Transcription
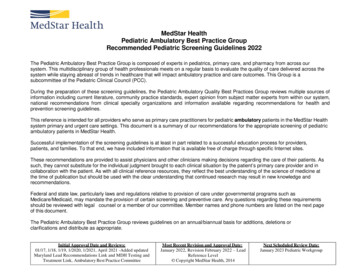
Fourth Quarter 2017MedStar Select/Medicare ChoiceProvider NewsletterMedStar Medicare Choice Vision Benefits and ProvidersThe vision networks for routine and medical vision are managed separately.Routine CareEffective Jan. 1, 2018, our MedStar Medicare Choice plans willoffer Routine vision care through Avesis. Members can be seenby providers within the Avesis network for routine visits. Pleasecontact Avesis at 844-478-0511 to confirm member benefits,eligibility and/or provider participation.Diabetes Eye ExamMembers with diabetes can receive one dilated retinal eye examper calendar year at no cost to them. Encourage your memberswith diabetes to schedule their eye exam today.Medical/Surgical CareMembers who have medical vision needs must use Ophthalmologists who are directlycontracted with our plan. We credential these providers and contract them for medical services.Therefore, par Ophthalmologists who perform medical procedures are listed on our website atMedStarProviderNetwork.org.MedStar Select Vision Benefits and ProvidersEffective Jan. 1, 2018, MedStar Select offers routine vision care through Group Vision Services.Members can be seen by providers within the Group Vision Services network for routine visits. Pleasecontact to confirm member benefits, eligibility, and/or provider participation at 866-265-4626.Medical/Surgical CareMembers who have medical vision needs must use Ophthalmologists who are directly contractedwith our plan. We credential these providers and contract them for medical services. Therefore, parOphthalmologists and Pediatric Ophthalmologists who perform medical procedures are listed on ourwebsite at MedStarProviderNetwork.org.
Laboratory, Radiology andDialysis ServicesElectronic AuthorizationSubmissionLaboratory services, refer to:There will be a new module to submit priorauthorizations electronically. Access to webbased submissions through Identifi Practice willbe a phased roll-out with select practices kickingoff the process in fall 2017. The objective is thatall practices will have the option of leveragingthis functionality prior to the end of the year. Any MedStar Health laboratory Quest Diagnostics (includes genetic testing) LabCorp (includes genetic testing)Visit MedStarProviderNetwork.org for acomplete listing of in-network laboratoryservices and locations.Radiology services, refer to: Any MedStar Health radiology facility Any contracted radiology providerVisit MedStarProviderNetwork.org for acomplete listing of in-network radiologyservices and locations.Dialysis CentersMedStar Medicare Choice: Fresenius Medical Care DaVita ARA-Adelphi, LLC BMA Capitol Dialysis, LLC FMC RAI Howard University Dialysis Center, LLC QCDC Southern Maryland Universal Dialysis Center, LLCMedStar Select: DavitaVisit MedStarProviderNetwork.org for acomplete listing of in-network dialysis centersand locations.2Those who wish to utilize this functionality willhave the option to access the module throughProvider OnLine with Single Sign On, or directlyto Identifi Practice.To access this functionality, provider mustemail mfc-providerrelations2@medstar.netto request permission and indicate if they areinterested in accessing through Provider OnLineor directly into Identifi Practice.If you are seeking access through the portal,you must first be a registered user with ProviderOnLine before the Electronic AuthorizationSubmission functionality can be offered.If you are not currently registered withProvider OnLine, instructions are located atMedStarProviderNetwork.org. A registeredAdministrator to Provider OnLine within yourpractice can also grant access to additional users.In-Network ReferralsAll providers are expected to utilize participatingproviders when making referrals.Please refer to the online directory atMedStarProviderNetwork.org for a list ofparticipating providers, or contract providerservices at 855-222-1042 for assistance. Pleasereview the information below on participatingproviders for lab, radiology, and dialysis services.
