Transcription
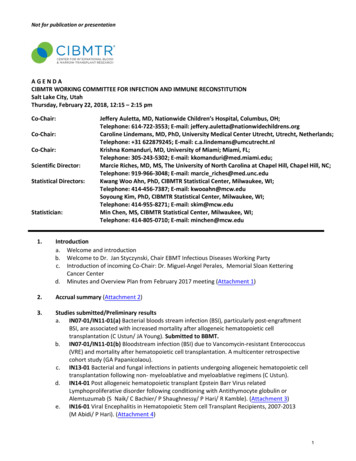
Not for publication or presentationAGENDACIBMTR WORKING COMMITTEE FOR INFECTION AND IMMUNE RECONSTITUTIONSalt Lake City, UtahThursday, February 22, 2018, 12:15 – 2:15 pmCo-Chair:Co-Chair:Co-Chair:Scientific Director:Statistical Directors:Statistician:Jeffery Auletta, MD, Nationwide Children’s Hospital, Columbus, OH;Telephone: 614-722-3553; E-mail: jeffery.auletta@nationwidechildrens.orgCaroline Lindemans, MD, PhD, University Medical Center Utrecht, Utrecht, Netherlands;Telephone: 31 622879245; E-mail: c.a.lindemans@umcutrecht.nlKrishna Komanduri, MD, University of Miami; Miami, FL;Telephone: 305-243-5302; E-mail: kkomanduri@med.miami.edu;Marcie Riches, MD, MS, The University of North Carolina at Chapel Hill, Chapel Hill, NC;Telephone: 919-966-3048; E-mail: marcie riches@med.unc.eduKwang Woo Ahn, PhD, CIBMTR Statistical Center, Milwaukee, WI;Telephone: 414-456-7387; E-mail: kwooahn@mcw.eduSoyoung Kim, PhD, CIBMTR Statistical Center, Milwaukee, WI;Telephone: 414-955-8271; E-mail: skim@mcw.eduMin Chen, MS, CIBMTR Statistical Center, Milwaukee, WI;Telephone: 414-805-0710; E-mail: minchen@mcw.edu1.Introductiona. Welcome and introductionb. Welcome to Dr. Jan Styczynski, Chair EBMT Infectious Diseases Working Partyc. Introduction of incoming Co-Chair: Dr. Miguel-Angel Perales, Memorial Sloan KetteringCancer Centerd. Minutes and Overview Plan from February 2017 meeting (Attachment 1)2.Accrual summary (Attachment 2)3.Studies submitted/Preliminary resultsa. IN07-01/IN11-01(a) Bacterial bloods stream infection (BSI), particularly post-engraftmentBSI, are associated with increased mortality after allogeneic hematopoietic celltransplantation (C Ustun/ JA Young). Submitted to BBMT.b. IN07-01/IN11-01(b) Bloodstream infection (BSI) due to Vancomycin-resistant Enterococcus(VRE) and mortality after hematopoietic cell transplantation. A multicenter retrospectivecohort study (GA Papanicolaou).c. IN13-01 Bacterial and fungal infections in patients undergoing allogeneic hematopoietic celltransplantation following non- myeloablative and myeloablative regimens (C Ustun).d. IN14-01 Post allogeneic hematopoietic transplant Epstein Barr Virus relatedLymphoproliferative disorder following conditioning with Antithymocyte globulin orAlemtuzumab (S Naik/ C Bachier/ P Shaughnessy/ P Hari/ R Kamble). (Attachment 3)e. IN16-01 Viral Encephalitis in Hematopoietic Stem cell Transplant Recipients, 2007-2013(M Abidi/ P Hari). (Attachment 4)1
Not for publication or presentation4.Studies in progress (Attachment 5)a. IN16-02 Determination of the burden of mucosal barrier injury-laboratory confirmedbloodstream infections (MBI-LCBI) in the first 100 days after stem cell transplant (C Dandoy/ PDaniels) Data file preparation (Attachment 6)b. IN17-01 Incidence and impact of cytomegalovirus and other viral infections, on posttransplant outcomes following HLA-haploidentical hematopoietic cell transplantationcompared to other donor sources. (Rizwan Romee/ Anurag Singh/ Randy Allison Taplitz)Protocol development (Attachment 7)5.Future/proposed studiesa. PROP 1707-01 Comparison of Early (d100) Infections after Haplo HCT between patientsreceiving Cy-based vs other GVHD prophylaxis (C Ustun/ G Papanicolaou) (Attachment 8)b. PROP 1710-06 Posa v Vori prophylaxis in patients with Allo HCT (S Farhan/ N Janakiraman/ EPeres) (Attachment 9)c. PROP 1711-57 Incidence and impact of C diff infection by day 100 on allo HCT outcomes (MRamanathan/ B Savani) (Attachment 10)d. PROP 1711-74 AlloHCT is feasible and effective for HIV positive patients with hememalignancies (SR Pingali/ A Mukherjee/ KUA Adekola) (Attachment 11)Dropped proposed studiesa. PROP 1710-13 Comparison of Cipro vs Levo