Transcription
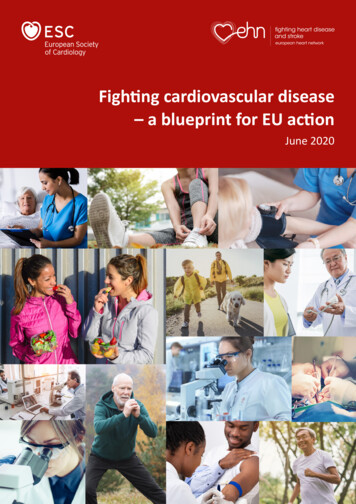
Fighting cardiovascular disease– a blueprint for EU actionJune 2020
Fighting cardiovascular disease –a blueprint for EU actionSubstantial progress in the prevention andtreatment of cardiovascular disease (CVD1) hasresulted in the dramatic decline in prematuredeath from CVD over the last 50 years. Thismay have led to false optimism that CVD needno longer be a public health priority.This paper provides a blueprint for addressingthe huge burden of CVD among the EUpopulation, by putting forward specificrecommendations for an ambitious EU actionplan that addresses cardiovascular health to beimplemented in the current EU mandate.However, this is not the case.We call on EU policymakers to supportthis proposal.In the European Union (EU)2, the burden ofCVD remains greater than that of any otherdisease. Cardiovascular events – mainlymyocardial infarction (heart attack) and stroke– remain, by far, the leading cause of death inthe EU. In addition, millions of people now livewith, and in the aftermath of, CVD.Any notion that “the job is done” isclearly amiss.The development of innovative solutions toensure people’s access to prevention andtreatment of CVD across Europe is a necessaryand urgent priority. Supporting research in CVDby creating a European-wide infrastructure toenable quality of care assessment, harmonisedhigh-quality disease registries, and streamlinedpragmatic randomised clinical trials will notonly improve the health of people living inEurope, but stimulate the pharmaceutical anddevice industry to invest in Europe.Understanding the burden ofcardiovascular disease (CVD)MorbidityMost recent data from the Global Burden ofDisease database estimate that, in the EU,more than 60 million people live with CVD,and that close to 13 million new cases of CVDoccur every year.LIVING WITHWITH CVDLIVINGCVD(EU)(EU)60MILLIONTotal of peopleliving withCardiovascularDisease today13MILLIONNew cases ofCardiovascularDisease each year1 For the definition of CVD please see Appendix 12 In this paper, the EU comprises 28 member statesA blueprint for EU action 1
More patients survive heart attack or stroke,and the pattern of CVD has changed – inparticular, nowadays many patients with CVDare co-morbid (that is, have co-existing renalfailure, cognitive decline, diabetes or otherconditions). This combination has significantadverse effects on patients and puts substantialstrain on health care systems across the EU.DEATHSININ 6565 YEARDEATHSYEAROLDSOLDS 65YEAR OLDSPremature deathfrom CardiovascularDisease17 %24 %MortalityCVD is the number one cause of death in theEU: more than 1.8 million people – equal tothe population of Vienna – die every year as aresult of CVD, accounting for 36% of all deaths— far more than any other condition (as acomparison, cancer accounts for 26% of alldeaths in the EU). This represents, on average,about 5 000 deaths per day in the EU.2 Fighting cardiovascular diseaseMoreover, a large proportion of CVD deaths ispremature. In the EU, 24% of deaths amongmen before age 65, and 17% of deaths amongwomen before age 65, are due to CVD.Notably, the rate of decline in CVD mortalityappears to be tapering. Indeed, for the firsttime in 50 years some EU countries havereported an increase in premature CVDdeath. These adverse trends have beenattributed to an insufficient awareness of CVD,limited and geographically varied investment incardiovascular prevention and treatment, andthe rising prevalence of obesity (and with thatof diabetes, hypertension, dyslipidaemia andatherosclerosis).The economic costThe burden of CVD is not only a health issue,but an enormous economic challenge to healthcare systems in the EU that is expected to growin future years.The most recent data estimate that CVD coststhe EU economy approximately 210 billion ayear. Of that cost, around 53% ( 111 billion) isfor health care costs, 26% ( 54 billion) is due toproductivity losses and 21% ( 45 billion) due toinformal care of people with CVD.