MedStar Select MyHealth Maternity ProgramThe MedStar Select MyHealth Maternity Program is available to MedStar Select members and theircovered dependents. The focus of the Maternity Care program is to promote optimal maternal andneonatal outcomes, including reduction in preterm births and neonatal hospitalizations, by earlyidentification of high risk pregnancies. Optimal maternal and neonatal outcomes are promoted byestablishing a collaborative relationship between the maternity health educator, registered nursecare advisor, and the associate or covered dependent, in which the associate or covered dependentis supported and encouraged to adopt a central role in managing their pregnancy and postpartumperiod. The associate or covered dependent will receive individualized support, education, andguidance throughout their pregnancy and postpartum period.Program Participation Guidelines: 50 into HRA for completing initial assessmentThe associate or covered dependent must enroll in the program and complete the initialassessment during the first trimester to qualify. 50 into HRA for completing the program, including the postpartum assessment with your MyHealthmaternity care advisorThe associate or covered dependent must have enrolled and completed the Initial Assessmentduring the first trimester to qualify. 100 into HRA for delivery at a MedStar Health facilityEnrollment into the program, completion of the initial assessment or postpartum assessment is notrequired to quality.For more information, members can call 888-959-4033 between 8:30 a.m. and 5 p.m. Mondaythrough Friday.MedStar Medicare Choice Participating Providers Please Confirm Directory Information!Please check MedStarProviderNetwork.org to confirm your office information is displaying correctlyon the searchable online directory.If there have been any changes or you become aware of an error, please resolve by emailing ProviderRelations at mfc-providerdemographics@medstar.net or calling 800-905-1722, option 5.Help us to ensure that MedStar Medicare Choice has the most accurate and up to date information!3
MyHealth Program HighlightsMyHealth Programs: Advising and Transition CareEach patient has a unique approach to accessing and utilizing healthcare services. In a continuedeffort to provide you with the tools needed to engage patients in better managing their chronicconditions, MedStar Health offers special programs to MedStar Select and MedStar MedicareChoice members. These programs are to include Care Advising and Transition Care.If your patient is enrolled in one of our programs and is admitted to a MedStar or non-MedStarfacility, we are able to notify you of the admission, send you records and test results, and provideyou with the necessary information and tools needed to follow up and provide optimal care foryour patient. This ability to share information and eliminate duplication helps us better managepatients with chronic conditions and decrease readmission rates.MedStar’s dedicated care advising and transition care teams help bridge the gaps to improvecare coordination. These services help MedStar Select and MedStar Medicare Choice memberswho need some extra support in managing their health. Whether the patient needs support with ashort-term solution, or help with a long-term care plan, Care Advising can offer valuable assistanceto your high-risk patients, as well as to Medicare members with a chronic special needs plan(CSNP) or dual special needs plan (DSNP).Care AdvisingIdentified patients engage with a registered nurse care advisor to help them follow their doctor’sorders, understand their test results and take their prescribed medication properly. Care advisorscan also help set follow-up appointments and coordinate important communication andinformation between the multiple providers the patient might be seeing.To ensure continuity of care, each enrolled patient and theirprimary care physician (PCP) will develop and maintain arelationship with the same care team. Care advisors are alsosupported by a broader care team, including social workers,pharmacists, and dietitians, all of whom help support andguide the patient through their personal care plan.Whatever support is needed, you and your patient will haveaccess to services such as nursing, pharmacy, nutrition,dietitians, social workers, and more.Care Advising services and the ongoing support that CareAdvising offers can improve the health of these patients andassist providers in managing their most vulnerable patients.The service also promotes active patient engagement, education, and understanding.For more information about our Care Advising services, please call 888-959-4033.4