in patients with AlloHCT. Dropped due tofeasibility-the data just started being requested Jan 2017.b. PROP 1711-17 Changing epidemiology of invasive pneumococcal infx since PCV vaccines.Dropped due to feasibility –We do not have the data to answer these questions.c. PROP 1711-62 Risk of CMV reactivation in Haplo patients with PTCY. Dropped due to overlapswith ongoing study IN1701d. PROP 1711-73 Association between respiratory viral infection and rates of GVHD by 2 yearsafter HCT. Dropped due to feasibilitye. PROP 1711-76 Impact of TMP/SMX prophy on rates of bacterial infection and NRM followingallogeneic HCT. Dropped due to feasibility-no data for duration of prophylaxis.6.Other Business2
Not for publication or presentationAttachment 1MINUTES AND OVERVIEW PLANCIBMTR WORKING COMMITTEE FOR INFECTION AND IMMUNE RECONSTITUTIONOrlando, FLSaturday, February 25, 2017, 12:15 – 2:15 pmCo-Chair:Co-Chair:Co-Chair:Scientific Director:Statistical Directors:Statistician:1.Jeffery Auletta, MD, Nationwide Children’s Hospital, Columbus, OH;Telephone: 614-722-3553; E-mail: jeffery.auletta@nationwidechildrens.orgCaroline Lindemans, MD, PhD, University Medical Center Utrecht, Utrecht, Netherlands;Telephone: 31 622879245; E-mail: c.a.lindemans@umcutrecht.nlKrishna Komanduri, MD, University of Miami; Miami, FL;Telephone: 305-243-5302; E-mail: kkomanduri@med.miami.edu;Marcie Riches, MD, MS, The University of North Carolina at Chapel Hill, Chapel Hill, NC;Telephone: 919-966-3048; E-mail: marcie riches@med.unc.eduKwang Woo Ahn, PhD, CIBMTR Statistical Center, Milwaukee, WI;Telephone: 414-456-7387; E-mail: kwooahn@mcw.eduSoyoung Kim, PhD, CIBMTR Statistical Center, Milwaukee, WI;Telephone: 414-955-8271; E-mail: skim@mcw.eduMin Chen, MS, CIBMTR Statistical Center, Milwaukee, WI;Telephone: 414-805-0710; E-mail: minchen@mcw.eduIntroductiona. Welcome and introductionDr. Jeffery Auletta moderated the introduction of the working committee followed by whichall the attending co-chairs and the statisticians were introduced.Dr. Auletta reviewed the goal of the working committee is to publish high impact studies in atimely manner. The expectations of the meeting are review of the current status of ongoingstudies and timelines and for members to assess and select proposals that will have a highimpact on the field. The working committee is limited by the complicated nature of infectiondata (Best before day 100) including data regarding infection prophylaxis.The working committee members were asked to vote on a level of scientific impact score, 1 isthe highest impact and 9 is the lowest impact score for the new proposals based on thefeasibility and impact on the transplant community. Due to limited statistical hours and ongoing work in the INWC, only one proposal will be accepted this year.Dr. Auletta mentioned the working committee’s membership is open to any individual willingto take an active role in study development and completion. He emphasized the rules ofAuthorship: 1. substantial and timely contributions to conception and design, acquisition ofdata, or analysis and interpretation of data; 2. drafting the article or revising it critically forimportant intellectual content; 3. final approval of the version to be published. All three3
