrhea, nausea, vomiting, epigastricdistress, anorexia, esophagitis, vaginalcandidiasis, photosensitivity, rashes,nail discoloration, AGEP, neutropeniaand eosinophiliaCardiac arrhythmias, hyperkalemia,gynecomastia, libido decrease, menstrual irregularity, post-menopausalbleeding, breast tenderness, hirsutism,amenorrheaCheilitis, xerosis, xerostomia, epistaxis,peeling, pruritus, acneiform rash,alopecia, eczema, flushing, hirsutism,impaired wound healing, infection,photosensitivity, seborrhea, skin fragility, skin hyper-, hypopigmentation,urticaria.Menstrual irregularity, breakthroughbleeding, spotting in the 1st 3 months,migraines, venous thrombosis embolism, hypertension, vaginal discharge,vaginal irritation, mood/personalitychanges, ocular disorders, Melasma,photosensitivity, bleeding of the gums,rash, urticaria, erythema, alopecia,hirsutism, can exacerbate acne vulgarisSIDE EFFECTS50mg (30 tablets): 97.59 (G)50mg (30 tablets): 35.79 (G)25mg (30 tablets): 11.19(FOR GENERIC)Accutane (B) 40mg (30 tablets): 849.9940mgAVP (30 tablets): 272.49(ALL GENERICS)28 tablets (ALL)MonoNessa : 27.99Ortho-Tri-Cyclen Lo : 62.59 (B)Tri-Lo-Sprintec : 54.99 (G)Ortho-Tri-Cyclen : 47.39 (B)Tri-Sprintec : 31.39 (G)Trinessa : 47.39 (G)Ortho-Cyclen : 48.49Sprintec : 27.99Yaz/Yasmin: 74.59Ocella: 59.99 (G)COSTARA androgen receptor antagonist; RAR retinoic acid receptor; TT testosterone; AA abdominal pain; N/V/D nausea, vomiting, diarrhea; AGEP acute generalized exanthematouspustulosis; AVP average variable price; G generic; B brandAdoxa , Adoxa, Pack ,Alodox , Atridox , Avidoxy , Doxy , Doxy100 , Oracea , Oraxyl Periostat , Vibra-Tabs ,Vibramycin Aldactone , Spirono Ocella , Yasmin , Yaz28 Drospirenone; EthinylEstradiolSpironolactoneBRANDSDRUGTable 4. Oral agents for the treatment of acne vulgaris.11,15
terone, and oral estrogens, such as ethinyl estradiol,decrease androgen levels in patients with acne. Krunicet. al., evaluated the safety and efficacy of dailysprionolactone (SL) 100 mg ,ethinyl estradiol 30 mcg,and drospirenone (EE/DRSP; Yasmin ) 3 mg. Thestudy found that 85% of subjects had complete clearing of acne lesions or excellent improvement, 7.4%had mild improvement, and 7.4% had no improvement. No significant increase in serum potassium orother side effects were observed in any subjects. Theauthors concluded that EE/DRSP combination therapyand SL 100 mg daily was well tolerated and efficaciousin the treatment of severe papular and nondulocysticacne in women.12In a multinational, multicenter, three-arm, doubleblind, randomized trial, Palombo-Kinne evaluatedhealthy women between the age of 16 and 45 withmild to moderate facial acne. Participants were randomly assigned to ethinylestradiol (EE)/dienogest(DNG), ethinylestradiol (EE)/cyproterone (CPA) orplacebo for six cycles. The primary efficacy variableswere the percent change from baseline to cycle 6 ininflammation and total lesion count and the percentage of patients with improvement in acne evaluated bythe Investigator Global Assessment. The study foundthat EE/DNG was superior to placebo and non-inferiorto EE/CPA. The rates of reduction ( SD) in inflammatory lesions were -65.6 /-29.9% for EE/DNG, -64.6 /31.2% for EE/CPA and -49.4 /-41.0% for placebo. Thepercentages of patients with improvement of facialacne were 91.9% for EE/DNG, 90.2% for EE/CPA and76.2% for placebo. The authors concluded that EE/DNG was superior to placebo and as effective as EE/CPA for treatment of mild to moderate acne.13teratogenicity, men and women of child-bearing ageare asked to register and comply with the FDA approved iPLEDGE program. This program is a risk management program that prevents isotretinoin exposureto the fetus.SUMMARYMany well-tolerated and effective options areavailable for the treatment of acne vulgaris, dependingon the type and severity of disease. Topical retinoids,antibiotics and BPO are effective for mild-to-moderateacne, while oral isotretinoin and hormonal therapy areeffective for more severe cases. In addition, combination therapy with clindamycin and BPO is more effective than treatment with either alone. Management ofthis common dermatologic disorder may contribute toa better quality of life. REFERENCES1.Pharmacotherapy: A Pathophysiological Approach. Joseph T.DiPiro, Robert L. Talbert, Gary C. Yee, Gary R. Matzke, BarbaraG. Wells, L. Michael Posey (Eds). 