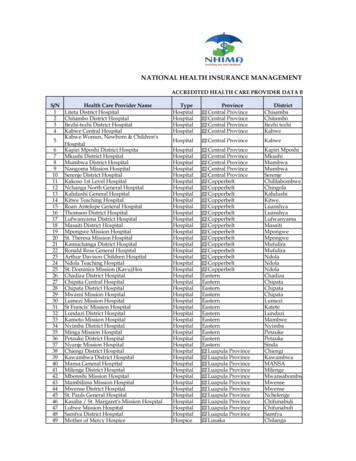
Transcription
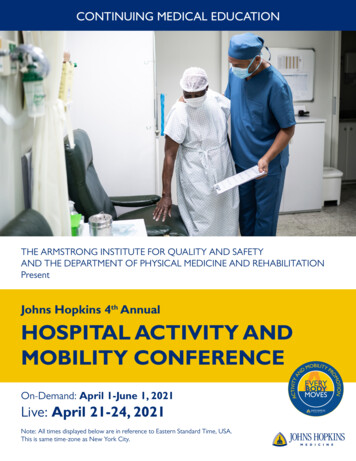
CONTINUING MEDICAL EDUCATIONTHE ARMSTRONG INSTITUTE FOR QUALITY AND SAFETYAND THE DEPARTMENT OF PHYSICAL MEDICINE AND REHABILITATIONPresentJohns Hopkins 4th AnnualHOSPITAL ACTIVITY ANDMOBILITY CONFERENCEOn-Demand: April 1-June 1, 2021Live: April 21-24, 2021Note: All times displayed below are in reference to Eastern Standard Time, USA.This is same time-zone as New York City.
Johns Hopkins Activity & MobilityPromotion (JH-AMP) firmly establishes theconcept that a systematic approach is beneficialin combating the harms of immobility in ourhospitals. While evidence supports the benefitsof mobility, implementation has been challengedby clinical “silos” and competing hospitalpriorities. Implementing interventions requirescreating a new collaborative culture and aligningclinical priorities.This conference features presentations bymembers of the inter-professional team whohave developed this new collaborative culture,successfully integrating mobility as an essentialcomponent of hospital operations, qualityimprovement and safety efforts.Who Should Attend?This activity is intended for physicians, nurse practitioners, nurses, occupational therapists, physiatrists, physical therapists,physician assistants, psychologists, administrators, hospitalists, surgeons and safety-quality professionals.ObjectivesAfter attending this activity, the learner will demonstrate the ability to: Appraise the evidence supporting mobility in the hospital. Describe mobility within the context of safe-patient handling and other hospital safety initiatives. Explain the tenets and methods of a structured quality improvement process for developing and implementing asystem mobility program in the acute hospital setting. Explain current practice and inter-disciplinary roles in an adult mobility program. Describe how to create a clinical culture that recognizes the importance of data. Develop clinical questions that can be answered using mobility data. Integrate mobility data into ongoing quality improvement efforts. Identify stakeholder barriers to implementing an activity and mobility project. Engage staff by increasing knowledge of functional assessment tools. Leverage the medical record for quality improvement. Facilitate activity and mobility reporting on all patients. Identify three new communication techniques that I can integrate in my standard of care to help my patients feel likepartners in health care. Correctly determine a patient’s level of readiness for change and identify an appropriate correspondingintervention.