Not for publication or presentationAttachment 1conditions must be met. The studies that are closest to submission will receive highestpriority.Last, Dr. Auletta introduced sources of HCT data in the CIBMTR. Dr. Marcie Riches emphasizedinfection information only available in CRF forms, which is a subset of reported patients basedupon an internally reviewed selection algorithm.b. Minutes and Overview Plan from February 2016 meetingThe minutes and overview plan from the 2016 Tandem meeting held in Honolulu, Hawaiiwere reviewed and approved by committee members.2.Published papersDr. Jeffery Auletta reported that the infection working committee has published four papers inthe past year.IN10-01 Karen Ballen, Kwang Ahn , Min Chen , Dr. Hisham Abdel-Azim , Ibrahim Ahmed , Dr.Mahmoud Aljurf , Dr. Joseph Antin , Ami Bhatt , Michael Boeckh , George Chen , Dr.Christopher Dandoy , Dr. Biju George , Mary Laughlin , Dr. Hillard Lazarus , Dr. MargaretMacMillan , David Margolis , Prof. David Marks , Dr. Maxim Norkin , Dr. Joseph Rosenthal ,Ayman Saad , Prof. Bipin Savani , Dr. Harry Schouten , Jan STOREK , Paul Szabolcs , Dr.Celalettin Ustun , Dr. Michael Verneris , Dr. Edmund K Waller , Dr. Daniel Weisdorf , Dr.Kirsten Williams , John Wingard , Baldeep Wirk , Tom Wolfs , Jo-Anne Young , Jeffery Auletta ,Dr. Krishna Komanduri , Dr. Caroline Lindemans , Dr. Marcie Riches: Infection Rates amongAcute Leukemia Patients receiving Alternative Donor Hematopoietic Cell Transplantation.Biol Blood Marrow Transplant 22(9):1036-1645b. IN09-01 Richard Maziarz, Dr. Ruta Brazauskas , Min Chen , Dr. Aleksandra McLeod , Dr.Rodrigo Martino , John Wingard , Dr. Mahmoud D Aljurf , Minnoo Battiwalla , Dr. ChristopherDvorak , Prof. Biju George , Dr. Eva Guinan , Dr. Gregory Hale , Dr. Hillard Lazarus , Prof. JongWook Lee , Dr. Jane Liesveld , Dr. Muthalagu Ramanathan , Dr. Vijay Reddy , Prof. Bipin Savani, Dr. Franklin Smith , Dr. Lynne Strasfeld , Dr. Randy Taplitz , Dr. Celalettin Ustun , Dr. MichaelBoeckh , Dr. Juan Gea-Banacloche , Dr. Caroline Lindemans , Jeffery Auletta , Dr. MarcieRiches : Outcomes of allogeneic HSCT for patients with hematologic malignancies (AML, ALL,MDS, CML) with and without pre-existing fungal infections- pre-existing invasive fungalinfection is not a contraindication for subsequent HSCT: a CIBMTR study. Bone MarrowTransplantation. doi:10.1038/bmt.2016.259. Epub 2016 Dec 19.c. IN12-01a Pierre Teira, Minoo Battiwalla, Muthalagu Ramanathan, Kwang Woo Ahn, Min Chen,Jaime Green, Ayman Saad, Joseph H. Antin, Bipin N. Savani, Hillard M. Lazarus, MatthewSeftel, Wael Saber, Carolyn Behrendt, David Marks, Mahmoud Aljurf, Maxim Norkin, John R.Wingard, Caroline A. Lindemans, Michael Boeckh, Marcie L. Riches, Jeffery J. Auletta: EarlyCytomegalovirus reactivation remains associated with increased transplant related mortalityin the current era: a CIBMTR analysis. Blood 127(20):2427-2438d. IN12-01b Muthalagu Ramanathan , Pierre Teira , Minnoo Battiwalla , Dr. A. Barrett , KwangAhn , Min Chen , Carolyn Behrendt , Jaime Green , Mary Laughlin , Dr. Hillard Lazarus , Prof.David Marks , Ayman Saad , Dr. Matthew Seftel , Dr. Wael Saber , Prof. Bipin Savani , Dr.Edmund K Waller , John Wingard , Jeffery Auletta , Dr. Caroline Lindemans , Michael Boeckh ,Dr. Marcie Riches : Impact of Early Cytomegalovirus Reactivation in Cord blood Stem CellRecipients in the Current Era. Bone Marrow Transplant 51(8):1113-1120a.4
Not for publication or presentation3.Studies with Preliminary ResultsDr. Jeffery Auletta also introduced two studies with preliminary results.a. IN07-01/IN11-01 Early Bacterial infection in patients undergoing allogeneic HCT (M Robien/GPapanicolaou/Celalettin Ustun/ JA Young)Two manuscripts are under preparation based on this study. One of them has been acceptedas a poster in this tandem meeting.b.4.Attachment 1IN13-01 Bacterial and fungal infections in patients undergoing allogeneic hematopoietic celltransplantation following non- myeloablative and myeloablative regimens (C Usten)The final analysis has been circulated to the writing comment for comments and themanuscript is under preparation.Studies in progressDr. Krishna Komanduri mentioned the ongoing studies.a.IN14-01 