![HEDIS Made Easy PPT [Read-Only] - 039189f Solhost](/img/19/la-care-hedis-made-easy.jpg)
Transcription
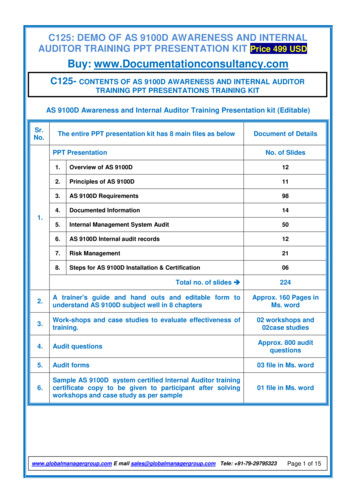
HEDIS Made EasyWhat you really need to knowDisclaimer“This document is merely a tool for providers and provides a general summary on some limited HEDIS Programrequirements. This document should not be used as legal advice or expert advice or comprehensive summary of the HEDIS Program. Please refer to ncqa.org for HEDIS Program measures and guidelines as well as relevant statutes.The information provided is in this document is for 2016 HEDIS period and is current at the time this document was created.NCQA HEDIS Program requirements, applicable laws, and L.A. Care’s policy change from time to time, and information anddocuments requested from you may also change to comply with these requirementsL.A. Care is not affiliated with NCQA or its HEDIS Program and does not receive any financial remuneration from it.”HEDIS is a registered trademark of the National Committee for Quality Assurance (NCQA).HEDIS OPERATIONSHEALTHCARE OUTCOMES & ANALYSIS1
L earning Goals forTod ay HIPAA Learn what HEDIS is What is your role inHEDIS ? Annual HEDIS Calendar Medical Record Requests Hybrid HEDIS Measures Questions & Answers2
O u r“1 ”S im ple Goal HEDIS can beintimidating HEDIS can be nervewracking HEDIS can befrustratingTo m ake H E D IS easierforyou !3
H ow to Reac h Goals Understand theguidelines Follow best practice Establish a habit Continual repetition tillit sticks4
H IP A AUnder the Health InformationPortability and Accountability Act rule: Personal Health Information (PHI)can be collected and shared withthe Health Plan for quality purposes Data collection is permitted No further authorization neededfrom the patient5
W hatis H E D IS ? Healthcare Effectiveness Data and Information Set6
Retrospec tive Review HEDIS is a lookbackwards at the year oryear(s) prior It is a review of theservices and clinicalcare provided to L.A.Care patients.FuturePast7
H E D IS H YB RID D A TAHEDIS hybrid data is a combination of:1 . A d m inistrative d ata: Data captured fromClaims, Encounters, Pharmacy, and Labs2 . M ed ic alRec ord review: A validation audit8
W hatis you rrole in H E D IS ? Ensure preventative healthcarescreening is done Ensure screening is completedwithin the right time frame Ensure all screenings aredocumented in the Medical Record Ensure the date of service, date ofbirth, and member name are legibleand correct Faxing medical records to L.A. Carewithin 5 business days of request9
H E D IS 2 0 1 6 C A L E N D A RJan – May Collection of medicalrecords from Dr. Offices Medical records audited byL.A. CareJune Audit results are compiled Audit results are sent toNCQAJuly - Oct NCQA releases report card NCQA releases newmeasures/changes Training at doctors’ offices Onsite medical record audit10
M ed ic alRec ord Requ estsMedical record requests are sentby fax and include: A patient list The measure(s) we areauditing Explanation of the minimumdocuments needed11
Frequ ently A sked Q u estionsShould I send the entire record?N o, we ask thatyou only provid e whatisneed ed whic h is spec ified on the m ed ic alrequ estformWho do I contact if I have a question about theHEDIS request?E ac h fax requ estsentinc lu d es the c ontac tperson’ s nam e and telephone nu m ber12
Tu rn-A rou nd Tim eDay turn-aroundto faxMedical Recordsto L.A. Care13
H ybrid H E D IS M easu resLine of i-CalMedi-CalMMPMMPAdult HealthABA Adult BMI AssessmentCBP Controlling High Blood PressureCDC Comprehensive Diabetes CareCOL Colorectal Cancer ScreeningMRP Medication Reconciliation Post DischargeOlder Adult HealthCOA Care for the Older AdultsWomen's HealthCCS Cervical Cancer ScreeningFPC Frequency of Prenatal CarePPC Prenatal and Postpartum CareChildren and Adolescent HealthCIS Children Immunization StatusHPV Human Papillomavirus Vaccine for Female AdolescentsIMA Immunizations for AdolescentsWeight Assessment and Counseling for Nutrition andWCC Physical Activity for Children/AdolescentsW34 Well-Child Visits in the 3rd, 4th, 5th & 6th Years of LifeAWC Adolescent Well-Care VisitsMMP – Cal MediConnect/dual eligible; MA – Medicare Advantage; LACC – Commercial/Marketplace;MLTSS – Managed Long Term Services and Support14
