Transcription
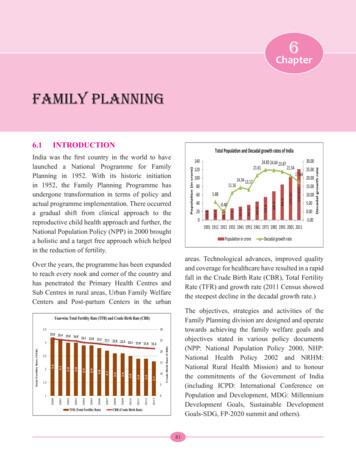
6ChapterFamily Planning6.1INTRODUCTIONIndia was the first country in the world to havelaunched a National Programme for FamilyPlanning in 1952. With its historic initiationin 1952, the Family Planning Programme hasundergone transformation in terms of policy andactual programme implementation. There occurreda gradual shift from clinical approach to thereproductive child health approach and further, theNational Population Policy (NPP) in 2000 broughta holistic and a target free approach which helpedin the reduction of fertility.areas. Technological advances, improved qualityand coverage for healthcare have resulted in a rapidfall in the Crude Birth Rate (CBR), Total FertilityRate (TFR) and growth rate (2011 Census showedthe steepest decline in the decadal growth rate.)Over the years, the programme has been expandedto reach every nook and corner of the country andhas penetrated the Primary Health Centres andSub Centres in rural areas, Urban Family WelfareCenters and Post-partum Centers in the urbanThe objectives, strategies and activities of theFamily Planning division are designed and operatetowards achieving the family welfare goals andobjectives stated in various policy documents(NPP: National Population Policy 2000, NHP:National Health Policy 2002 and NRHM:National Rural Health Mission) and to honourthe commitments of the Government of India(including ICPD: International Conference onPopulation and Development, MDG: MillenniumDevelopment Goals, Sustainable DevelopmentGoals-SDG, FP-2020 summit and others).81
Annual Report 2015-161. Some facts on Family Planning and related mattersExpected increase of population of 15.7% in 15 years From 1210 million in 2011 to 1400 million in 2026Decline in TFR Helps to stabilize India’s population growth which in turn spursthe economic and social progressGreater investments in familyplanning Helps to mitigate the impact of high population growth byhelping women achieve desired family size and avoid unintendedand mistimed pregnancies Reduce maternal mortality by 35% Reduce infant mortality and abortions significantly Maternal Mortality Ratio (MMR) to 100/100,000Govt. of India’s commitmentby 2017 Infant Mortality Rate (IMR) to 30/1000 live birthsTotal Fertility Rate (TFR) to 2.12. Factors that influence population growthUnmet need of Family Planning 21.3% as per DLHS-III (2007-08)Age at Marriage and firstchildbirth 22.1% of the girls get married below the age of 18 years Out of the total deliveries 5.6% are among teenagers i.e. 15-19yearsSpacing between Births Spacing between two childbirths is less than the recommendedperiod of 3 years in 59.3% of births (SRS 2013)15-25 age group(women) 52.5% contribution in total fertility 46% contribution in maternal mortality3. Current demographic scenario in the country (Census 2011)2.4% of world’s land mass 17.5% of the world’s population1.21 billion India’s population as per Census-2011200 million Population of Uttar Pradesh – more than the population of BrazilGrowth of Population in IndiaCensus Year19711981199120012011Population (in crores) Decadal Growth 17.6482Average AnnualExponential Growth (%)2.202.222.161.971.64
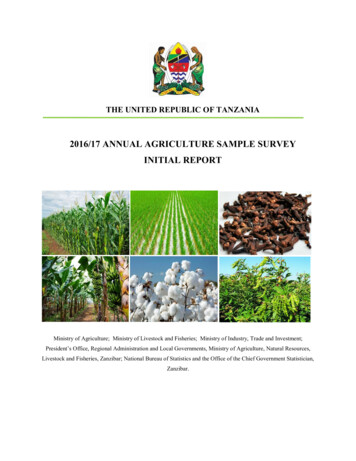
Annual Report 2015-16Perceptible decline (in last 5decades) Population added Significant decline 4. Progress in TFRTFR decline TFR of 2.1 or lessTFR 2.1-3.0 TFR above 3.0 Crude Birth Rate – 40.8 per 1000 in 1951 to 21.4 in 2013.Infant Mortality Rate – from 146 in 1951-61 to 40 in 2013.Total Fertility Rate – from 6.0 in 1951 to 2.3 in 2013.(Ref: Appendix-I)Steepest decline in growth rate between 2001 and 2011 from21.54% to 17.64%.Decline in 0-6 population by 3.08% compared to 2001Lesser than the previous decade, 18.14 crores added during2001-2011 compared to 18.23 crores during 1991-2011.There is a 4.1 percentage point fall from 24.99% in 2001 to20.92% in 2011 in the growth rate of population in the EAGStates (Uttar Pradesh, Bihar, Jharkhand, Madhya Pradesh,Chhattisgarh, Rajasthan, Odisha and Uttarakhand) after decadesof stagnation.From 2.9 in 2005 to 2.3 in 2013Decline more significant in High Focus States24 States and Union Territories10 States–Haryana-2.2, Gujarat-2.3, Arunachal