Transition CareTransition Care, a hospital transition program, provides members with the necessary tools to gethealthy and stay well. Our Transition Care program helps patients decrease their chances of hospitalreadmission.While in the hospital, a patient is assigned to a transition coach who will educate them on how tosuccessfully adjust from hospital to home. The patient will leave the hospital with a printed care plan,including medication reminders and a list of follow-up appointments.In addition to giving the patient the much needed assistance to make a smooth transition from hospitalto home, the transition coach and the care advisor will follow up with the patient to ensure medicationadherence and confirm travel arrangements for upcoming physician appointments.If you have a MedStar Select or MedStar Medicare Choice patient who you feel would benefit fromTransition Care services, please call 888-959-4033.MedStar Medicare Choice Service Area ReductionMedStar Medicare Choice has decided to discontinue our Medicare Choice plans in certain counties for2018. Effective Jan. 1, 2018, MedStar Medicare Choice will no longer offer a Medicare Advantageproduct in Anne Arundel, St. Mary’s, Calvert, Charles and Baltimore counties. This change mayaffect the health coverage for some of your patients; however, it does not affect your provider contractwith MedStar Medicare Choice/MedStar Family Choice.In which counties will MedStar Medicare Choice operate for 2018?Effective Jan. 1, 2018, MedStar Medicare Choice will offer a Medicare Advantage Plan for patients livingin the following counties: Baltimore City, Harford, Howard, Prince George’s, and Washington, D.C.How does this affect your patients?MedStar Medicare Choice will no longer be a Medicare Advantage plan option for your patientsresiding in Anne Arundel, St. Mary’s, Calvert, Charles and Baltimore counties in 2018. This means theircoverage through MedStar Medicare Choice will end Dec. 31, 2017. Your affected patients need to makea decision about how they want to proceed with their health and prescription drug coverage. They mustchoose a different Medicare Advantage Health Plan, or revert back to Original Medicare. If they donot take action by Dec. 31, they will lose their prescription drug coverage and only be coveredby Original Medicare starting Jan. 1, 2018. Affected members can join a new plan anytime betweenOct. 15, 2017 and Feb. 28, 2018. If they don’t join a plan with prescription drug coverage by Feb. 28,2018, they won’t have prescription drug coverage in 2018 and may have to pay a lifetime Part D lateenrollment penalty if they join a Medicare prescription drug plan later.For patients who are enrolled in MedStar Dual Advantage (D-SNP) and also have coverage throughMedicaid, their coverage through Medicaid is not affected. Affected members may contact their salesbroker or call 800-MEDICARE (800-633-4227) to determine which option is best for them.For more information, please contact Provider Relations at 800-905-1722, option 5.5
Medicare Star Measures FAQs Including Pharmacy ImpactThis document was developed as a referenceguide, providing information about StarPharmacy measures and has been dividedinto three sections: Helpful Information,Provider Questions and Member Questions.encourages quality and performanceimprovement—with the goal of bettermedication adherence rates in members.Why is MedStar Focusing on Star Rating Now?This section shares information aboutStar Measures and why MedStar Healthwill be focusing on it this year.MedStar Medicare Choice wants to ensurethe health and wellbeing of our members.By increasing Star measure awareness in ourprovider community, we hope to encouragequality and performance improvement.What are the Centers for Medicare andMedicaid Services (CMS) Star Ratings?What do the Five-Star Rating MeasuresConsist of?CMS uses a five-star quality rating system tomeasure Medicare beneficiaries’ experiencewith their health plans and participating healthsystems. Medicare plans are measured on afive point rating scale. Five is the highest score.CMS bases the five-star rating system on arange of quality metrics, including clinicalmeasures (ie: blood pressure control forpatients with hypertension), member satisfactionand complaints and medication adherence.Why are Star Measures and Rating Important?Which Pharmacy Measures Should MedStarProviders Focus on?Helpful InformationThe five-star program is a key component infinancing health care benefits for MedicareAdvantage beneficiaries. This programBelow is a table listed the four quality measuresand their specific components.Quality Measure (Prior Authorization)Medication Adherence for DiabetesMedicationsMeasure SpecificsAny patient 18 years and older with a diabetesprescription should maintain 80 percent adherence.This includes drug therapy across the followingclasses of medications: biguanides, sulfonylureas,thiazolidinediones, and DiPeptidyl Peptidase (DPP)-IVinhibitors, incretin mimetics, and meglitinides.Medication Adherence for Hypertension Any patient 18 years and older with a prescription forMedicationsRAS antagonist medication should maintain80 percent adherence. This includes ACE, ARB, or a directrenin inhibitor drug.Medication Adherence for CholesterolAny patient 18 years and older with a prescription forMedicationscholesterol medication (a statin drug) should maintain80 percent adherence.Diabetes Treatment6Any patient who has both diabetes and high bloodpressure whose treatment included a renin angiotensinsystem (RAS) antagonist [ACE/ARB or direct renininhibitor] medication.