H ybrid H E D IS M E A S URE SA D UL T H E A L TH15
Adult BMIAssessment(ABA)Documentation must have: 20 years-of-age and Older: Weightand BMI value. Younger than 20 years-of-age :Height, Weight, and BMI inPercentile.Common Chart Deficiencies:Ages 18-74Documentation in 2014/2015 Height and/or weight are documentedbut there is no calculation of the BMI A range was given or threshold to bemet. Each patient must have a distinctBMI value or %16
ControllingHigh Blood Pressure(CBP)Documentation must have: HTN Diagnosis before June 2015 Last BP reading of 2015 You must have the date and resultA minimum of two notes must besubmitted. 1) HTN Diagnosis 2) BPreadingThe Diagnosis can be from any progressnote, problem list, consult note, hospitaladmission or dischargeAges 18-85Diagnosis of HypertensionBlood Pressure Controlled18-59 140/9060-85 with diabetes 140/9060-85 without diabetes 150/90Common Chart Deficiencies: Elevated BP Check the patient’s BP at thebeginning and the end of the visit anddocument both findings Diagnosis date of hypertension is notclearly documented17
ComprehensiveDiabetes Care(CDC)Documentation must have: Hemoglobin A1cBlood PressureNephropathy: Urine Tests ( ) and (-)now acceptable, ACE/ARB prescription,or visits notes from nephrologists Retinal Eye Exam (2014/2015)Submit the last HbA1c and BP screeningof the year 2015Common Chart Deficiencies:Ages 18-75HbA1c TestingHbA1c ResultsNephrologyRetinal Eye ExamBlood Pressure reading Tests ordered but not doneLab results not foundConsult reports not found BP reading elevated. Take BP reading at thebeginning and end of each visit, anddocument18
Colorectal CancerScreening(COL)Documentation must have:Date and result of one of these screenings: Colonoscopy within ten years (2006 -2015) Sigmoidoscopy within five years (2011-2015) FOBT (in 2015)Any of the three scenarios pass for FOBT1. Guaiac FOBT – 3 samples or note thatdone2. Immunochemical FOBT note that itwas done3. FOBT unknown but documented asdoneCommon Chart Deficiencies:Ages 50-75Screening for Colon Cancer Not documenting Colorectal screenings inthe health history Not providing the health history with thenote and/or test results FOBT test performed in an office setting orperformed during a digital rectal exam donot meet criteria19
Medication ReconciliationPost-Discharge(MRP)Ages 18 Medication reconciliationconducted by a prescribingpractitioner, clinical pharmacist orregistered nurse on date ofdischarge through 30 days afterdischarge (31 days total)Documentation must have:1. Notation that the medicationsprescribed upon discharge werereconciled with the current medicationin the outpatient record -or2. A medication list in a dischargesummary that is present in theoutpatient chart and evidence of areconciliation with the currentmedications -or3. Notation that no medicationswere prescribed upon dischargeAn outpatient visit is not required,only documentation in the outpatientrecord that the medication was reconciledmeets criteria20
H ybrid H E D IS M E A S URE SO L D E R A D UL T H E A L TH21
Care of the OlderAdult(COA)Documentation must have:1. Advance care planningIncludes a discussion about preferences forresuscitation, life sustaining treatment andend of life care. Examples include: Advance directives Actionable medical orders Documentation of care planningdiscussion Living Will2. Medication reviewIncludes at least one (1) medication reviewwith:Ages 66 Advance Care PlanningMedication ReviewFunctional Status AssessmentPain Assessment Presence of a medication list and datethe review was performed or Dated notation that the member is nottaking any medicationReview must be by a prescribingpractitioner and/or pharmacist22