Inequalities in CVD in the EURobust action on CVD has the potential tosignificantly reduce health inequalities in theEU. Inequalities in mortality from CVD accountfor almost half of the excess mortalityin lower socio-economic groups in mostEuropean countries.Geographical inequalities are significant andpersistent in CVD: The prevalence of CVD is higher in Easternand Central European countries andlower in Western, Northern and SouthernEuropean countries. Indeed, in 2017, orlatest available year, the age-standardisedCVD prevalence rate in the EU in men was50% higher in the country with the highestrate (Bulgaria) than in the country with thelowest rate (Cyprus), and in women therate was 60% higher in the countries withthe highest rates (Bulgaria and the CzechRepublic) compared to the countries withthe lowest rates (Italy and Spain). CVD is responsible for 27 million disabilityadjusted life years (DALYs) in the EU (18%).The rates of DALYs lost due to CVD are againhigher in Central and Eastern Europe thanin Northern, Southern and Western Europe. In line with the prevalence data, deathrates from both heart disease and strokeare higher in Central and Eastern Europethan in Northern, Southern and WesternEurope. For example, the age-standardiseddeath rate for heart disease in 2017, or latestavailable year, is 13-fold higher in women inLithuania than in France, and 9-fold higher inmen. For stroke, the age-standardised deathrate is 7-fold higher in women in Bulgariathan in France, and 8-fold higher in men.The single most important contributor toexcess mortality in Eastern European countriesis CVD. While among men less than 50% ofthe excess mortality is due to CVD, in womenthis percentage is 80%.DISPARITIES IN MORTALITY (EU)A woman in Lithuania is13 xmore likely to die fromheart disease than awoman in FranceA man in Bulgaria is8xmore likely to die fromstroke than a manin FranceA blueprint for EU action 3
An action plan for cardiovascular diseaseWhile the organisation and delivery of healthcare are Member States’ competences, the EUcan play a crucial role in tackling the burdenof CVD through policy and regulation, as wellas supporting research and innovation intoCVD prevention and management.Taking into consideration the competences ofthe EU, we propose an action plan on CVD inthe following areas: The need for prioritising prevention ofavoidable CVD The need for promoting innovation andmodernising research regulations toimprove access Better patient care through improveddiagnosis, treatment and managementCARDIOVASCULAR DISEASECardiovascularDisease is thebiggest killerin the EU andthe world3 See Appendix 2 for CVD risk factors4 Fighting cardiovascular disease1 The Need for Prioritising Preventionof Avoidable CVDCVD is often referred to as a lifestyle diseasebecause of its causal link with behaviouralrisk factors (lifestyle determinants). However,as for cancer, CVD is caused by several otherfactors3 and, given the scale of the disease, itwould be more appropriate to refer to CVD as asocietal disease.Many people are already disabled by ill-healthbefore they reach retirement age. Greaterreduction of exposure to the main behaviouralrisk factors – tobacco, unhealthy diet, physicalinactivity and harmful use of alcohol –would increase the number of years lived ingood health.Effective population-wide interventions toprevent CVD have the potential to provideboth human and economic benefits withconsiderable returns on investment.Given that the majority of cases come fromindividuals at low or moderate risk of CVD,small reductions in CVD risk factors across thepopulation will produce large societal gain.