Provider Specific QuestionsThis section offers answers to common questionsour provider community may ask as it relates toStar Measures and improving pharmacy outcomes.I Recently Received a Pharmacy AdherenceReport? What Information is in This Report?Providers who have members eligible for thismeasure will receive a report called the “Point ofCare” report. This report showcases results of patientmedication adherence measures and can helpidentify which members may need some additionalassistance with their medications. The adherencemeasure is calculated based on the number of daysa patient has a filled medication out of the 365 daysof the year. A patient is considered noncompliantonce they fall below 80 percent adherence level.Non-compliant patients lower the overall adherencescore for the health plan.What Will Happen if the Medication AdherenceRates of My Patients do not Improve?As a provider led-health plan, our goal isto provide you with the resources necessaryto help your patients get and stay healthy.By working closely with your patients, togetherwith the care advising and pharmacy servicesteam, we are confident most patients’ adherencescores will improve.Unfortunately, there may be some patients thatare more challenging to work with. Patients whoseadherence rates fall below the 80 percent thresholdwill be considered non-compliant. Because thiscan reflect poorly on the care delivered by the planand provider, we are available to work with you inmeeting your patient’s needs.Member Specific QuestionsYour patients may be avoiding their medicationsfor the following reasons:This section offers answers to some commonquestions MedStar Medicare Choice membersmay ask. Please note, members may havequestions for the care advising team, memberservices and/or their provider. CostWhat if I Can’t Afford to Pay for My Medications? Access Unpleasant side effects ForgetfulnessThere are many low cost generic medications thatare available on the plans covered drug list. Forhelp in finding cost effective alternatives, reachout to your provider or call 800-772-1213 to beconnected with a care advisor.Some of My Patient’s Adherence Rates are LowerThan I Would Like. How Can I Help Them?As their provider, you may be able to help byconsidering the following: Why have they chosen not to continue theirmedications? What generic alternatives are available tothem? Do they have access to a pharmacy thatdelivers? Are they interested in enrolling in an autorefill program offered by mail order or a localpharmacy?What if I Can’t Get to a Pharmacy to Pick Up MyPrescription?If you are having trouble accessing a pharmacy,consider the following solutions: Mail Order: Your doctor can call or fax yourprescription to an Express Scripts mail orderfacility and deliver 90 days of medication ata time. Delivery Service: Check with your localpharmacy to see if they have a delivery service.(continued on next page)7
I Often Forget to Take My Medication. How CanI do a Better Job of Remembering?Consider purchasing a pill box that storesyour medication by day or time. Your clinicalpharmacist can help you do that. In addition,try setting daily reminders on your phone oralarm clock.I Can’t Recall if There has Been a Changein My Therapy?If you do not remember if and how yourmedication regimen has changed, feel freeto reach out to a clinical pharmacist or yourprovider. When you receive the informationyou are looking for, we suggest writing itdown and creating reminders.The Medication Side Effects I am Experiencingare Very Uncomfortable.What are My Options?Taking your prescribed medication is integralto your improved health and managementof disease. We do understand, however, thatcertain side effects can be uncomfortable.Before stopping or changing your medicationregimen, please speak with your provider andclinical pharmacist. Together, you may be ableto identify alternative medications.I am not Sure that My Medication hasAny Affect. Can I Stop Taking It?Your medication is necessary in treating yourcondition and preventing future catastrophicevents. Some medication benefits arenot noticeable, others are prescribed aspreventative measures. If you have concernsor questions, please reach out to your provideror clinical pharmacist.8I Feel Like I don’t Need My Medication Anymoreand My Friends and Family Agree. Can I StopTaking this Medication?Only your doctor can advise you to stop orchange your medication. Remember, somemedications are prescribed for prevention only. Inaddition, abruptly stopping your medication cansometimes cause serious complications. Pleasereach out to your provider with questions.What Should I Talk to My Provider Aboutat Our Next Appointment?Every visit to your doctor should consist of acomprehensive review of your medicationsso your doctor can be informed and betterassist you with cost, side effects or other healthimprovement tactics. If you have questions inbetween visits, feel free to call your provider’soffice or clinical pharmacist.