Post allogeneic hematopoietic transplant Epstein Barr Virus relatedLymphproliferative disorder following conditioning with Antithymocyte globulin orAlemtuzumab (S Naik, C Bachier, P Shaughnessy, P Hari, R Kamble) Date file preparationDr. Jeffery Auletta updated the study on behalf of the PIs.The specific aims of this study are: to describe the characteristics of patients with posttransplant lymphoproliferative disorders (PTLD) following allogeneic hematopoietic celltransplantation (allo HCT); To determine morbidity and outcomes associated with EpsteinBarr virus (EBV) positive and EBV negative PTLD. The current population has 236 EBV positivepatients and 34 EBV negative patients. 190 path reports have been reviewed.Comments from Working Committee:- Campath may effect EBV. Dr. Riches mentioned few patients received Campath in thecurrent population.- Assessment of prior use of Rituximab in the conditioning regimen. It was noted thatsince the patients included did not have B-cell lymphoma as the disease fortransplant, it was unlikely that patients had received Rituximab during theconditioning regimen.b. IN16-01 Viral Encephalitis in Hematopoietic Stem cell Transplant Recipients, 2007-2013(M Abidi, P Hari) Protocol developmentDr Abidi Maheen updated the study.The objectives of the study are: to describe the frequency and significance of viral DNAdetection in cerebrospinal fluid (CSF) in hematopoietic stem cell transplant (HCT) recipientsscreened for viral encephalitis; to determine the OS of patients with viral encephalitis afterHCT. The primary endpoint will be overall survival of patients developing EBV positive andEBV negative PTLD. The secondary endpoints will be time to onset of PTLD. Factors attransplant impacting outcomes following diagnosis of EBV positive PTLD. There are 118patients in the current population.Dr. Komanduri expressed surprise by how much HHV6 dominated the infections in this study.The lack of viremia may due to some centers do not test viremia routinely until recently. Dr.5
Not for publication or presentationAttachment 1Riches pointed out, during the time period, cord blood transplants were over selected and itmay potentially skew the data.c.Additional issues raised by the working committee:1. Limitations include: no clear systematic evaluation of patients, unknownsymptomatology triggering LP, inability to determine HHV6 latency in the study,inability to have a control cohort that also had an LP- These limitations may result in erroneous conclusions2. Discussion of unpublished data from NIH suggesting a low level of HHV-6 in the CSFwhen tested in patients receiving intrathecal chemotherapy3. Should we address the season of the year for the encephalitis?IN16-02 Determination of the burden of mucosal barrier injury-laboratory confirmedbloodstream infections (MBI-LCBI) in the first 100 days after stem cell transplant (C Dandoy, PDaniels) Protocol developmentDr. Christopher Dandoy updated the study.This study hypothesizes that patients in the first 100 days after stem cell transplant whodevelop mucosal barrier injury laboratory confirmed bloodstream infections (MBI-LCBI) haveincreased transplant related mortality (TRM) and decreased overall survival (OS) compared tothose with no infection or an infection not classified as an MBI-LCBI. The Specific Aims of thestudy are: compare TRM and OS post-SCT between patients who develop a MBI-LCBI versusthose with no infection or a non-MBI-LCBI in the first 100 days; Determine the incidence ofMBI-LCBIs in the first 100 days post SCT; Determine the risk factors for development of a MBILCBI in the first 100 days; and determine the timing of MBI-LCBI after SCT. The outcomes ofthe study are: overall survival; transplant related