Pradesh-2.3,Assam-2.3, Chhattisgarh-2.7, Jharkhand-2.6, Rajasthan-2.8,Madhya Pradesh-2.9, Meghalaya-2.9 and Dadara& NagarHaveli-2.92 States– Bihar-3.4, Uttar Pradesh-3.1In six very high focus States, Uttar Pradesh hasshown a decline of 0.2 points (between 2012 &2013). Among high focus states, Jharkhand hasshown a decline of 0.2 points. Madhya Pradesh,Chhattisgarh and Gujarat have not shown anydecline whereas Rajasthan, Assam and Haryanahas shown a decline of 0.1 points.6.1.1 Impact of High Focus Approach of theGovernment of India (GoI)Government of India has categorized States as perthe TFR level in very high-focus (more than orequal to 3.0), high-focus (more than 2.1 and lessthan 3.0) and non-high focus (less than or equalto 2.1).CategoryVery High Focus States for FPHigh Focus States for FPStateBiharUttar PradeshMadhya aryanaOdishaSRS-2011 SRS-2012 SRS-2013 Point 32.30.02.32.32.2-0.12.22.12.10.083
Annual Report 2015-166.2married women (aged 15-49 years) was 56.3% inNFHS-3 (an increase of 8.1 percentage points fromNFHS-2) while corresponding increase betweenDLHS-2 & 3 is relatively lesser (from 52.5% to54.0%). The proximate determinants of fertilitylike, age at marriage and age at first childbirth(which are societal preferences) are also showinggood improvement at the national level.FAMILY PLANNING SCENARIO(NHFS, DLHS AND AHS)The last survey figures available are from NFHS3 (2005-06) and DLHS-3 (2007-08), which arebeing used for describing current family planningsituation in India. Nation-wide, the small familynorm is widely accepted (the wanted fertilityrate for India as a whole is 1.9 (NFHS-3) andAHS survey has been conducted in 9 States (8EAG States Assam) which indicates that:the general awareness of contraception is almostuniversal (98% among women and 98.6% amongmen: NFHS-3). Both NFHS and DLHS surveysshowed that contraceptive use is generally rising(see adjoining figure). Contraceptive use among Contraceptive use has been static in almostall AHS States except Bihar which has showna decrease in use of modern contraceptives.Rajasthan and Chhattisgarh have shown asubstantial increase in modern contraceptiveusage. The unmet need has declined in all statesexcept Madhya Pradesh where it hasremained static.6.2.1 District wise contraceptive prevalence The graph given below shows the districtswith the highest contraceptive prevalence:State-wise TFR, Modern contraceptive prevalence & Unmet Need for High Focus StatesS. N.StatesTFRmCPR (%)Unmet Need ajasthan3.23.12.958.859.462.419.612.613.07Madhya Pradesh3.13.13.057.059.359.422.421.621.68Uttar .63.533.938.236.539.233.531.584
Annual Report 2015-16method (emergency contraceptive pill) to be usedin cases of emergency.District-wise modern Contraceptive PrevalenceRate6.3.1.a. Spacing Methods:- These are thereversible methods of contraception tobe used by couples who wish to havechildren in future. These include:6.3A.Oral Contraceptive Pills (OCPs) These are hormonal pills which have to betaken by a woman, preferably at a fixedtime, daily. The strip also contains additionalplacebo/iron pills to be consumed during thehormonal pill free days. The method may beused by majority of women after screeningby a trained provider. At present, there is a scheme for deliveryof OCPs at the doorstep of beneficiaries byASHA with a minimal charge. The brand“MALA-N” is available free of cost at allpublic healthcare facilities.B.Condoms These are the barrier methods ofcontraception which offer the dual protectionof preventing unwanted pregnancies aswell as transmission of ReproductiveTransmitted Infection/Sexually TransmittedInfection (RTI/STI) including HIV. Thebrand “Nirodh” is available free of cost atgovernment health facilities and suppliedat the doorstep by the ASHAs for minimalcost.C.Intra-Uterine(IUCD) Copper containing IUCDs are a highlyeffective method for long term birth spacing. Should not be used by women with uterineanomalies or women with active PID orthose who are at increased risk of STI/RTI(women with multiple partners).CURRENT FAMILY PLANNINGEFFORTSFamily planning has undergone a paradigm shiftand emerged as one of the interventions to reducematernal and infant mortalities and morbidities.It is well-established that the states with highcontraceptive prevalence rate have lower maternaland infant mortalities.Greater investments in family planning can thushelp mitigate the impact of high population growthby helping women achieve the desired family sizeand avoid unintended and mistimed pregnancies.Further, contraceptive use can prevent recourseto induced abortion and eliminate most of thesedeaths. Studies show that if the current unmetneed for family planning could be fulfilled overthe next 5 years, we can avert 35,000 maternaldeaths, 1.2 million infant death, save more thanRs. 