7th edition. Chapter 100. AcneVulgaris: Treatment: Acne Vulgaris. Accesspharmacy. http://www.accesspharmacy.com/content.aspx?aID 32121232. Thiboutot D, Gollnick H. New insight into the management ofacne: An update from the Global Alliance to Improve Outcomes in Acne Group. J Am Acad Dermatol 2009;60:S1-50.3. Haider A, Shaw J. Treatment of Acne Vulgaris. JAMA:2004;292(6):726-35.4. Strauss JS, Krowchuk DP, Leyden JJ, et al. Guidelines of carefor acne vulgaris management. J Am Acad Dermatol 2007;56(4):651-63.5. Lookingbill DP, Chalker DK, Lindholm JS, et al. Treatment ofacne with a combination clindaymycin/benzoyl peroxide gelcompared with clindamycin gel, benzoyl peroxide gel andvehicle gel: combined results of two double blind investigations. J Am Acad Dermatol 1997;37:590-5.6. Fox Lindy P, Merk Hans F, Bickers David R. Chapter 62: Dermatological Pharmacology. Laurence L. Brunton, John S.Lazo, Keith L. Parker (Eds): Goodman & Gilman's The accesspharmacy.com/content.aspx?aID 9593377. Leyden JJ, Shalita A, Thiboutot D, et al. Topical retinoids ininflammatory acne: A retrospective, investigator-blinded,vehicle-controlled, photographic assessment. Clin Ther2005;27:216-24.8. Gollnick HPM, Draelos Z, Glenn MJ, et al. Adapelene-benzoylperoxide, a unique fixed-dose combination topical gel for thetreatment of acne vulgaris: a transatlantic, randomized, double-blind controlled study in 1670 patients, Br J Dermatol2009 [Epub ahead of print].9. Leyden JJ. Meta-analysis of the topical tazarotene in the treatment in the treatment of the mild to moderate acne. Cutis2004;74(supp 4):9-15.10. George R., Clarke S, et al. Hormonal Therapy in Acne. SeminCutan Med Surg 2008:27(3):188-96.11. Gold Standard, Inc. Clinical Pharmacology [database online].Severe Acne: Oral IsotretinoinIsotretinoin (Accutane ) is a naturally occurringmetabolite of Vitamin A, and is indicated for the treatment of severe acne. Isotretinoin works by reducingthe size of the sebaceous gland, suppressing sebumproduction, and normalizing follicular epithelial desquamation (Table 4).14 Several studies show isotretinoin to be effective in severe acne. In a randomizedcontrolled trial with 76 patients, isotretinoin showedan 80% reduction in total acne after 4 months. Treatment doses ranged from 0.1mg/kg/day to 0.5mg/kg/day. An 89% reduction in total lesions was observed atthe 1.0mg/kg/day dose.10,14 Although the drug is effective for severe acne, reported side effects may be severe, including inflammation of the lips, which is doserelated. In addition, xerosis, xerostomia, epitaxis, peeling, pruritus, nausea/vomiting, altered lipid profiles,and most importantly, teratogenesis may occur withany amount of isotretinoin ingestion.10 Because of thePharmaNote6Volume 25, Issue 3December 2009
12.13.14.15.rhythm. In the AFFIRM trial, 67% of patients in therhythm control group were started on amiodarone orsotalol; and at the end of the study 66% of the patientshad tried amiodarone at least once.5 An advantage ofamiodarone is the low poarrhythmic risk of in left ventricular (LV) hypertrophy, heart failure (HF), coronaryartery disease, and post myocardial infarction.3 However, this agent is limited by extra-cardiac toxicitiesincluding pulmonary fibrosis, hepatic and thyroid dysfunction, neurological disorders, blue-gray skin discoloration, and corneal deposits. In addition, amiodaronehas a complicated dosing schedule and interacts withsome cardiovascular (CV) agents including warfarinand digoxin.3,6 Dronedarone (Multaq ) is an amiodarone analogue manufactured by Sanofi-Aventis and recently approved by the FDA in July 2009. The structure of dronedarone differs from amiodarone by theabsence of iodine and the presence of a methanesulfonyl group that decreases lipophilicity. Thesechanges were intended to reduce accumulation in tissues to prevent thyroid and other peripheral adverseeffects.7 This article will review the efficacy, safety andtolerability of dronedarone for maintenance of sinusrhythm in AF.Available: http://www.clinicalpharmacology.com. Accessed:July 15, 2009.Krunic A, Ciurea A, Scheman A, et al. Efficacy and tolerance ofacne treatment using both spironolactone and a combinedcontraceptive containing drospirenone. J Am Acad Dermatol2008;58:60-2.Paloma-Kinne E, Schellschmidt I, Schumacher U, et al. Efficacyof a combined oral contraceptive containing 0.030 mgethinylestradiol/2 mg dienogest for the treatment of papulopustular acne in comparison with placebo and 0.035 mgethinylestradiol/2 mg cyproterone acetate. Contraception2009 ;79(4):282-9.Jones DH, King K, Miller AJ, et al. A dose response study of 13cis retinoic acid in acne vulgaris. Br J Dermatol 1983;108:33343.Lexi-Comp OnlineTM , 2009. Accessed: July 15, 2009. crlonline.DRONEDARONE: A NEWTREATMENT OPTION FORATRIAL FIBRILLATIONAna Marquez, Pharm.D. CandidatePHARMACOLOGY AND PHARMACOKINETICS (PK)Dronedarone is a benzofuran derivative that haselectrophysiological properties of all VaughanWilliams antiarrhythmic drug classes. Specifically,dronedarone blocks sodium and calcium