1.1 Food and nutrition1.2 SmokingIn the EU, unhealthy diets are associatedwith over 800 000 deaths from CVD eachyear, accounting for over 40% of all CVDdeaths – 417 000 in men and almost 400 000in women. Dietary risks are responsible foralmost 45% of all the years lost to CVD death ordisability in the EU.Smoking is the second largest cause of CVDafter high blood pressure. It is associatedwith 13% of all CVD deaths in the EU, whichtranslates to almost 250 000 CVD deathsevery year (around 165 000 male and 82 000female deaths).Achieving a CVD health-promoting dietrequires moving away from an animal-baseddiet to a more plant-based diet. CVD-specificnutrients, where target goals at a populationlevel should be reached, are saturated fats (lessthan 10% of calories), salt (less than 5 g of saltper day) and fibre (at least 12.6 g of dietaryfibre per 1000 kcal 3 g per MJ energy).RECOMMENDED EUPRIORITY ACTIONS Set nutrient profiles to underpin nutritionand health claims as required by the ECregulation on nutrition and health claims(EC) No 1924/2006 Adopt rules on simplified front-of-packnutritional labelling Adopt regulations restricting all marketingto children, including digital, of food anddrinks high in fat, salt and sugarThe average prevalence of smoking (daily andoccasional smokers; people older than 15)in the EU is 24%. However, prevalence varieshugely, from just under 17% in Sweden toalmost 35% in Bulgaria.Recent studies increasingly highlight therisks of electronic cigarette use to thecardiovascular system.RECOMMENDED EUPRIORITY ACTIONS Raise minimum tobacco excise duties tothe highest possible level Bring excise duties on “roll yourown” tobacco up to the same level asmanufactured cigarettes Strengthen regulation on e-cigarettesA blueprint for EU action 5
1.3 Physical inactivityLow physical activity is estimated to beresponsible for 140 000 cardiovascular deathsin the EU every year. It causes more deathsamong the female population (77 000) thanamong the male population (63 000).Participation in regular physical activity and/or aerobic exercise training is associatedwith a reduction in the prevalence of andmortality from CVD, while a sedentary lifestyleincreases the risk of CVD by increasing the riskof hypertension, high triglycerides, low HDL(‘good’) cholesterol, diabetes and obesity.RECOMMENDED EUPRIORITY ACTION Encourage the development and approvalof EU funded projects (in particularprojects supported by EU Structural Funds)that have a positive impact on active living1.4 AlcoholHarmful alcohol consumption is estimatedto be responsible for close to 50 000 CVDdeaths in the EU.High alcohol consumption, particularlybinge drinking, increases the risk of CVD byraising blood pressure and blood levels oftriglycerides. Consumption of three or morealcoholic drinks per day is associated withincreased CVD risk.6 Fighting cardiovascular diseaseRECOMMENDED EUPRIORITY ACTIONS Raise minimum excise duties on alcoholicbeverages to the highest possible level Introduce mandatory, front-of-pack energylabelling on alcohol Introduce mandatory ingredients list onalcoholic beverages1.5 Air pollutionAir pollution has been associated with around115 000 cardiovascular deaths per year (6% ofall cardiovascular deaths) in the EU, accountingfor more than 60 000 male deaths and morethan 53 000 female deaths.Exposure to air pollution affects everybody, butit is an amplifying factor for health inequalities,as people living in less affluent areas are oftenmore exposed to it.RECOMMENDED EUPRIORITY ACTION Revise the ambient air quality directiveadopting the WHO Air Quality Guidelinevalues as limit values
