Transcription
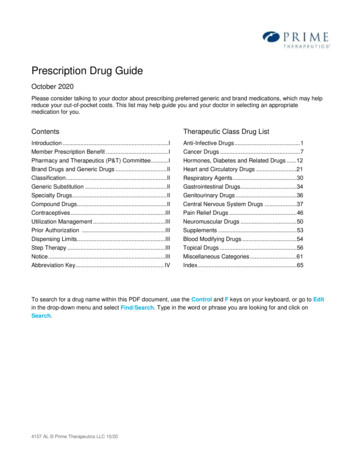
Prescription Drug GuideOctober 2020Please consider talking to your doctor about prescribing preferred generic and brand medications, which may helpreduce your out-of-pocket costs. This list may help guide you and your doctor in selecting an appropriatemedication for you.ContentsTherapeutic Class Drug ListIntroduction .IAnti-Infective Drugs . 1Member Prescription Benefit .ICancer Drugs . 7Pharmacy and Therapeutics (P&T) Committee .IHormones, Diabetes and Related Drugs .12Brand Drugs and Generic Drugs .IIHeart and Circulatory Drugs .21Classification .IIRespiratory Agents .30Generic Substitution .IIGastrointestinal Drugs.34Specialty Drugs .IIGenitourinary Drugs .36Compound Drugs .IICentral Nervous System Drugs .37Contraceptives .IIIPain Relief Drugs .46Utilization Management .IIINeuromuscular Drugs .50Prior Authorization .IIISupplements .53Dispensing Limits.IIIBlood Modifying Drugs .54Step Therapy .IIITopical Drugs .56Notice .IIIMiscellaneous Categories .61Abbreviation Key. IVIndex. 65To search for a drug name within this PDF document, use the Control and F keys on your keyboard, or go to Editin the drop-down menu and select Find/Search. Type in the word or phrase you are looking for and click onSearch.4157 AL Prime Therapeutics LLC 10/20
IntroductionThe Prescription Drug Guide includes all Preferred Brand drugs and a partial listing of Generic drugs. Brand namedrugs not listed in this Prescription Drug Guide are Non-Preferred Brands. A drug may not be added to the PreferredBrand tier for reasons including safety or effectiveness, or because a similar, more cost-effective drug is alreadyavailable as a Preferred Brand or Generic drug.Physicians are encouraged to prescribe drugs listed in this Prescription Drug Guide. Members are encouraged toshow this Prescription Drug Guide to their physician and pharmacist.Member Prescription BenefitThe prescription benefit is multi-tiered, placing prescription drugs into one of the following copayment levels.Tier 1 – Lowest copayment – Generic drugs and select Preferred Brand drugs– listed and unlisted generic drugsTier 2 – Middle copayment – Preferred Brand drugs – all shown in the Prescription Drug GuideTier 3 – Highest copayment – Non-Preferred Brand drugs – unlistedTier 4 – Specialty (if applicable)Coverage is limited to prescription products approved by the Food and Drug Administration (FDA) as evidenced by aNew Drug Application (NDA), Abbreviated New Drug Application (ANDA), or Biologics License Application (BLA) onfile. Any legal requirements or group specific benefits for coverage will supersede this (e.g., preventive drugs per theAffordable Care Act).The drug benefit includes most prescription drugs, although some restrictions and exclusions apply. Investigationaldrugs and drugs indicated for cosmetic purposes (e.g., Propecia for hair growth) are not covered. Coverage andcopayment levels vary depending on the plan. Drugs that require Prior Authorization, Step Therapy, or that haveDispensing Limits are noted in the Prescription Drug Guide.Pharmacy and Therapeutics (P&T) CommitteeThe P&T Committee is comprised of independent practicing physicians and pharmacists. The Committee meetsat least quarterly. Newly marketed prescription drugs may not be covered until the P&T Committee has had anopportunity to review the drug, to determine whether the drug will be covered and if so, which tier will apply basedon safety, efficacy, and the availability of other products within that class of drugs. If your physician feels that anew drug is medically necessary prior to P&T Committee evaluation, a non-formulary exception request forcoverage may be submitted.Prescription Drug Guide October 2020I
Brand Drugs and Generic DrugsClassificationPrescription drugs are classified as either a Brand drug or a Generic drug. The Brand or Generic status providedis by a nationally recognized company providing drug product information. The Brand/Generic status for a specificdrug/specific marketer can sometimes change over the life of a product in the marketplace and change fromBrand to Generic (or Generic to Brand). Such changes might change your copayment share. Brand drug orGeneric drug status is never based upon a product having a trade name. Generic drugs often have trade names.Generic SubstitutionGeneric drug utilization is encouraged as a way to provide high quality drugs at a reduced cost. Generic drugs areas safe and effective as their brand counterparts, but are usually less expensive. Generic drugs are manufacturedunder the same strict requirements of FDA’s current Good Manufacturing Practice regulations required for Branddrugs and cover the manufacturing, and identity, strength, purity and quality.An FDA-approved Generic drug may be substituted for the Brand counterpart when it: Contains the same active ingredient(s) as the brand drug Is identical in strength, dosage form, and route of administration Is therapeutically equivalent and can be expected to have the same clinical effect and safety profile.To encourage use of Generic drugs, Tier 2 Preferred Brand drugs typically move to Tier 3 after an equivalentgeneric version becomes available.Specialty DrugsSpecialty drugs are used in the treatment of medical conditions such as hepatitis, multiple sclerosis andrheumatoid arthritis. Specialty drugs may be oral or injectable medications that can either be selfadministered or administered by a health care professional.Some members must obtain their specialty drugs from the Pharmacy