Accreditation StatementThe Johns Hopkins University School of Medicine is accredited by the Accreditation Council forContinuing Medical Education (ACCME) to provide continuing medical education for physicians.Credit Designation StatementThe Johns Hopkins University School of Medicine designates this live activity for a maximum of 26 AMA PRA Category 1Credits . Physicians should claim only the credit commensurate with the extent of their participation in the activity.American Academy of Nurse Practitioners National Certification Program accepts AMA PRA Category 1 Credit fromorganizations accredited by the ACCME.American Nurses Credentialing Center (ANCC) accepts AMA PRA Category 1 CreditTM from organizations accredited bythe ACCME.Other CreditThe Johns Hopkins University School of Medicine is an AOTA Approved Provider of continuing education. AOTA does notendorse specific course content, products, or clinical procedures. AOTA CEUs will be provided.The Maryland Board of Social Work Examiners certifies that this program meets the criteria for 26 credit hours ofCategory 1 or 26 CEUs of continuing education for social workers licensed in Maryland. The Johns Hopkins UniversitySchool of Medicine is an approved sponsor of the Maryland Board of Social Work Examiners for continuing educationcredits for licensed social workers in Maryland.This course has been approved by the Maryland State Board of Physical Therapy Examiners for 3.7 CEUs. You will beissued a CEU certificate upon completion of the course. A record of CEUs earned will be retained by the sponsor.Physical Therapist attendees should check with their state regarding self report.Policy on Presenter and Provider DisclosureIt is the policy of the Johns Hopkins School of Medicine that the presenter and provider globally disclose conflicts ofinterest. The Johns Hopkins School of Medicine OCME has established policies that will identify and resolve conflicts ofinterest prior to this educational activity. Detailed disclosure will be made prior to presentation of the education.GENERAL INFORMATIONRegistration Includes On-demand content available (April 1, 2021 - June 1, 2021) Live content (April 21- 24, 2021) Recorded live content (April 26, 2021 - June 1, 2021)LocationA link will be provided before the activity.FeesRegistration Cut Off Date: April 20, 2021Registration On-line: http://bit.ly/RegisterNowAMPMethods of Payment: We require full payment prior to the start of the activity. The registration fee includes instructionalmaterials, on-demand and live content.The Johns Hopkins University reserves the right to cancel or postpone any activity due to unforeseen circumstances. Inthis event, the University will refund the registration fee. Under such circumstances registrants will be notified as soon aspossible.
Refund PolicyA handling fee of 25 will be deducted for cancellation. Refund requests must be received by email by April 15, 2021.No refunds will be made thereafter. Transfer of registration to another Johns Hopkins activity in lieu of cancellation is notpossible.Handouts and SyllabusThe handouts will be accessible online prior to the activity. A link to the handouts will be made available to all registrantsprior to the conference. The syllabus will be accessible online and via your mobile device in MyLearning prior to the activity.How to Obtain CreditPost activity, an online evaluation will be available to attendees to evaluate the activity and individual presentations andto identify future educational needs. Upon completion of the evaluation, the learner