2 The need for promoting innovationand modernising researchregulations to improve accessDespite the burden of CVD being greater thanany other disease, research and innovationin CVD is lagging, compared with otherdisease domains. Only one CVD medicinewas approved by the European MedicinesAgency in 2018.The complexity and costs of clinical trials andan unfavourable regulatory framework forfostering innovation are key contributors tothis decline.2.1 The need for promoting research &innovation in CVDResearch funding for CVD is disproportionallylow at EU level, compared with other diseases.CVD and its risk factors feature very little inthe call descriptions for Horizon 2020, and thenumber of EU-funded projects related to CVDis far fewer than those in other clinical areas.The Strategic Research Agenda for CVD, whichwas produced by the ERA-CVD Network incooperation with the European Heart Networkand the European Society of Cardiology,identifies key areas for which clinical research isneeded if we want to succeed in reducing CVDmortality and morbidity. The top five researchpriorities identified are:1. Earlier recognition of cardiovascular disease2. Repair of the heart and blood vessels3. The interaction between CVD andother disorders4. Treatment of chronic heart failure andatrial fibrillation5. Personalised treatment and managementof cardiovascular diseaseRECOMMENDED EUPRIORITY ACTION Recognise key areas of CVD researchas priorities in the Horizon EuropeprogrammeDYING FROMCARDIOVASCULAR DISEASE (EU)DYING FROM CARDIOVASCULAR DISEASE (EU)1.836 % CardiovascularMILLIONCardiovascular Disease deaths per yearDisease26 % Cancer 5000Cardiovascular Disease deaths per day8 % Respiratory2 % DiabetesA blueprint for EU action 7
2.2 Modernise the regulatory framework forthe assessment of the efficacy and safetyof new treatmentsCardiology has one of the strongest evidencebases, yet only about 14% of ESC ClinicalPractice Guideline recommendations arebased on randomised clinical trial evidence,demonstrating the prohibitive cost andcomplexity of clinical trials in CVD.Currently, the cost of randomised controlledtrials and the reluctance of payers to reimbursetherapies that produce effects on moderatesize in very large numbers of eligible patientsare a major threat to the development of newtreatments in CVD, and the reason why severalpharmaceutical companies have moved out ofthe cardiovascular area.To mitigate these worrying trends, innovativeapproaches are urgently needed.These include a regulatory frameworkadapted to the challenges of developing newtherapies, better and more flexible rules forthe conduct of randomised clinical trials,and the development of a European-wideinfrastructure either based on patients’electronic health records or continuouspatient registries that would allowrandomisation at the point of care and lowcost long-term automated capture of efficacyand safety signals within health care systemsor registries for reliable assessment of newtherapies and devices.8 Fighting cardiovascular diseaseFew interventions could have such a majorimpact on the cost effectiveness of regulatorystudies, ultimately leading to better dataand potentially much less expensivetreatments, not only for CVD but for allcommon conditions.Together, such developments would not onlyimprove patient access to better treatments,but also be instrumental in bringinginvestment to and promoting innovationin Europe and would benefit all areas ofmedical research.RECOMMENDED EUPRIORITY ACTIONS Promote and support the developmentof harmonised and comprehensivecontinuous patient registries in CVD, aswell as the digital capability to enable theevidence generated within health systemsto improve the speed and efficiency ofrandomised controlled trials Establish a structured collaborationbetween academic clinical trialists,patients, regulators and industry, tomodernise the International Council ofHarmonisation (ICH) Good Clinical Practice(GCP) standards and make them fit for thedigital era