channels,demonstrates noncompetitive antiadrenergic actionsand prolongs the action potential and refractory periods.8 Oral dronedarone prolongs the PR and QTc interval in a dose-dependent manner. Heart rate is not affected by oral administration of 400 mg twice dailyand is reduced by 4 beats/min with 800 mg twicedaily.9Dronedarone undergoes extensive first-pass metabolism and has a low bioavailability that is increasedby food. A 2-fold increase in dose results in an approximate 2.5- to 3.0- fold increase in Cmax and AUC,indicating nonlinear PK. The main active circulatingmetabolite is formed by N-debutylation. This Ndebutyl metabolite has one-tenth to one-third the potency of dronedarone. Time to peak plasma concentration of dronedarone and its primary metabolite is 3to 6 hours under fed conditions. Dronedarone reachessteady-state concentrations after 4 to 8 days of oraladministration of 400 mg twice daily. Steady-stateCmax and AUC are similar for both parent and activemetabolite. Dronedarone moderately inhibits CYP3Aand CYP2D6. 10Females have an approximate 30% greater expo-Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia affecting approximately 2.2 million people in the US.1 AF isprevalent in 1% of adults younger than 55 and approaches 10% in those older than 80.2 AF results inhemodynamic and thromboembolic complications,and increases the rate of ischemic stroke 5 fold.1,3Hospitalization rates due to AF have increased by 66%during the past 20 years resulting in a significant public health burden. This cost will continue to rise due toan aging population.3,4 One of every six strokes occursin a patient with AF with mortality rates doubled compared to patients in sinus rhythm.Treatment for AF consists of ventricular rate control or sinus rhythm control with concomitant anticoagulation therapy. Use of long term antiarrhythmictherapy may be needed in the majority of patients dueto the high rate of recurrence after electrical or pharmacological cardioversion. Antiarrhythmic drugs alsomay be started when symptoms are not suppressedwith rate control therapy alone. But the choice of antiarrhythmic agent must take into account the safetyprofile of the drug as well as the underlying heart disease of the patient.3Amiodarone, a class III antiarrhythmic drug, is effective and commonly used for maintenance of sinusPharmaNote7Volume 25, Issue 3December 2009
sure to dronedarone than males. In a cross study, Japanese men showed a 2-fold increase in dronedaronelevels compared to Caucasian men after a single doseof 400 mg. Patients 65 years of age have a 23%higher exposure than younger patients. Dronedaroneexposure is increased by 30% and the N-debutyl metabolite is decreased by about 50% in patients withmoderate hepatic impairment. Dronedarone’s PK havenot been studied in individuals with severe hepaticimpairment. No significant PK differences were observed in patients with mild to severe renal insufficiency relative to patients with normal renal function.10 In animal studies, dronedarone distributeswidely throughout the body, crosses the placenta andblood brain barrier, and is excreted into breast milk.9These PK properties differ significantly from those ofamiodarone (Table 1).total of 25 patients (8.1%) died in the dronedaronegroup and 12 patients (3.8%) died in the placebogroup. In the dronedarone arm, 24 out of the 25deaths were caused by CV events. Ten of these CVdeaths were caused by worsening HF. In the placeboarm, 9 out of the 12 deaths were caused by CV events.Two of these deaths were from worsening HF. Thenumber of patients having a first hospitalization for anacute CV event was more common in the dronedaronegroup (71 patients) compared to placebo (50 patients). Overall, rates of hospitalization due to any CVcause were higher in the dronedarone group. Themain cause of these hospitalizations was worseningHF (35 patients taking dronedarone vs. 30 taking placebo). The only significant laboratory adverse eventmore common with dronedarone was an increase inserum creatinine. This increase in serum creatininewas observed immediately after the start of therapyand returned to baseline after discontinuation ofdronedarone.The authors concluded that dronedarone shouldnot be used in patients with HF and LV systolic dysfunction, and that further studies were needed to analyze the effect of the drug on renal function (Table 2).CLINICAL TRIALSANDROMEDAANDROMEDA was a rand
Cosmetic Use: Moisturizers Tanning oils Phenobarbital Cocoa butter Ethonamide Hormonal Factors: Menarche High-androgenic progestin birth control Emotional Factors: Severe/prolonged period of stress Physical Factors: Occlusive clothing Headbands Helmets Friction-producing devices Medicati