must attest to the number of hoursin attendance. Credits earned will be added to the learner’s transcript and immediately available for print. The last day toaccess the evaluation and attest to your credits is July 16, 2021.An outcome survey will be sent to all attendees within two months post activity to assist us in determining what impact thisactivity had on the learner’s practice.American With Disabilities ActThe Johns Hopkins School of Medicine fully complies with the legal requirements of the ADA and the rules and regulationsthereof. Please notify us if you have any special needs.Commercial SupportThe Johns Hopkins School of Medicine did not solicit or receive commercial funding from any commercial entity, includingpharmaceutical and medical device manufacturers, for this activity.
CONTENT LIBRARY: On-DemandFoundations:Moving Safely with PatientsModule 1Establishing Mobility as a Priority in the Hospital1.1. Introduction to Hospital MobilitySowmya Kumble, PT, MPT, NCS1.2 The Role of Nurse Mobility AdvocatesEleni Flanagan, DNP, MBA, RN, NEA-BC1.3 Integrating Mobility into Daily Nursing WorkflowLarissa Bell, BSN, RN, PCCNModule 2Common Language for Mobility Tools2.1. Introduction and Measuring Capacity: AM-PACSowmya Kumble, PT, MPT, NCS2.2. Measuring Performance: JH-HLMSowmya Kumble, PT, MPT, NCS2.3. Setting Daily Mobility Goals: JH-MGCSowmya Kumble, PT, MPT, NCS2.4. Balancing Mobility and Safe Patient HandlingSowmya Kumble, PT, MPT, NCSModule 3Patient Engagement3.1. Hospital Mobilization: Optimizing Patient Engagement-Part 1Nicole Schechter, PsyD3.2. Hospital Mobilization: Optimizing Patient Engagement-Part 2Nicole Schechter, PsyDModule 4Techniques for Moving Patients Safely4.1. Planning and Preparing to Move Patients SafelySowmya Kumble, PT, MPT, NCS4.2. Integrating Safe Patient Handling EquipmentSowmya Kumble, PT, MPT, NCS4.3. Video Demonstration: Bed Mobility, Transfers, andAmbulationSowmya Kumble, PT, MPT, NCSMain Conference:Functional Assessment and MeasurementModule 1Updates in AM-PAC and JH-HLM1.1. Activities of Daily Living and ValueAnnette Lavezza, OTR/LFoundations:The Johns Hopkins AMP Hospital Mobility SolutionModule 1 Rationale and Evidence for Supporting Hospital Mobility1.1. The Rationale for Developing Formal Hospital MobilityProgramsMichael Friedman, PT, MBA1.2. Designing, Conducting, & Sustaining Quality ImprovementDale Needham, MD, PhD, FCPA1.3. The Evidence Supporting Hospital MobilityErik Hoyer, MDModule 2 Common Interdisciplinary Language for Activity andMobility2.1. Functional Measurement StrategyMichael Friedman, PT, MBA2.2. JH-HLM and AM-PAC Principles and PropertiesDaniel Young, PT, DPT, PhD2.3. AM-PAC and JH-HLM ImplementationAnnette Lavezza, OTR/L2.4. JH-MGC Development and ImplementationLisa Klein, MSN, AGCNS-BC, CNRN and Erik Hoyer, MDModule 3 Clinician Workflows and Roles3.1. Data Design - From Bedside to Electronic Health RecordKelly Daley, PT, MBA3.2. The Role of NursingEleni Flanagan, DNP, MBA, RN, NEA-BC3.3. The Role of RehabilitationAnnette Lavezza, OTR/L3.4. The Physician Role in MobilityMelinda Kantsiper, MDModule 4 Barriers4.1. Administering the Patient Mobilization: Knowledge,Attitudes, and Behaviors SurveyMichelle Cvach, MS1.2. Choosing Rehabilitation WiselyCarmen Capo-Lugo, PT, PhD4.2. Assessing BarriersEleni Flanagan, DNP, MBA, RN, NEA-BC1.3. Using the AM-PAC Applied Cognitive Short Form to Screenfor Cognitive ImpairmentsKelly Casey, OTD, OTR/L, BCPR, ATP, CPAM4.3. Addressing BarriersAshley Pleiss, RN1.4. JH-HLM and AM-PAC Use in the ICUDaniel