4450 crores and saveRs. 6500 crores, if safeabortion services are coupled with increasedfamily planning services. This strategic direction isthe guiding principle in implementation of familyplanning programme in future.6.3.1 Contraceptive services under theNational Family Welfare ProgrammeThe methods available currently in India maybe broadly divided into two categories, spacingmethods and permanent methods. There is another85ContraceptiveDevices
Annual Report 2015-16 The acceptor needs to return for followup visit after 1, 3 and 6 months of IUCDinsertion as the expulsion rate is highest inthis duration. Two types:heat or electricity (cautery). The procedureis performed by MBBS doctors trained inthese. However, the couple needs to use analternative method of contraception for firstthree months after sterilization till no spermsare detected in semen.o Cu IUCD 380A (10 yrs) o Cu IUCD 375 (5 yrs) o ConventionalNew approach of method delivery- postpartum IUCD insertion by specially trainedproviders to tap the opportunities offered byinstitutional deliveries.o Non- Scalpel Vasectomy – no incision,only puncture and hence no stitches6.3.1.c. Emergency Contraceptive Pill (ECP)6.3.1.b. Permanent Methods:- These methodsmay be adopted by any member of thecouple and are generally consideredirreversible.A.Female Sterilisation Two techniques:o Minilap: Minilaparotomy involvesmaking a small incision in the abdomen.The fallopian tubes are brought to theincision to be cut or blocked. Can beperformed by a trained MBBS doctor.Male Sterilisation Through a puncture or small incision inthe scrotum, the provider locates each ofthe 2 tubes that carries sperm to the penis(vas deferens) and cuts or blocks it bycutting and tying it closed or by applying To be consumed in cases of emergencyarising out of unplanned/unprotectedintercourse and The pill should be consumed within 72hours of the sexual act and should neverbe considered a replacement for a regularcontraceptive.6.3.1.d. Other Commodities - Pregnancy TestingKits (PTKs)o Laparoscopic: Laparoscopy involvesinserting a long thin tube with a lensin it into the abdomen through a smallincision. This laparoscope enables thedoctor to see and block or cut the fallopiantubes in the abdomen. Can be done onlyby trained and certified MBBS doctor orspecialist.B.Two techniques being used in India: Helps to detect pregnancy as early as oneweek after the missed period, thus providingan early opportunity for medical terminationof pregnancy, thus saving lives lost to unsafeabortions and These are available at the sub-centre leveland also carried by ASHA.6.3.1.e. Service Delivery Points 86All the spacing methods, viz. IUCDs,Oral Contraceptive Pills(OCPs) andCondoms are available at the public healthfacilities beginning from the sub-centrelevel. Additionally, OCPs Condoms andEmergency Contraceptive Pills (since arenot skill based services) are available at thevillage level also through trained ASHAsand
Annual Report 2015-16 Permanent methods are generally availableat primary health centre level or above.They are provided by MBBS doctors whohave been trained to provide these services.Laparoscopic sterilization is being offeredFamily Planning MethodSpacing MethodsIUD 380 A/IUCD 375Oral Contraceptive Pills (OCPs)Sub-centre & higher levelsCondomsSub-centre & higher levelsLimiting MethodsMinilapLaparoscopic SterilizationNSV: No Scalpel Vasectomyat CHCs and above level by a specialistgynaecologist/surgeon only.These services are provided to around 20crores eligible couples. Details of servicesprovided at different level of:Service ProviderService LocationTrained & certified ANMs, LHVs, SNs