2.3 Unlocking the full potential of digitaltechnologies for cardiovascular health2.4 Better understand the interactionbetween CVD and cancerDigital technologies may have great potentialin transforming prevention, early detectionand management of cardiovascular disease.In primary prevention for example, mobileapplications, text messaging and monitoringsensors for self-tracking, as well as onlinecounselling, have the potential to identifypeople with high cardiovascular risk, andimprove lifestyle management intervention toreduce cardiovascular risk.Advances in oncological treatment have ledto the improved survival of patients withcancer but have also increased morbidityand mortality due to the cardiotoxicity ofcancer treatment.Digital technologies in health care deliveryprovide the opportunity to redesign andimprove patients’ care after diagnosisand discharge, thanks to innovations intelecommunication technologies (i.e. cardiactelerehabilitation).Furthermore, supporting the digitisation ofhealth systems through the development ofelectronic health records and data repositories,as well as exploiting the potential of artificialintelligence, would play a key role in improvingdiagnosis and treatment of CVD.RECOMMENDED EUPRIORITY ACTION Support research and deployment of digitalhealth technologies in cardiovasculardisease prevention and managementResearchers have found that within five yearsof a cancer diagnosis, the risk of heart failurewas three times higher in people treated forbreast cancer or lymphoma than in peoplewithout cancer. Equally, an increased incidenceof cancer in patients with heart failure hasbeen identified, with some studies estimatingthis incidence to be in the range of 19–33% per1 000 person-years.We believe it is of great importance to conductresearch in the area of CVD and cancer comorbidities and complications, as we witnessan increasing number of patients with bothdiseases or recovering completely fromcancer but ending up dying or suffering fromcardiovascular disease as a result of theircancer treatment.RECOMMENDED EUPRIORITY ACTION Include a focus on cancer and CVD comorbidities and research on the shortterm and long-term cardiovascular effectsof cancer treatment in the new Europe’sBeating Cancer Plan and Cancer Missionwithin Horizon EuropeA blueprint for EU action 9
3 Better patient care throughimproved diagnosis, treatmentand managementIt is essential to enable people who are at highrisk of developing CVD, or who have alreadycontracted CVD, to actively manage theircondition, so that they can live to an old agewith a good quality of life.EU Member States are responsible fororganising, funding and providing healthcare to their people. EU policymakers canpromote coordination, share best practiceand guidelines, as well as carry out nonbinding initiatives.Targeted high-quality, risk-assessmentprogrammes may help identify people atrisk and determine the most appropriatepreventive measures. In deprived communities,the rate of high-risk individuals is known to besignificantly higher than in other areas. It istherefore critical to develop approaches thatenable the inclusion of hard-to-reach groups.RECOMMENDED EUPRIORITY ACTION Establish a joint action/network ofMember States, supported by experts,to identify the most effective policiesand measures for reaching out to andmanaging individuals at high risk ofdeveloping CVD3.1 Identification of people at high risk ofdeveloping CVDAround 20–40% of heart attacks occur inpeople previously undiagnosed with CVD.In order to assist these people to reducetheir risks, and to avoid the onset of disease,it is crucial to identify them and providethem with the appropriate advice andpreventative treatment.COSTS OFOF CVDCOSTSCVD(EU)(EU) 111 BILLIONHealthcare costs26 % 54 BILLION 210BILLION21 % 45 BILLIONInformal care costs10 Fighting cardiovascular diseaseper year53 %3.2 Improving treatmentSubstantial differences exist betweencountries in terms of access to technologiesand procedures for treating patients withcardiovascular disease. While access toinnovative treatments correlates with healthexpenditure per capita in a country, budgetallocation explains only some of the variationin provision.High standards for the evaluation andmonitoring of health technologies along theirwhole life-cycle – from market authorisation topost-marketing surveillance – are an essentialelement of ensuring that safe, effective andinnovative technologies are available topatients in a timely manner.