mortality (TRM); Incidence of MBI-LCBIwithin the first 100 days; and Incidence of bloodstream infections (bacterial and fungal) notmeeting criteria for MBI-LCBI; and infection as primary or secondary cause of death by day100 and by 1 year.A bloodstream infection will be classified as a MBI-LCBIs if it meets both the organism criteriaand the patient criteria from the NHSN.Study strengths are: Large sample size, Contemporary, Reflects the global reality of HSCT byincluding all centers, Identify MBI-LCBI burden for public health reporting, Public healthimplications and should target major public health journal such as JAMA.Comments:- Important topic for hospital epidemiology/infection control- Consider inclusion of autologous transplants5.Future/proposed studiesDr Caroline Lindemans reported that 9 proposals were received this year and 4 will be presented.Since there is significant overlap of Prop 1611-02, Porp1611-117 and Prop1611-134, we proposeto merge the three proposals into one study to maximize efficiency and statistical hours.a.PROP1605-01 Clinical outcomes for patients with invasive fungal infections undergoinghematopoietic stem cell transplant, (Myeloablative vs. Nonmyeloablative/Reduced intensitystem cell transplant) in the era of newer anti-fungals, 2009-2015 (Maheen Abidi/6
Not for publication or presentationAttachment 1Mark R. Litzow/M. Rizwan Sohail/Randall C. Walker)Dr. Maheen Abidi presented the proposal.The objectives of this proposal are: 1. Study period 2010-2015 in era of newer antifungals;compare results with outcomes of IFIs that underwent HSCT 1995-2009 (IN09-01); 2.Determine outcomes & mortality rates of patients with leukemia & other hematologicmalignancies with & without IFIs that undergo HSCT; 3. Determine the relationship betweenIFIs and the incidence & severity of GVHD & on relapse rates.Dr. Riches answered the question regarding why limited the patients with 2046 and 2146form (fungal supplemental forms) only, since the requested information is available only inthe 2046/2146 form. Dr. Komanduri suggested adding time from diagnosis to transplant, ortime of remission. Since delay of transplant will increase the relapse mortality.Committee Discussion:- Inability to determine if the fungal infection is possible/probable/proven- Lack of information of the status of the infection at the time of transplantb. PROP 1611-02 The Incidence of Cytomegalovirus Viremia and Disease following HLAHaploidentical Hematopoietic Cell Transplantation Compared to HLA-Matched Related Donor,Matched Unrelated Donor, and Umbilical Cord Blood Transplantation (Rizwan Romee /Ephraim Fuchs/ Asad Bashey/ Stefan Ciurea)Dr. Scott Goldsmith presented the proposal.The hypotheses of the study are: Incidence of CMV reactivation and disease higher afterhaploHCT with PTCy compared to MUD/MRD/UCB; CMV reactivation does not promotedecreased relapse, or longer DFS or OS in haploHCT. The Inclusion criteria are: Hememalignancy, age 18 years, and HCT between 2008-2015; HaploHCT w/ PTCy, UCB, 8/8 MUD,MRD. The exclusion criteria are: Ex-vivo T-cell depletion; HaploHCT for benign condition; Lackof donor/recipient CMV serostatus. The Primary Endpoint are: Compare incidence of CMVreactivation and disease between haploHCT w/ PTCy to MRD/MUD/UCB. SecondaryEndpoints: Determine association of CMV donor/recipient serostatus with CMV disease;Compare DFS, relapse, NRM, GVHD and GRFS between the groups (Association with CMVreactivation; Association with CMV donor/recipient serostatus; Subset analysis for patientswith AML).c.PROP 1611-117 Impact of CMV Reactivation on Relapse of Hematological Malignancies afterHaploidentical HSCT: a CIBMTR Analysis (Anurag Singh/ Siddhartha Ganguly) (Attachment 11)Dr. Anurag