Sub-centre & higher levelsand doctorsTrained ASHAs, ANMs, LHVs, SNs Village leveland doctorsTrained ASHAs, ANMs, LHVs, SNs Village leveland doctorsTrained & certified MBBS doctors &specialist doctorsTrained & certified MBBS doctors &specialist doctorsTrained & certified MBBS doctors &specialist doctorsPHC & higher levelsUsually CHC & higherlevelsPHC & higher levelsEmergency ContraceptionEmergency Contraceptive Pills Trained ASHAs, ANMs, LHVs, SNs Village level, Sub-centre &(ECPs)and doctorshigher levelsNote: Contraceptives like OCPs, Condoms are also provided through Social Marketing Organizationsassociated with less failure and complicationrates.6.3.2 The Salient features of the FamilyPlanning ProgrammeA.On-going interventions: More emphasis on spacing methods likeIUCD. Availability of Fixed Day Static Services atall facilities. Emphasis on minilaptubectomy servicesbecause of its logistical simplicity and87 A rational human resource development planis in place for provision of IUCD, minilapand NSV to empower the facilities (DH,CHC, PHC, SHC) with at least one providereach for each of the services and Sub Centreswith ANMs trained in IUD insertion. Ensuring quality care in Family Planningservices by establishing Quality Assurance
Annual Report 2015-16Committees at State and district levels. Accreditation of more private/NGO facilitiesto increase the provider base for familyplanning services under PPP. Increasing male participation and promotingNon- Scalpel Vasectomy. Compensation scheme for sterilizationacceptors, under the scheme, Ministryof Health & Family Welfare providescompensation for loss of wages to thebeneficiary and also to the service provider(& team) for conducting sterilizations. Thecompensation scheme has been enhanced in11 high focus States from the year 2014. for placement of dedicated family planningcounsellors and training of personnel.‘National Family Planning IndemnityScheme’ under which clients are indemnifiedin the eventualities of deaths, complicationsand failures following sterilization. Theproviders/ accredited institutions areindemnified against litigations in thoseeventualities. Post-Partum Intra-Uterine ContraceptiveDevices(PPIUCD) Incentive for serviceproviders and ASHAs. Ministry of Health & Family Welfarehas introduced short term IUCD (5 yearseffectivity), Cu IUCD 375 under theNational Family Planning Programme.Training of State level trainers has alreadybeen completed and process is underway totrain service providers up to the sub-centerlevel. A new method of IUCD insertion (postpartum IUCD insertion) has been introducedby the Government. Promoting post-partum family planningservices at district hospitals by providingB.Home Delivery of Contraceptives (HDC) A new scheme was launched to utilize theservices of ASHA to deliver contraceptivesat the doorstep of beneficiaries. The schemewas launched in 233 pilot districts of 17States on 11 July 2011 and later expandedto the entire country from 17th December2012. ASHA is charging a nominal amountfrom beneficiaries for her effort to delivercontraceptives at doorstep i.e. Re. 1 fora pack of 3 condoms, Re. 1 for a cycle ofOCPs and Rs. 2 for a pack of one tablet ofECP.C.Ensuring Spacing at Birth (ESB) Under a new scheme launched by theGovernment of India, services of ASHAsto be utilised for counselling newly marriedcouples to ensure spacing of 2 years aftermarriage and couples with 1 child to havespacing of 3 years after the birth of 1st child.The scheme is operational in 18 States (EAG,North Eastern and Gujarat and Haryana).ASHA would be paid following incentivesunder the scheme:o Rs. 500/- to ASHA for delaying first childbirth by 2 years after marriage;o Rs. 500/- to ASHA for ensuring spacingof 3 years after the birth of 1st child ando Rs. 1000/- in case the couple opts fora permanent limiting method up to 2children only.88D.Pregnancy Testing Kits (PTKs) Nishchay: Home based Pregnancy Test