Young, PT, DPT, PhD and Stephanie Hiser, PT, DPT4.4. The Balance Between Mobility, Falls, and Safe PatientHandlingSowmya Kumble, PT, MPT, NCSModule 2Wearables and Functional Reconciliation2.1. Using Wearables to Measure In-Hospital Activity andMobilityCharles Brown, MD2.2. Longitudinal Functional MeasurementDaniel Young, PT, DPT, PhD2.3 Use of Accelerometers in Routine CareKarin Valkenet, PhD, PTModule 3Activity Mapping: Direct Observation of the Patient’s Day3.1. Physical, Cognitive and Social ActivityPrue McRae, MPH, Bphty3.2. Activity Mapping FindingsPrue McRae, MPH, Bphty3.3. Integration Information to Improve MobilityPrue McRae, MPH, Bphty4.5. Patient Engagement: Overcoming Patient RefusalsNicole Schechter, PsyDModule 5 Evaluate and Execute5.1. Sustainable Education and TrainingAshley Pleiss, RN5.2. Using Data to Drive Culture and AccountabilityMichael Friedman, PT, MBA and Erik Hoyer, MD5.3. Project Management and SustainabilityMichelle Cvach, MS5.4. Implementation Tools and ResourcesMichael Friedman, PT, MBA
CONTENT LIBRARY: On-DemandMain Conference:Interdisciplinary Clinical ProgramsModule 1Eat, Walk Engage: Australia (Part 1)1.1. Why are Older People at Risk of Hospital-AcquiredHarm?Alison Mudge, PhD, FRACP1.2 What are the Common Forms of Harm for Older Peoplein the Hospital?Alison Mudge, PhD, FRACP1.3 How Can We Improve Hospital Care for Older People?Alison Mudge, PhD, FRACPModule 2Eat, Walk Engage: Australia (Part 2)2.1. Engaging Older People in Improving Mobility:Partnering with PatientsPrue McRae, MPH, Bphty2.2. Engaging Older People In Improving Mobility: What doOlder People Say About Mobility?Prue McRae, MPH, BphtyModule 3End PJ Paralysis: Canada3.1. End PJ Paralysis: Say Goodnight to Hospital Gowns,Get Up, Get Dressed, Get MovingPaul Wright, RN, BScN, CNNC3.2. Designing, Engaging, and Tri-Storming: Our Approachto End PJ Paralysis in Calgary, Alberta, CanadaPaul Wright, RN, BScN, CNNC3.3 So What, Now What: Capturing Key Learnings forFidelity and Next Steps to End PJ ParalysisPaul Wright, RN, BScN, CNNCModule 4Hospital Programs: United States4.1. Geisinger System Wide Mobility and Home FirstDischarge Efforts: A Multidisciplinary ApproachMichael DiMare, PT, DPT, GCS, MSOM and LaurenMurphy, DNP, RN, ACNS-BC4.2. Nurse Driven AM-PAC “6 clicks” Mobility Plan of CareCharlie Workman, MSPT, MBA; Kathy Tussey, MSN, RN,NEA-BC; Emily Sacca, PT, DPT4.3. Pediatric AMP Step 1: Establishing a SharedInterprofessional Common LanguageSapna Kudchadkar, MD, PhD and Katherine Denlinger, PT,DPT, PCSModule 5Geriatric Surgical Pathways: United States5.1. Mobility within the Enhanced Recovery After Surgery(ERAS) FrameworkGina Vickery, BSN, RNMain Conference:Establishing a Culture of Mobility at the Front LinesModule 1Balancing Falls, Mobility, and Safe Patient Handling1.1. Fall Prevention: Myths and RealitiesYuri Agrawal, MD, MPH, FACS1.2 The Tension Between Mobility and FallsSowmya Kumble, PT, MPT, NCS and Holley Farley, BSN, RN1.3 Role of Mobility in Fall AssessmentErik Hoyer, MD1.4 The Impact of Fall Risk Assessment on Patient MobilityCarmen Capo-Lugo, PT, PhD1.5 Safe Patient Handling and Employee InjuryAnita Stone, MS, CSPHAModule 2Proactive Discharge Planning through Prediction Models2.1. The Value of Early Discharge Disposition PredictionMelissa Richardson, MBA2.2. Development of a True Prediction ToolDaniel Young, PT, DPT, PhD2.3. Translating Prediction Tools into PracticeMichael Friedman, PT, MBAModule 3Value-based Hospital Rehabilitation Delivery of Care Model3.1. Value and WasteMichael Friedman, PT, MBA3.2. Rehabilitation