Singh presented the proposal.The specific aim of the study is to describe the effect of early CMV reactivation on relapse inthe setting of haploidentical transplant. The Inclusion criteria are: patients receiving a firstallogeneic transplantation for any AML, MDS, ALL and lymphomas from a haploidenticaldonor between 2000 and 2015 and reported to the CIBMTR. The exclusion criteria are:Second transplant or more; lack of day 100 follow-up forms capturing CMV reactivation data.The statistical methods are: Patient-, disease-, and transplant-related factors will becompared among groups using the Pearson χ2 test for discrete variables and the KruskalWallis test for continuous variables.7
Not for publication or presentationAttachment 1d. PROP 1611-134 Incidence and Outcomes of individuals with and without viral infections inrecipients of haploidentical versus other allogeneic hematopoietic stem cell transplantationfor patients with hematologic malignancies (Randy Allison Taplitz/ Carolyn Mulroney/ RichardMaziarz) (Attachment 12)Dr. Randy Allison Taplitz presented the proposal.This study hypothesizes that outcomes of treatment related mortality, overall survival,relapse rate, GVHD, diagnosis of bronchiolitis obliterans/COP, leukemia-free survival andpresence of co-infection in patients with any viral infections after transplant will be inferior inthose patients receiving haploidentical donors vs some other donor type transplant(compared separately – cord and mismatched unrelated, matched transplants; and as agroup). Characteristics of patient who underwent first Allo transplant with AML, ALL, MDS,CML, CLL, NHL, HL, plasma cell disorders and severe aplastic anemia reported to the CIBMTRfrom 2010-2015Dr. Marcie Riches mentioned, if we decide this combined proposal proceed forward, we haveto redefine the population. Dr. Komanduri is concerned the testing methods changeovertime, so some compromise has to be made.Committee Discussion (for proposals b – d)- Issues of Haploidentical with post-transplant cyclophosphamide vs without PTCy- Issues of PTCy in donors other than Haploidentical- Consideration of including an lymphocyte recovery data at day 100- Limited data/events for viruses other than CMV- Can we include information on duration of CMV reactivation (data not available)and treatment of CMV (data not available)Chairs discussion: Is there a way to collaborate with the EBMT to increase the Haplopopulation?Dropped proposed studiesa. PROP 1611-72 CMV exposure of cord blood donor- Impact on CMV reactivation in therecipient. Dropped due to feasibility-low number of patients.b. PROP 1611-151 Immune Reconstitution and its relation with Infectious Morbidity PostAutologous Peripheral Blood Stem Cell Transplantation (PBSCT). Dropped due to feasibility the CIBMTR does not capture the data required to answer the hypothesis.c. PROP 1611-122 Outcomes from progressive multifocal leukoencephalopathy inhematopoietic stem cell transplant patientsDropped due to feasibility-low number of patientsd. PROP 1611-54 The Effect of Antibacterial Prophylaxis on Early Post-transplant Mortality inPatients with Multiple Myeloma and Lymphoma Undergoing High-dose Chemotherapy andAutologous Stem Cell Transplantation. Dropped due to feasibilitye. PROP 1611-01 Infection Density per Donor Type and Conditioning Intensity and TheirAssociation with NRM in 3 different time points (0-33, 34-66, and 67-100 days) within 100days after alloHCT. Dropped due to low scientific impact8