Care of the Older Adult Documentation must have:(COA)3. Functional status assessment(Continued) One (1) functional status assessment andthe date it was performed Notation ADLs were assessed, or Notation that Instrumental Activity ofDaily Living (IADL) were assessed, or Results of assessment using astandardized tool, or Notation that at least 3 of the 4following were assessed: cognitivestatus, ambulation status, hearing,vision and speech, other functionalindependenceThe assessments may be done duringseparate visits4. Pain assessmentDocumentation of pain assessment andthe date it was performed (Positive orNegative findings)23
H ybrid H E D IS M E A S URE SW O M E N ’ S H E A L TH24
Cervical CancerScreening(CCS)Documentation must have: Date and result of cervical cancerscreening test -or Date and result of cervical cancerscreening test and date of HPV test onthe same date of service -or Evidence of hysterectomy with noresidual cervixHPV ordered after positive Pap testingdoes not count as co-testingFemales Ages 21-64 Pap(2013/2014/2015)Females Ages 30-64 Papwith HPV co-testing results(2011–2015)Common Chart Deficiencies: Pap Smear test results not found in PCPcharts Incomplete documentation related tohysterectomy25
Frequency of OngoingDocumentation must have:Prenatal CareDate and documentation of all prenatal(FPC)visitsMost of this information is foundon the ACOG formACOG recommends 14 visits for a40 week pregnancyLive Births Deliveredon or between11/6/2014 to 11/5/2015and were continuouslyenrolled 42 days prior to deliveryCommon Chart Deficiencies:Must be “unduplicated” prenatal visits.If there is an office visit and the providerorders an U/S and labs and they aredone on separate days, all three wouldonly count as one date of service.26
Prenatal andPostpartumCare(PPC)Documentation must have:Prenatal Care: Prenatal visit during thefirst trimester or within 42 days ofenrollmentMost information is found on theACOG formPostpartum Care: Post-partum visit within21-56 days of deliveryCommon Chart Deficiencies: Live Births Deliveredon or between11/6/2014 to 11/5/2015 Prenatal care not done withintimeframeNo Postpartum care visitIncision check for post C-section doesnot constitute a postpartum visit27
H ybrid H E D IS M E A S URE SC H IL D A N D A D O L E S C E N T H E A L TH28
ChildhoodImmunization Status(CIS)Documentation must have:4 Dtap3 IPV1 MMR3 Hib3 HepB1 VZV4 PCV1 HepA2 or 3 RV1 FluDiphtheria, tetanus and cellularpertussisInactivated Polio VirusMeasles, Mumps, and RubellaHaemophilus influenza type BHepatitis BChicken PoxPneumococcal conjugateHepatitisRotavirusInfluenzaSubmit:% of children 2 years ofage who had all of the requiredimmunizations(2013-2015) Complete Immunization RecordsPM 160CAIR RecordsCopy of yellow immunization cardParental refusalAllergies ListHistory of Illness, as applicable29
ChildhoodImmunization Status(CIS)(Continued)Common Chart Deficiencies: Immunizations received after the 2ndbirthday PCP charts do not containimmunization records if received atHealth Department or school. Immunizations records given in thehospital at birth are not obtained No documentation of allergies orcontraindications No documentation of parental refusalIf missing any immunizations,please include: Documentation of parental refusal Documentation of request fordelayed immunization schedules Immunizations given athealth departments Immunizations given in thehospital at birth Documentation ofcontraindications or allergies30