MedStar Medicare Choice Risk Adjustment Factor ProgramMedStar Medicare Choice is committed to the ongoing health and wellness of our Medicaremembers. We know that as our partner, you are the key to optimizing health outcomes and improvingthe member experience.We encourage participating providers to conduct an annual comprehensive exam and patientassessment for each of our MedStar Medicare Choice members. MedStar Medicare Choice willprovide you with patient data indicating specific patients on your panel that are due for thiscomprehensive exam via pre-populated forms as well as a member roster.Remember, capturing appropriate diagnosis codes on a medical claim drives improved patient careand clinical quality.Why Risk Adjustment is Important Enhances physicians’ understanding of their patient population’s chronic conditions Allows for an accurate account of the population’s clinical profile, including conditions treated byspecialists, complications, and comorbidities Helps identify previously undocumented suspect medical conditions through integration ofpatient data Encourages outreach to patients without regular visits to their primary care physician Provides fair payment for accurate treatmentEnhanced PaymentYou can receive a 200 reimbursement payment for completing the following: Conduct a face-to-face visit with a MedStar Medicare Choice member. Using the Patient Assessment Form (PAF), check the conditions that are currently affecting and notaffecting your patient’s care. During the face-to-face visit, discuss all ‘confirmed’ conditions with the member, making sure todocument them in the medical record and document a treatment plan for each condition. Submit the completed PAF worksheet via fax to 202-379-7826 or scan/email torafworksheet@evolenthealth.com. Bill the office visit with CPT Code 99429 and add the ICD-10 diagnosis codes for all ‘confirmed’conditions that were addressed during the visit.Note: Copayment, coinsurance and deductible amounts, if any, for MedStar Medicare Choicemembers are waived for these visits.Want to learn more about the Risk Adjustment Factor (RAF) Program?Receive 0.5 CME credits for viewing the RAF education video at MedStarProviderNetwork.org, thenclick on the Annual Required Training.Have further questions about Risk Adjustment or need your 2017 worksheets?Email us at medstarreports@evolenthealth.com.9
MedStar Medicare Choice Pharmacy BenefitsVisit MedStarProviderNetwork.org for more information regarding the MedStar MedicareChoice Pharmacy benefits, such as a directory of participating pharmacies, the formulary, andprior authorization forms. If your patient must take a non-formulary medication, an exception maybe available. To request an exception, complete the non-formulary exception form, posted onMedStarProviderNetwork.org under Pharmacy Prior Authorization forms. Please remember, ifapproved, the medication will be tiered as nonpreferred and may still incur significant costs for thepatient. Please call Evolent Health at 855-266-0712 with questions.Where can MedStar Medicare Choice Members get their Vaccines?Medicare beneficiaries MUST receive most of their vaccinations from a pharmacist at a pharmacy(mandated by the Medicare Part D benefit). If a Medicare beneficiary receives a vaccine that iscovered under the Medicare Part D benefit in a physician’s office rather than at a pharmacy, themember is responsible for the cost of the drug and the administration of the drug. In this instance,the Medicare beneficiary would have to submit for reimbursement from their Medicare Part Dplan administrator. Exception: Influenza, pneumonia, and tetanus (following an injury) are coveredthrough the member’s medical benefit and can be administered at and billed by a pharmacy, aphysician’s office, or an ER.Policies related to specific vaccines can be found acy-2016-Vaccine-Coverage.It’s flu season! We care about keeping our members healthy. Catching the flu can lead to seriousillness and hospitalization. Prevent the flu by reminding your patients to get their flu vaccine at no costto them.Helping Your MedStar Medicare Choice Patients Afford Their Diabetic CareFor many of your patients, caring for their diabetes is not only an emotional challenge, but also afinancial challenge. For some, this financial burden has led to medication adherence issues andother complications. If your patient is still struggling financially, patient assistant programs may beavailable. These programs are typically offered for brand-only medications and are sponsored by thedrug manufacturer. The following two websites can help in determining your patient’s eligibility forassistance programs: NeedyMeds.org and -income Medicare patients may also contact the Social Security Administration to determine ifthey qualify for Medicare Extra Help (low income subsidy), which may reduce their prescription costs.More information can be found at SocialSecurity.gov/ExtraHelp or by calling 800-772-1213.When prescribing for diabetic testing supplies, the covered manufacturer is Lifescan (OneTouchproducts). The quantity limit for blood glucose test strips is 150 strips per 30 days. If morefrequent testing is required, a quantity limit exception may be applied. Please complete the priorauthorization form found on MedStarProviderNetwork.org.10