Not for publication or presentation6.Attachment 1Other BusinessDr. Marcie Riches presented the infection form updates.The following sections have/will be updated:1. Infection Prophylaxis data (activated Jan 2017)2. PostHCT infection data capture revisions (activated Jan 2017)3. Revised organism lists focusing on viral and fungal infections (activated Jan 2017)4. 2046/2016 form (fungal infection form) (anticipated July 2017)5. 2149 form (Respiratory Virus form) (anticipated July 2017)6. 2150 form (CMV/EBV/ADV/HHV-6 form) (anticipated July 2107)Working Committee Overview Plan for 2017-2018a. IN07-01/IN11-01 Early bacterial infection in patients undergoing allogeneic HCT (C Ustun /J-A Young/MRobien/G Papanicolaou).i. VEP vs LEP BSI: Plan to submit to Blood by June 2017. We anticipate the paper is publishedby June 30, 2018. (Hour to completion: 60; Allocated by Jun 30, 2017: 60)ii. VRE vs Other BSI: Plan to submit to Blood by June 2017. We anticipate the paper ispublished by June 30, 2018. (Hour to completion: 60; Allocated by Jun 30, 2017: 60)b. IN 13-01 Bacterial and fungal infections in patients undergoing allogeneic hematopoietic celltransplantation following nonmyeloablative and myeloablative regimens (C Usten). Plan to submit toBBMT by July 2017. We anticipate paper is published by June 30, 2018. (Hour to completion: 70;Allocated by Jun 30, 2017: 70)c. IN 14-01 (PROP 1303-03/PROP1311-19): Post allogeneic hematopoietic transplant Epstein Barr Virusrelated lymphproliferative disorder following conditioning with antithymocyte globulin or alemtuzumab(R Kamble/ P Hari/S Naik /C Bachier/P Shaughnessy). We anticipate paper is submitted by June 30, 2018(Hour to completion: 150; Allocated by Jun 30, 2017: 150)d. IN16-01 Viral encephalitis in hematopoietic stem cell transplant recipients, 2007-2013 (Maheen Abidi/Parameswaran Hari) (PROP1510-16). We anticipate paper is published by June 30 2018. (Hour tocompletion: 230; Allocated by Jun 30, 2018: 230)e. IN16-02 Determination of the burden of mucosal barrier injury-laboratory confirmed bloodstreaminfections in the first 100 days after stem cell transplant (Christopher Dandoy/ Paulina Daniels) (PROP1511-85). We anticipate receiving the paper for submission by June 30, 2018. (Hour to completion: 300;Allocated by Jun 30, 2018: 300)f.IN17-01 Incidence and Outcomes of individuals with and without viral infections in recipients ofhaploidentical versus other allogeneic hematopoietic stem cell transplantation for patients withhematologic malignancies (Rizwan Romee/ Ephraim Fuchs/ Asad Bashey/ Stefan Ciurea/ Anurag Singh/Siddhartha Ganguly/ Randy Allison Taplitz/ Carolyn Mulroney/ Richard Maziarz). We anticipate data fileready for analysis by June 30, 2018. (Hour to completion: 310; Allocated by Jun 30, 2018: 160)9
Not for publication or presentationAttachment 1Work Assignments for Working Committee Leadership (March 2017)Jeffery AulettaIN07-01/IN11-01: Early bacterial infection in patients undergoing allogeneic HCTCarolineLindemansIN13-01 Bacterial and fungal infections in patients undergoing allogeneichematopoietic cell transplantation following non- myeloablative and myeloablativeregimens.Jeffery AulettaIN14-01 Post allogeneic hematopoietic transplant Epstein Barr Virus relatedlymphproliferative disorder following conditioning with antithymocyte globulin oralemtuzumab (R Kamble/ P Hari/S Naik /C Bachier/P Shaughnessy)KrishnaKomanduriIN16-01 Viral encephalitis in hematopoietic stem cell transplant recipients, 2007-2013(Mhaeen Abidi/ Parameswaran Hari)CarolineLindemans andJeffery AulettaIN16-02 Determination of the burden of mucosal barrier injury-laboratory confirmedbloodstream infections in the first 100 days after stem cell transplant (ChristopherDandoy/ Paulina Daniels)CarolineLindemans andKrishnaKomanduriIN17-01 Incidence and Outcomes of individuals with and without viral infections inrecipients of haploidentical versus other allogeneic hematopoietic stem celltransplantation for patients with hematologic malignancies(Rizwan Romee/ EphraimFuchs/ Asad Bashey/ Stefan Ciurea/ Anurag Singh/ Siddhartha Ganguly/ Randy AllisonTaplitz/ Carolyn Mulroney/ Richard Maziarz). (PROP 1611-02/1611-117/1611-134)10