Annual Report 2015-16Kits (PTKs) was launched under NRHM in2008 across the country and was anchoredwith the Family Planning Division on 24thJanuary, 2012. The PTKs are being made available at subcenters and to the ASHAs. The PTKs facilitate the early detectionand decision making for the outcomes ent up to peripheral facilities.F.Demand generation activities in the formof display of posters, billboards and otheraudio and video materials in the variousfacilities.G.Strong political will and advocacy at thehighest level, especially in states with highfertility rates.H.New interventions to improve access tocontraception Expansion of basket of choicethrough promotion of post-partum familyplanning (esp. through Minilap) and NSV:The detailed programme specificationswas shared with States in August 2015-16.Handholding of the States is being done forimproving the static centers for post- partumfamily planning and NSV.6.3.3 Progress made under Family PlanningProgrammeService Delivery 2014-15: The performance offamily planning services (in lakhs) during 2014-15is provided below (source: HMIS):o Injectable Depot MedroxyprogesteroneAcetate (DMPA): The Drugs TechnicalAdvisory Board (DTAB) agreed tothe introduction of the injectablecontraceptive DMPA in the publichealth system under the National FamilyPlanning Programme.o POP: Under piloting processo Centchroman: Under programming Improved Contraceptive Packaging: Thepackaging for Condoms, OCP and ECP isnow being improved so as to influence thedemand for these commodities. Number of IUCDs and sterilisations hasremained static in spite of declining CBR andTFR. There is a need to sustain momentumto reach the replacement level fertility. Considering the current efforts to focuson spacing, it is expected that IUCDperformance would increase in near future. State wise sterilisation and IUCDachievements is provided at Appendix-2.6.3.4 Promotion of IUCDs as a short and longterm spacing methodIn 2006, Government of India (GoI) launched“Repositioning IUCD in National Family WelfareProgramme” with an objective to improve thePlanning for improved service delivery89
Annual Report 2015-16health facilities after undergoing stipulatedtraining.mixed method in contraceptive services and hasadopted diverse strategies including advocacy ofIUCD at various levels; community mobilizationfor IUCD; capacity building of public healthsystem staff starting from ANMs to providequality IUCD services and intensive IEC activitiesto dispel myths about IUCD. Currently, increasedemphasis is given to promotion of IUCD insertionas a key spacing method under Family Planningprogramme.Onsite training for IUCD services“Alternative Training Methodology in IUCD”using anatomical, simulator pelvic models,incorporating adult learning principles andhumanistic training technique was started inSeptember 2007 to train service providers inprovision of quality IUCD services. Jhpiego, Engender Health and IPAS havebeen engaged for onsite training for IUCDservices. To track the progress of training and forbetter post training follow up, an IUCDtracking software has been designed and isoperational now.6.3.5 Emphasis on PostpartumPlanning (PPFP) services In order to capitalize on the ies, the Government of India isfocusing on strengthening post-partum FPservices; PPFP services are not being offereduniformly at all levels of health systemacross different States of India resulting inmissed opportunities; Insertion of IUCD during the post-partumperiod, known as Post-partum Intra-uterineContraceptive Device (PPIUCD), is beingfocused to address the high unmet need ofspacing during post-partum period.Actions taken and achievements Hindustan Latex Family Planning PromotionTrust (HLFPPT) has been engaged to supportstates to conduct interval IUCD trainingand also post training follow-up of trainedpersonnel. HLFPPT would also follow-upsample cases of IUCD insertion to ensureretention; Directive has been issued to the states tonotify fixed days/ per week at SHC and PHClevel for conducting IUCD insertions and Introduction of Cu-IUCD-375 (5 yearseffectivity) under the Family PlanningProgramme.Actions taken and achievements Increasing provider base for IUCD (throughAYUSH practitioners) FamilyStrengthening Post-Partum IUCD (PPIUCD)services at high case load facilities:o Currently the focus is on placement oftrained providers for PPIUCD insertionat district and sub-district hospital levelonly, considering the high institutionaldelivery load at these facilities.It has been approved to train AYUSH doctorsin IUCD after a short refresher course/training and AYUSH doctors except Yogaand Naturopathy practitioners are allowedto perform IUCD insertions at public90