Select Network as the preferredprovider. If the preferred provider is not utilized you may be responsible for up to 100 percent of the drugcost. Your plan may have a different coverage level for self-administered specialty drugs. If you havequestions about your coverage for specialty drugs or your prescription drug benefit, call the number on theback of your ID card.Compound DrugsCompound drugs are defined as a drug product made or modified to have characteristics that are specificallyprescribed for an individual patient when commercial drug products are not available or appropriate. To beeligible for coverage, compounded drugs must contain at least one FDA-approved prescription ingredient andmust not be a copy of a commercially available product. All compounded drugs are subject to review and mayrequire prior authorization. Drugs used in compounded drugs may be subject to additional coverage criteria andutilization management edits. Compounds are covered only when medically necessary. Compound drugs arealways classified as the highest cost-sharing non-specialty drug Tier.Prescription Drug Guide October 2020II
ContraceptivesSome or all of the contraceptive methods or prescription drugs listed in this Prescription Drug Guide may not becovered under your plan because of your employer’s religious beliefs. To find out if contraceptive methods andprescription drugs are excluded, you may find this information in the exclusions section of your benefit booklet oryou may contact your group administrator.Utilization ManagementYour Plan is committed to supporting proper selection and use of drugs for its members. To help assure thesegoals are met, several programs have been developed to promote drug selection that encourages botheffectiveness and safety. Preferred generic or brand drugs requiring Prior Authorization or Step Therapy, or drugswith Dispensing Limits will be noted in the Therapeutic Class Drug List portion of the Prescription Drug Guide.Prior AuthorizationSome drugs require Prior Authorization (PA) because of their high potential for misuse or overuse. Drugs selectedfor Prior Authorization may require that specific clinical criteria are met before the drugs will be covered under amember’s prescription benefit. Approval is required for claims to process at network pharmacies.Dispensing LimitsDispensing Limits (DL) identify gender or age restrictions, and/or the maximum quantity that can be dispensedover a specific period of time. Limits are in place to encourage appropriate drug utilization, enhance memberoutcomes, and reduce drug benefit costs. Limits are typically developed based upon FDA-approved drug labeling.Step TherapyStep Therapy (ST) programs help manage the cost of expensive drugs by redirecting members to safe, effectiveand less expensive alternatives. Drugs included in the Step Therapy program require a more cost-effectiveprerequisite drug be tried before the Step Therapy drug will be approved for coverage. If the member meets theprerequisite requirement, the requested drug will be covered automatically without requiring review. If prerequisitedrugs are not found in the claims history, Prior Authorization may be required. Drugs and drug categories includedin the Step Therapy program are subject to change.NoticeThe purpose of the Prescription Drug Guide is to provide a guide to coverage. The Prescription Drug Guide is notintended to dictate to physicians how to practice medicine. Physicians should exercise their medical judgment inproviding the care they feel is most appropriate for their patients.Neither this Prescription Drug Guide, nor the successful adjudication of a pharmacy claim, is guarantee ofpayment.Prescription Drug Guide October 2020III
Abbreviation Keyaer. aerosolnebu . nebulizercap .capsulesodt. .orally disintegrating tabschew .chewableoint . ointmentconc . concentrateophth . ophthalmiccr. controlled releaseosm . osmotic releasedr . delayed releasepack . packetsec . enteric coatedpowd. powderequiv . equivalentpttw . twice-weekly patcher. extended releasesl . sublingualgm. gramsoln . solutioninhal. inhalersuppos . suppositoriesinj .injectionsusp . suspensionliqd. liquidtab . tabletsmg. milligramtd .transdermalml . milliliterw/ . withPrescription Drug Guide October 2020IV
ANTI-INFECTIVE DRUGSCEPHALOSPORINSPENICILLINScefaclor cap 250 mgamoxicillin (trihydrate) cap250 mgamoxicillin (trihydrate) cap500 mgamoxicillin (trihydrate) for susp125 mg/5mlamoxicillin (trihydrate) for susp200 mg/5mlamoxicillin (trihydrate) for susp250 mg/5mlamoxicillin (trihydrate) for susp400 mg/5mlamoxicillin (trihydrate) tab500 mgamoxicillin (trihydrate) tab875 mgamoxicillin & k clavulanate forsusp 200-28.5 mg/5ml11cefaclor cap 500 mgcefadroxil cap 500 mgcefadroxil for susp 250 mg/5ml1cefadroxil for susp 500 mg/5ml1cefdinir cap 300 mg11111amoxicillin & k clavulanatefor susp 250-62.5 mg/5ml(Augmentin)1amoxicillin & k clavulanate forsusp 400-57 mg/5ml1cefadroxil tab 1 gmcefdinir for susp 125 mg/5mlcefdinir for susp 250 mg/5mlcefixime cap 400 mg (Suprax)11111111cefpodoxime proxetil for susp50 mg/5ml1cefprozil for susp 125 mg/5mlcefprozil for susp 250 mg/5ml11111amoxicillin & k clavulanatefor susp 600-42.9 mg/5ml(Augmentin es-600)1amoxicillin & k clavulanate tab250-125 mg1ceftriaxone sodium for inj250 mg1ceftriaxone sodium for inj500 mg (Rocephin)1ceftriaxone sodium for inj 1 gm(Rocephin)11ceftriaxone sodi
Prescription Drug Guide October 2020 I Introduction The Prescription Drug Guide includes all Preferred Brand drugs and a partial listing of Generic drugs.