The EU must ensure adequate capacity fora fully operational regulatory system forpharmaceuticals and medical devices alike.Cooperation in Health Technology Assessment(HTA) at EU level is equally important forreducing inequalities in CVD treatment andwasteful spending, allowing decision-makers totake informed decisions based on the clinicaleffectiveness of technologies. In this respect,patients and health care professionals must beinvolved in regulatory processes so that theymay meaningfully contribute to a safe, effectiveand equitable system.RECOMMENDED EUPRIORITY ACTIONS Ensure the necessary human and financialresources are available to the EuropeanCommission services responsible for theimplementation of the Medical DevicesRegulation Secure a positive outcome for the EUlegislative proposal on Health TechnologyAssessment, covering the assessment ofboth medicines and medical devices3.3 Cardiac and stroke rehabilitation andsecondary preventionA crucial part of treatment for CVD isrehabilitation after an event, includingcounselling, medical treatment, exercise andpsychological support. These programmes helpprevent recurrence, and improve functionalcapacity, recovery and psychological wellbeing. They help patients regain as normal alife as possible, optimise their quality of life,and reduce the burden on health services byreducing hospital re-admissions.Although the considerable benefits of cardiacand stroke rehabilitation for patients as well asthe wider society are well-documented, accessto and uptake of quality rehabilitation is patchyin most European countries and is consideredan underutilised resource.RECOMMENDED EUPRIORITY ACTIONS Adopt a European definition of cardiac andstroke rehabilitation Establish a joint action/network ofMember States to identify barriers foruptake of cardiac and stroke rehabilitationand secondary prevention programmesand how to address themA blueprint for EU action 11
Conclusions and recommendationsDeath rates from CVD have fallen steadily over the past half century. Thishas been due to successful interventions, including population-basedprevention and improved treatment options. Nonetheless, CVD remainsthe most common cause of death in the EU, claiming more than 1.8million lives each year. Recent data estimate that more than 60 millionpeople in the EU live with CVD.Recent trends show a slowdown in the rate of decline in CVD death rates– a trend which is more pronounced in younger age groups. These trendsare alarming and suggest that if the status quo prevails, there could be anincrease in deaths from CVD over and above what would be expected froma growing and ageing population. Moreover, there is evidence from EUcountries for an increase in the determinants of CVD, including diabetes andobesity. Should this trend continue, then the latent effects would set thescene for a tremendous setback in CVD morbidity and mortality.We must not be complacent: fighting CVD is far from over, and action atEU level is urgently needed. This CVD Action Plan provides a blueprint forthe 2019–24 EU mandate.OVERALL AIMReduce premature disease and death from CVD andinequalities in cardiovascular death rates in the EUOVERARCHING RECOMMENDATIONEnsure that TFEU Article 168 is properly operationalised,by establishing a world-class health impact assessmentmethodology that considers potential impact on CVD aswell as differential impact in regions (East/West) of the EUby 202412 Fighting cardiovascular disease
Specific priority recommendationsto be achieved by 2024 Set nutrient profiles to underpin nutrition andhealth claims as required by the EC regulation onnutrition and health claims (EC) No 1924/2006 Adopt rules on simplified front-of-pack nutritional labelling Adopt regulations restricting all marketing to children,including digital, of food and drinks high in fat, salt and sugar Raise minimum tobacco excise duties to the highest possible level Bring excise duties on “roll your own” tobacco upto the same level as manufactured cigarettes Strengthen regulation on e-cigarettes Encourage the development and approval of EU fundedprojects (in particular projects supported by EU StructuralFunds) that have a positive impact on active living Raise minimum excise duties on alcoholicbeverages to the highest possible level Introduce mandatory, front-of-pack energy labelling on alcohol Introduce mandatory ingredients list on alcoholic beverages Revise the ambient air quality directive adopting theWHO Air Quality Guideline values as limit values Recognise key areas of CVD research as prioritiesin the Horizon Europe programmeA blueprint for EU action 13