Annual Report 2015-16have been approved across the country (asper the state projections) in financial year2014-15. Of these, 959 positions are filledand counselors are in place.Graph 6: Top 10 performing states as per totalPPIUCD insertions6.3.6 Assured delivery of family planningservices6.3.6.a. Fixed Day Services (FDS) for IUCDinsertion: States are facilitated to ensurefixed days IUCD insertion services atthe level of SC and PHC (at least 2 daysin a week). 6.3.6.b. Fixed Day Static Servicessterilisation at facility level:Total 10,34,894 PPIUCDs have beeninserted all across the country since theinitiation of the PPIUCD programme.Approximately 5,90,217 PPIUCD insertionshave taken place in 2014-15 as againstaround 3,24,487 in 2013-14. Operationalization of FDS has followingobjectives: To make a conscious shift from campapproach to regular routine services;Appointing dedicated counsellors at highcase load facilities: To make health facilities self-sufficient inprovision of sterilization services ando RMNCH A counsellors are beingappointed at all high case load facilities toprovide counselling services in followingareas: To enable clients to avail sterilizationservices on any given day at theirdesignated health facility.FDS Guidelines for Sterilization Services Post-partum Family Planning (IUCD andSterilisation);Health FacilityMinimum Frequency Other family planning methods such ascondoms, pills etc.;District HospitalTwice a weekSub District HospitalWeeklyCHC / Block PHCFortnightly24 7 PHC / PHCMonthly Ensuring healthy timing and spacing ofpregnancy; Mother & baby care;Note: Those facilities providing more frequent servicesalready must continue to do so. Early initiation of breast feeding;6.3.6.c. Camp approach for sterilizationservices is continued in those stateswhere operation of regular fixed daystatic services in sterilization takeslonger time. Immunization and Child nutrition. inThe posts of 1633 RMNCH A counselors91
Annual Report 2015-166.3.6.d. Rational placement of trainedproviders at the peripheral facilities forprovision of regular family planningservices.However, it is important to note thatmajority of laparoscopic sterilisation(45.8%) is conducted at CHC level.27.1% of cases were operated at SDH/DHlevel and 0.5% at State owned institutesandActions taken and achievements: In year 2014-15, all the States have showntheir commitment to strengthen fixed dayfamily planning services for both IUCDand sterilisation and it has been includedunder quarterly review mechanism to assessprogress made by the States. Recent field visits and review missions tothe States reveal that most of the facilitiesat the level of CHC and above have beenoperationalised for providing FP services onfixed day basis. o As anticipated around 67.2% of thePPS is reported at DH/ SDH level sincemajority of institutional deliveries areconducted at these facilities; however,this needs to increase at PHC (12.7%)and CHC (17.6%) level as well.6.3.7 Quality assurance in Family PlanningQuality assurance in family planning services isthe decisive factor in acceptance and continuationof contraceptive methods and services. TheHon’ble Supreme Court of India in its Order dated1.3.2005 in Civil Writ Petition No. 209/2003(Ramakant Rai V/s Union of India) has, interalia, directed the Union of India and States/UTsfor ensuring enforcement of Union Government’sGuidelines for conducting sterilization proceduresand norms for bringing out uniformity with regardto sterilization procedures by:Analysis of the data available from HMISfor 2014-15 reveals that:o Around 36.3% of NSVs are conductedat PHC, 33.2% at CHC level, 29.2% atSDH/DH level and 1.2% at State ownedinstitutes;o Majority of minilap sterilisations (45.4%)are conducted at PHC level followedby 31.5% at CHC level. 22.9% of theminilap were conducted at SDH/DHlevel and 0.2% at State owned institutes;o 26.6% laparoscopic sterilisation isconducted at PHCs via camp mode.92 Creation of panel of doctors/health facilitiesfor conducting sterilization procedures andlaying down of criteria for empanelmentof doctors for conducting sterilizationprocedures; Laying down of checklist to be followed byevery doctor before carrying out sterilizationprocedure; Laying down of uniform proforma forobtaining the consent of person undergoingsterilization; Setting up of Quality Assurance Committeefor ensuring enforcement of pre and postoperative guidelines regarding sterilizationprocedures and