Not for publication or presentationAttachment 2Accrual Summary for Infection and Immune Reconstitution Working CommitteeDonor-recipient and Infection information reported to the CIBMTR after 2008Characteristics of PatientsNumber of PatientsInfectionInfectionDonor/recipient CMV status-/ /-/ / Missing/not testedDonor/recipient hepatitis B status-/ /-/ / Missing/not testedDonor/recipient hepatitis C status-/ /-/ / Missing/not testedFungal Infection historyNoYesMissingFungal Infection after starting of conditioningNoYesMissingInfection prophylaxis after starting of conditioningNoYesMissingImmune ReconstitutionIgG at 100 dayData not availableData 4 (23)2773 (11)6302 (26)8379 (34)1648 ( 7)N/A9160 (37)281 ( 1)384 ( 2)107 ( 1)14774 (60)N/A9437 (38)63 ( 1)97 ( 1)6 ( 1)15103 (61)N/A22686 (92)1994 ( 8)26 ( 1)10483 (99)110 ( 1)2 ( 1)19553 (79)4679 (19)474 ( 2)9262 (87)613 ( 6)720 ( 7)326 ( 1)24112 (98)268 ( 1)227 ( 2)10143 (96)225 ( 2)9038 (37)15668 (63)4401 (42)6194 (58)11
Not for publication or presentationCharacteristics of PatientsIgM at 100 dayData not availableData availableIgA at 100 dayData not availableData availableCD3 at 100 dayLymphocyte analyses were not performedData not availableData availableCD4 at 100 dayLymphocyte analyses were not performedData not availableData availableCD8 at 100 dayLymphocyte analyses were not performedData not availableData availableCD20 at 100 dayLymphocyte analyses were not performedData not availableData availableCD56 at 100 dayLymphocyte analyses were not performedData not availableData availableInfection ProphylaxisAntibioticsNoYesMissingAntifungal inAttachment 2AllogeneicN(%)AutologousN(%)16414 (66)8292 (34)5086 (48)5509 (52)16416 (66)8290 (34)5039 (48)5556 (52)14239 (58)4297 (17)6170 (25)9356 (88)694 ( 7)545 ( 5)14239 (58)4377 (18)6090 (25)9356 (88)691 ( 7)548 ( 5)14239 (58)4517 (18)5950 (24)9356 (88)718 ( 7)521 ( 5)14239 (58)8829 (36)1638 ( 7)9356 (88)1118 (11)121 ( 1)14239 (58)6542 (26)3925 (16)9356 (88)1010 (10)229 ( 2)8450 (34)15988 (65)268 ( 1)3914 (37)6456 (61)225 ( 2)9496 (38)14942 (60)268 ( 1)6658 (63)3712 (35)225 ( 2)20741 (84)1626 ( 7)2339 ( 9)9142 (86)71 ( 1)1382 (13)12
Not for publication or presentationCharacteristics of oYesMissingOther systemic antifungal agentNoYesMissingAntiviral achment 2AllogeneicN(%)21221 (86)1156 ( 5)2329 ( 9)AutologousN(%)9158 (86)55 ( 1)1382 (13)14845 (60)8291 (34)1570 ( 6)6563 (62)3481 (33)551 ( 5)21937 (89)403 ( 2)2366 (10)9172 (87)42 ( 1)1381 (13)19328 (78)3333 (13)2045 ( 8)9093 (86)133 ( 1)1369 (13)19712 (80)2795 (11)2199 ( 9)9181 (87)35 ( 1)1379 (13)22151 (90)23 ( 1)2532 (10)9013 (85)5 ( 1)1577 (15)16597 (67)5989 (24)2120 ( 9)9047 (85)169 ( 2)1379 (13)21854 (88)569 ( 2)2283 ( 9)9148 (86)66 ( 1)1381 (13)4651 (19)19787 (80)268 ( 1)1732 (16)8638 (82)225 ( 2)7310 (30)16399 (66)997 ( 4)2492 (24)7377 (70)726 ( 7)13
Not for publication or presentationCharacteristics of iclovirNoYesMissingValacyclovirNoYesMissingOther antiviral agentNoYesMissingPneumocystis agentNoYesMissingOther prophylaxis agentNoYesMissingDiseaseAcute Leukemia/MDSChronic LeukemiaNon-Hodgkin LymphomaHodgkin LymphomaSolid tumorsMyeloma/Plasma Cell DisorderNon-malignant disordersYear of transplant2008200920102011
Dr. Marcie Riches emphasized infection information only available in CRF forms, which is a subset of reported patients based upon an internally reviewed selection algorithm. b. Minutes and Overview Plan from February 2016 meeting The minutes and overview plan from the 2016 Tandem meeting held in Honolulu, Hawaii