HumanPapillomavirus Vaccine(HPV)Documentation must have:At least (3) three HPV vaccinations withdifferent dates of service. Submit: MD Progress note, PM 160, Copy ofimmunization record, CAIR RecordIf immunizations are missing please send: Documentation of parental refusal Copy of Immunization card Patient Contraindications/allergiesCommon Chart Deficiencies: HPV vaccines administered prior to the 9thbirthday or after the 13thbirthdayFemale adolescent PCP charts do not contain immunization3 doses of the HPV vaccine by age 13records if received elsewhere, i.e. Health2011 – 2015Departments and schools.between the 9th and 13th birthdays Immunizations not documented Parental refusal not documented31
Immunizations forAdolescents(IMA)Documentation must have: Date administered and typeCertificate of immunizationNotation of anaphylactic reactionIf immunizations are missing please send: Documentation of parental refusal Patient Contraindications/allergiesCommon Chart Deficiencies:Meningococcal 2013 – 2015(11th - 13th birthday)Tdap or Td 2012 – 2015(10th - 13th birthday) Immunizations not administeredduring timeframes Immunization records not found inthe PCP chart or Immunization card32
Weight Assessment &Counseling forNutrition&Physical Activity forChildren/Adolescents(WCC)Documentation must have:BMI date and percentileWeight date and valueHeight date and valueAge growth chart(s)BMI Value option removed for membersages 16-17, must be in percentile onlyCounseling for Nutrition:Documentation of discussion on diet andnutrition, checklist, referral to nutritionist,anticipatory guidance, or weight/ obesitycounselingAges 3-17Notation in the medical recordYear 2015Counseling for Physical Activity:Documentation of discussion on currentphysical activities, check list,counseling/referral , education,anticipatory guidance, or weight/ obesitycounseling33
Weight Assessment &Counseling forNutrition&Physical Activity forChildren/Adolescents(WCC)Common ChartDeficiencies: BMI documented as value (number) notas percentile BMI growth charts not submitted Anticipatory guidance does not alwaysaddress nutrition and physical activity Developmental milestones are notacceptable PM 160 forms do not address physicalactivity34
Well Child Visits inthe 3rd, 4th, 5th & 6thYears of Life(W34)Documentation must have: Health historyDevelopmental history - physicalDevelopmental history - mentalPhysical examHealth education/anticipatory guidancePreventive services may be rendered onvisits other than well-child visitsCommon Chart Deficiencies: Lack of documentation of required elementsAges 3 -6 yrs.At least ONE “Well-Child” visitwith a PCP in 2015 Children being seen for sick visits and therequired elements are not addressed35
Adolescent Well-Child Documentation must have: Health historyVisits Developmental history physical Developmental history mental(AWC) Physical exam Health education/anticipatory guidancePreventive services may be rendered onvisits other than well-care visits.Common Chart Deficiencies: Lack of documentation of required elementsAges 12 - 21 yrs.At least one “Well-Child” visitwith a PCP or an OB/GYN in 2015 Adolescents being seen for sick visits and therequired elements are not addressed36
Let’s See What You’ve Learned1. What does HEDIS Stand for?2. What is your role inHEDIS ?3. Do you need to send theentire record?4. What do you do if youhave questions?37
Got Questions?Email us at: HEDIS Ops@lacare.orgCheck out our website rcesClick on:HEDIS ResourcesFor helpful trainings and guides38
Resources at Your FingertipsPresentation and Trainings:HEDIS Overview PresentationWCC – Weight Assessment DocumentationHEDIS Made EasyGuidance Documents:HEDIS 2016 Measure CriteriaHEDIS at a GlanceHEDIS Measures HandoutHEDIS Measures PosterHEDIS Office Manager’s GuideProvider Opportunity ReportHEDIS Value Set Directory39
Question and Answer PeriodHEDIS is a registered trademark of the National Committee for Quality Assurance (NCQA).40HEDIS OPERATIONS HEALTHCARE OUTCOMES & ANALYSIS
H E D IS M ad e E asy 2 0 1 6TH E E N D41
(PPC) Live Births Delivered on or between 11/6/2014 to 11/5/2015. 28 C H IL D A ND A DOL ES C ENTH EA LTH H ybrid H EDIS M EA S URES. 29 Childhood I