Model DevelopmentAnnette Lavezza, OTR/L3.3 Rehabilitation Model DeploymentAnnette Lavezza, OTR/L3.4 Opportunities and ChallengesMichael Friedman, PT, MBAModule 4Nursing Best Practices at the Bedside4.1. It's a Marathon, not a Sprint Engaging Patients in PostOperative MobilityStacey Danielczyk, MS, RN; Kalli Veldman, MSN, RN; SamanthaBabiarz, ADN, RN; and Josie Leal, BSN, RN4.2. Nursing Best Practices at the Bedside: The Neurosurgery andNeurology PopulationLisa Klein, MSN, AGCNS-BC, CNRN; Tenise Shakes, MSN, RN,CNRN; Diana Sanchez, BSN, RN; Saundra Roberts, RN; ShirleyAnsari, BSN, RN, CNRN; Nozomi Tahara, BSN, RN, CNRN4.3 The AMP Journey in MedicineAshley Pleiss, RN, BS; Shelby Cahill, BSN, RN; Danielle Balsano,BSN, RN; Alphonsa Rahman, DNP, APRN, CNS, CCRN4.4 Balancing Falls and MobilityHolley Farley, BSN, RNModule 5Training and Awareness5.2. Frailty and Risk StratificationSusan Gearhart, MD5.1 everyBODYmoves Awareness CampaignMichelle Cvach, MS5.3. Integrating Mobility into PracticeJessica Peters, BSN, RN5.2 Mobility Trainer Certificate ApproachSowmya Kumble, PT, MPT, NCSModule 6Environment-Life/Space Design: Netherlands6.1. Hospital in MotionLotte van Delft, PT, MS6.2. Reactivate: Stimulating Environment for Patients DuringHospital AdmissionJordi Elings, PT, PhD
SCHEDULE OF LIVE CONTENTMoving Safely With PatientsWednesday, April 21, 2021Welcome and Opening Remarks8:00 AM-8:10 AMSession 1Social Media PrimerSapna Kudchadkar, MD, PhDEstablishing Mobility as a Priority in the Hospital8:10 AM-8:25 AMIntroduction to Hospital MobilitySowmya Kumble, PT, MPT, NCS8:25 AM-8:30 AMThe Role of Nurse Mobility AdvocatesEleni Flanagan, DNP, MBA, RN, NEA-BC8:30 AM-8:55 AMIntegrating Mobility into Daily Nursing WorkflowLarissa Bell, BSN, RN, PCCN8:55 AM-9:05 AMBreakSession 2Common Language for Mobility Tools9:05 AM-9:50 AMIntroduction and Measuring Capacity: AM-PACSowmya Kumble, PT, MPT, NCS9:50 AM-10:00 AMMeasuring Performance: JH-HLMSowmya Kumble, PT, MPT, NCS10:00 AM-10:10 AMSetting Daily Mobility Goals: JH-MGCSowmya Kumble, PT, MPT, NCS10:10 AM-10:35 AMBalancing Mobility and Safe Patient HandlingSowmya Kumble, PT, MPT, NCS10:35 AM-10:55 AMCases and QuestionsSowmya Kumble, PT, MPT, NCS10:55 AM-11:05 AMBreakSession 3Patient Engagement11:05 AM-11:35 AMHospital Mobilization: Optimizing Patient Engagement-Part 1Nicole Schechter, PsyD11:35 AM-12:05 PMHospital Mobilization: Optimizing Patient Engagement-Part 2Nicole Schechter, PsyD12:05 AM-12:40 PMBreakSession 4Techniques for Moving Patients Safely12:40 PM-1:00 PMPlanning and Preparing to Move Patients SafelySowmya Kumble, PT, MPT, NCS1:00 PM-1:20 PMIntegrating Safe Patient Handling EquipmentSowmya Kumble, PT, MPT, NCS1:20 PM-1:45 PMVideo Demonstration: Bed Mobility, Transfers, and AmbulationSowmya Kumble, PT, MPT, NCS1:45 PM-1:55 PMBreakSession 5Interactive Workshop: What Would You Do?1:55 PM-2:15 PMTechniques for Moving Patients SafelySowmya Kumble, PT, MPT, NCS and Nicole Schechter, PsyD2:15 PM-2:35 PMRole of Mobility Advocates: Practical ScenariosSowmya Kumble, PT, MPT, NCS and Nicole Schechter, PsyD2:35 PM-2:45 PMDaily Close