Annual Report 2015-16 Bringing into effect an insurance policyuniformly in all States for acceptors ofsterilizations etc.For the acceptors of Sterilization fortreatment of post-operative complications,failure or death attributable to the procedureof sterilization. The manual has been revisedin 2013.The division came up with the‘India’s Vision FP 2020’ document whichmanifests the efforts taken by our countryin turning the global FP 2020 commitmentinto reality. Ministry of Health and FamilyWelfare, Family Planning Division hasrecruited technical experts to support statesin improving delivery of quality servicesActions taken and achievementsRevision of FP manuals and Guidelines: TheMinistry of Health & Family Welfare has revisedand updated the standards/manuals/ guidelines anddirected the states to adhere to the same to ensurequality of service provision. FP manuals andguidelines have been widely disseminated and canbe freely accessed at the NHM website. Standards and Quality Assurance inSterilization Services: A comprehensivemanual on ‘Standards and Quality Assurancein Sterilization Services’ which is anamalgamation of four existing manuals (i.e.Standards for Female and Male sterilization2006; Quality Assurance Manual forSterilization Manual- 2006; Standardoperating procedure for sterilization servicesin camps- 2008; Operational Guidelinesfor FDS approach for Sterilization services-2008) was released in November 2014. Themanual not only includes the contents ofthe four manuals but also newer inclusionsbased on field experiences. The ‘Reference Manual for FemaleSterilization’ has been prepared and releasedin November 2014 which is a combination oftwo existing manuals, i.e. Reference Manualfor MinilapTubectomy- 2009; Guidelinesfor Training in Female Sterilization forProgramme Officers, Training Coordinatorsand Trainers- 2010. IUCD Reference Manual for MedicalofficersandNursingpersonnel:Comprehensive manual for the intervalIUCD and PPIUCD insertion.IUCDreference manual for AYUSH, Referencemanual on male sterilization and Manual onFamily Planning Indemnity Scheme.Manual for RMNCH A Counsellors6.3.8 State Quality WorkshopsTo orient the States and services providers ontechnical standards, an orientation workshop forupdated guidelines has been conducted in all thestates by FP division technical experts and coregroup members.6.3.9 Other promotional schemes6.3.9.a. Compensation scheme for acceptors ofsterilization: Government has been implementinga Centrally Sponsored Scheme (CSS) since 1981 tocompensate the acceptors of sterilization for the lossof wages for the day on which he/she attended themedical facility for undergoing sterilization. Thiscompensation scheme for acceptors of sterilizationservices was revised with effect from 31.10.2006and has been further improved with effect from07.09.2007.In the light of the rise in cost of living,the ever increasing transport cost which enablesa client to travel from his residence/village to thenearest service centre, the prevalent high wagecompensation for the days requiring recuperationas well as other incidental cost, Government ofIndia has approved an enhancement in the currentcompensation package for the 11 high focusStates- Uttar Pradesh (UP), Bihar (BH), MadhyaPradesh (MP), Rajasthan (RJ), Chhattisgarh (CG),Jharkhand (JH), Odisha (OD), Uttarakhand (UK),Assam (AS), Haryana (HR) and Gujarat (GJ).93
Annual Report 2015-166.3.9.b. Compensation scheme in Public Facilities(Amount in Rs.)StatesType of Operation Acceptor ASHA/Health Others TotalWorker2000300400 270011 High Focus States (UP, BH, MP, VasectomyRJ,
Family Planning 6 Chapter 6.1 INTRODUCTION . Age at Marriage and first . equal to 3.0), high-focus (more than 2.1 and less than 3.0) and non-high focus (less than or equal to 2.1). In six very high focus States, Uttar Prad