Getting Ready for 2018 HEDIS SeasonEvery year, MedStar Health is required to report HEDIS data to the National Committee for QualityAssurance (NCQA). This reporting is also mandated by the Centers for Medicare & Medicaid Services(CMS) for Medicare Advantage plans. MedStar Health has contracted with Datafied to retrieve anymedical records necessary for HEDIS. Therefore, in the upcoming months, you may be receiving a callfrom Datafied requesting MedStar Health member’s records.What is HEDIS?The Healthcare Effectiveness Data and Information Set (HEDIS) is used bymore than 90 percent of America’s health plans to measure performance onimportant dimensions of care and service. It allows the comparison of healthplans in these key areas of measurement: Quality of care, access to care andmember satisfaction with the health plan and providers.1. When will the collection of these records occur?Medical record reviews can occur from Jan. 25 through May 9, 2018.2. Are all MedStar Health members’ records needed?No, records are only needed for a random subset of MedStar Health associates who are part ofMedStar Medicare Choice, MedStar Medicare Choice Dual Advantage, and MedStar MedicareChoice Care Advantage.3. Does the Health Insurance Portability and Accountability Act (HIPAA) permit me to releaserecords to Datafied for HEDIS data collection?Yes. As a MedStar Health contracted provider, you are permitted to disclose protected healthinformation (PHI) to Datafied, our contracted medical record reviewer. A signed consent fromthe member is not required under the HIPAA privacy rule for you to release the requestedinformation.4. Is my participation in HEDIS data collection mandatory?Yes. Network participants are contractually required to provide medical record information “forthe purpose of quality assurance,” and this includes HEDIS.5. What is my office’s responsibility regarding HEDIS data collection?You and your office staff are responsible for replying to the request from Datafied in a timelymanner and providing access to the requested records either by fax, mail, remote access to EMR,or on-site review.We appreciate your help with this annual quality of care and service initiative.11
MedStar Medicare Choice Annual TrainingAs a participating provider of MedStar Family Choice’s Medicare Choice product you arecontractually required to complete the MedStar Medicare Choice SNP Model of Care ProviderTraining (Earn 1.75 CMEs), the Medicare Parts C&D General Compliance Training and the CombatingMedicare Parts C and D Fraud Waste and Abuse training each calendar year.Be sure to attend all mandatory trainings.We would like to send a special thank you those who have already completed both trainings andnotified us. To receive credit for the MedStar Family Choice’s SNP Model of Care training and accompanyingCMEs you must complete and sign the attestation form at the end of the training and fax it to703-890-1636. This course is specific to our Medicare Choice product and as a result trainingstaken for other payers do not count towards our training requirement. To receive credit for the Parts C&D General Compliance training and the Combating MedicareParts C&D Fraud Waste and Abuse training you must submit a copy of each certificate that isawarded upon completion of the trainings to our Provider Relations department at800-905-1722, option 5 or to mfc-providerrelations2@medstar.net. These courses are notspecific to our Medicare Choice product and as a result trainings taken and certificates awardedfor other payers can count towards our training requirement.If you have not yet completed the training please follow the link below to complete the requiredtraining(s): le-Provider-TrainingSNP Model of CareMedStar Medicare Choice is working hard to continue its relevant communication with its networkof physicians, all while maintaining a zero dollar premium for its members. MedStar MedicareChoice has enrolled additional members into its Plans during the latest Annual Enrollment Period,and a good portion of these members are enrolled in one of two Special Needs Plans (SNP) in bothWashington, D.C., and Maryland. The Dual Special Needs Plan (D-SNP) serves patients eligible forboth Medicare and Medicaid and the Chronic Special Needs Plan (C-SNP) serves patients diagnosedwith diabetes and/or congestive heart failure (CHF).1. Medicare Parts C and D General Compliance TrainingA new Medicare Parts C and D General Compliance Training Web-Based Training (WBT) course isavailable through the Learning Management and Product Ordering System. Learn about: How a compliance program operates How compliance program violations should be reportedTo get your certificate you must go through the WBT itself. The PDF version is provided as a service12
to organizations to incorporate the CMS training content into existing training systems and writtendocuments and is not intended to take the place of the WBT, no certificate is provided with the PDFdownload.Download available at: wnload.pdfSponsors and/or FDRs will have three options for ensuring FDRs have satisfied the g
MedStar Select Vision Benefits and Providers Effective Jan. 1, 2018, MedStar Select offers routine vision care through Group Vision Services. Members can be seen by providers within the Group Vision Services network for routine visits. Please contact to confirm member benefits, eligibility, and/or provider participation at 866-265-4626.