Promote and support the development of harmonisedand comprehensive continuous patient registries in CVD,as well as the digital capability to enable the evidencegenerated within health systems to improve the speedand efficiency of randomised controlled trials Establish a structured collaboration between academic clinicaltrialists, patients, regulators and industry to modernise theInternational Council of Harmonisation (ICH) Good ClinicalPractice (GCP) standards and make them fit for the digital era Support research and deployment of digital health technologiesin cardiovascular disease prevention and management Include a focus on cancer and CVD co-morbidities andresearch on the short-term and long-term cardiovasculareffects of cancer treatment in the new Europe’s BeatingCancer Plan and Cancer Mission within Horizon Europe Establish a joint action/network of Member States,supported by experts, to identify the most effectivepolicies and measures for reaching out to and managingindividuals at high risk of developing CVD Ensure the necessary human and financial resources areavailable to the European Commission services responsiblefor the implementation of the Medical Devices Regulation Secure a positive outcome for the EU legislative proposalon Health Technology Assessment, covering theassessment of both medicines and medical devices Adopt a European definition of cardiac and stroke rehabilitation Establish a joint action/network of Member States to identifybarriers to uptake of cardiac and stroke rehabilitation andsecondary prevention programmes, and how to address them14 Fighting cardiovascular disease
This blueprint has been developed by:The European Heart Network and the European Society of Cardiology.About the EHNAbout the ESCThe European Heart Network (EHN) is aBrussels-based alliance of foundations andassociations dedicated to fighting heartdisease and stroke and supporting patientsthroughout Europe.The European Society of Cardiology (ESC)brings together health care professionals frommore than 150 countries, working to advancecardiovascular medicine and help people leadlonger, healthier lives.www.escardio.orgThe EHN plays a leading role in the preventionand reduction of cardiovascular diseases, inparticular heart disease and stroke, throughadvocacy, networking, capacity-building,patient support, and research so that theyare no longer a major cause of prematuredeath and disability throughout Europe.www.ehnheart.orgA blueprint for EU action 15
Appendix 1What is CVD?CVD affects men and women of all ages, in allEU countries. CVD has many forms, all relatedto the heart and the circulatory system.They include: Ischaemic heart disease (IHD), also knownas coronary artery disease (CAD), whichis caused by atherosclerosis in which fattyplaque deposits cause a narrowing of theartery walls leading the heart to reduceblood flow, the primary cause of heartattacks. Chronic stable angina is chest painthat occurs when the heart is working hardand needs more oxygen. It is often due tophysical exertion and indicates damagedheart function. Stroke, which occurs when an artery thatcarries oxygen and nutrients to the brainis affected by atherosclerosis, blocked by aclot, or bursts. Peripheral artery disease, in whichnarrowed arteries reduce blood flow to thelimbs. Common in diabetes, and the majorcause of lower limb amputations. Heart rhythm disturbances: suddencardiac death is often the first and finalpresentation of other underlying CVD andis of ongoing concern in most patients withCVD. Atrial fibrillation (AF or AFIB) is anarrhythmia with irregular heart rate thatmay cause stroke, heart failure, palpitations,fatigue and shortness of breath.16 Fighting cardiovascular disease Heart failure (HF) occurs when damageto the heart muscle is severe enoughto prevent it from functioning properly;morbidity and mortality in severe heartfailure is worse than in many cancers andthe only current cure is transplantation. Congenital heart disease is a general termfor a range of birth defects that affect thenormal way the heart works. The term“congenital” means the condition is presentfrom birth. Congenital heart disease is oneof the most common types of birth defect,affecting up to 8 in every 1,000 babies bornin Europe. Inherited heart conditions, also knownas genetic heart conditions, as theyare passed on through families. Theycan affect people of any age and can belife-threatening. If left undetected anduntreated, an inherited heart condition maylead to heart failure or even sudden deathfrom cardiac arrest. For many families,the first sign there is a problem is whensomeone dies suddenly with no obviouscause or explanation. Vascular dementia, in which mentalproblems such as confusion, slow thought,memory issues, mood and personalitychanges occur in combination with reducedblood flow to the brain; it is increasing inincidence with the ageing population. Valvular heart disease, of which aorticstenosis and mitral valve insufficiency arethe most frequent.
Appendix 2What are CVD risk factors?Risk factors associated with cardiovascular disease can be divided into different categories:Biological determinantsLifestyle determinantsElevated blood pressureUnhealthy dietRaised blood sugarTobacco useElevated blood cholesterolPhysical inactivityOverweight/obesityAlcohol abuseBroader neticsLiving conditions (including air pollution)EthnicityWorkin
This paper provides a blueprint for addressing the huge burden of CVD among the EU population, by putting forward specific recommendations for an ambitious EU action plan that addresses cardiovascular health to be implemented in the current EU mandate. We call on EU policymak