SCHEDULE OF LIVE CONTENTThe Johns Hopkins AMP Hospital Mobility SolutionThursday, April 22, 2021Welcome and Opening Remarks8:00 AM-8:10 AMSocial Media PrimerSapna Kudchadkar, MD, PhD8:10 AM-8:15 AMWelcomeMichael Friedman, PT, MBASession 1 The Johns Hopkins AMP Hospital Immobility Harm Solution8:15 AM-8:30 AMIntroduction and Project ComponentsMichael Friedman, PT, MBA8:30 AM-8:45 AMCommon Interdisciplinary Language of Mobility: JH-HLM, AM-PAC, Mobility Goal Calculator (JH-MGC)Michael Friedman, PT, MBA8:45 AM-9:00 AMBarriers and Multi-Disciplinary RolesMichael Friedman, PT, MBA9:00 AM-9:15 AMEducate, Engage, Evaluate, ExecuteMichael Friedman, PT, MBA9:15 AM-9:25 AMBreakDesign Workshop Project Charter and Timeline9:25 AM- 10:15 AM Implementation Tools, Resources, and DiscussionMichael Friedman, PT, MBA10:15 AM - 10:25 AM BreakSession 2 Common Interdisciplinary Language for Activity and Mobility10:25 AM - 10:40 AM Functional Measurement StrategyMichael Friedman, PT, MBA10:40 AM - 11:10 AM JH-HLM and AM-PAC Principles and PropertiesDaniel Young, PT, DPT, PhD11:10 AM - 11:30 AM AM-PAC and JH-HLM ImplementationAnnette Lavezza, OTR/L11:30 AM - 11:55 AM JH-MGC Development and ImplementationLisa Klein, MSN, AGCNS-BC, CNRN and Erik Hoyer, MD11:55 AM - 12:10 PM Using Data to Drive Culture and AccountabilityMichael Friedman, PT, MBA and Erik Hoyer, MD12:10 PM -1:00 PMLunchDesign Workshop Common Interdisciplinary Language for Activity and Mobility1:00 PM-1:50 PM-1:50 PMImplementation Tools, Resources, and DiscussionMichael Friedman, PT, MBA; Daniel Young PT, DPT, PhD; Annette Lavezza, OTR/L; Erik Hoyer, MD; and Lisa Klein, MSN, AGCNS-BC, CNRN2:00 PMBreakSession 3 Assessing Barriers and Developing an Education Plan2:00 PM-2:10 PMAdministering the Patient Mobilization: Knowledge, Attitudes, and Behaviors SurveyMichelle Cvach, MS2:10 PM-2:25 PMAssessing BarriersEleni Flanagan, DNP, MBA, RN, NEA-BC2:25 PM-2:40 PMAddressing BarriersAshley Pleiss, RN, BS2:40 PM-3:00 PMSustainable Education and TrainingAshley Pleiss, RN, BS3:00 PM-3:10 PMBreakDesign Workshop Assessing Barriers and Developing an Education Plan3:10 PM-4:00 PM-4:00 PMImplementation Tools, Resources, and DiscussionMichelle Cvach, MS; Eleni Flanagan, DNP, MBA, RN, NEA-BC; and Ashley Pleiss, BS, RN4:10 PMBreakSession 4 Implementing and Expanding Johns Hopkins Activity and Mobility Promotion4:10 PM-4:30 PMGeisinger System Wide Mobility and Home First Discharge Efforts: A Multidisciplinary ApproachMichael DiMare, PT, DPT, GCS, MSOM and Lauren Murphy, DNP, RN, ACNS-BC4:30 PM-5:00 PMNurse Driven AM-PAC “6 clicks” Mobility Plan of CareCharlie Workman, MSPT, MBA; Kathy Tussey, MSN, RN, NEA-BC; Emily Sacca, PT, DPT5:00 PM-5:20 PMPediatric AMP Step 1: Establishing a Shared Interprofessional Common LanguageSapna Kudchadkar, MD, PhD and Katherine Denlinger, PT, DPT, PCS5:20 PM-5:50 PMQ&AMichael DiMare, PT, DPT, GCS, MSOM; Lauren Murphy, DNP, RN, ACNS-BC; Charlie Workman, MSPT, MBA; Kathy Tussey, MSN, RN, NEABC; Emily Sacca, PT, DPT; Sapna Kudchadkar, MD, PhD; and Katherine Denlinger, PT, DPT, PCS5:50 PM-6:00 PMDaily Close
SCHEDULE OF LIVE CONTENTMain ConferenceFriday, April 23, 2021Welcome and Opening Remarks9:00 AM-9:10 AMSocial Media PrimerSapna Kudchadkar, MD, PhD9:10 AM-9:15 AMWelcomeMichael Friedman, PT, MBASession 1Updates in AM-PAC and JH-HLM9:15 AM-9:25 AMActivities of Daily Living and ValueAnnette Lavezza, OTR/L9:25 AM-9:40 AMChoosing Rehabilitation WiselyCarmen Capo-Lugo, PT, PhD9:40 AM-9:55 AMUsing the AM-PAC Applied Cognitive Short Form to Screen for Cognitive ImpairmentsKelly Casey, OTD, OTR/L, BCPR, ATP, CPAM9:55 AM- 10:25 AMJH-HLM and AM-PAC Use in the ICUDaniel Young, PT, DPT, PhD and Stephanie Hiser, PT, DPT10:25 AM- 10:55 AMQ&AAnnette Lavezza, OTR/L; Carmen Capo-Lugo, PT, PhD; Kelly Casey, OTD, OTR/L, BCPR, ATP, CPAM; Daniel Young, PT, DPT,PhD; and Stephanie Hiser, PT, DPT10:55 AM- 11:05 AMBreak11:05 AM- 11:25 AMHospital in MotionLotte van Delft, PT, MS11:25 AM- 11:40 AMReactivate: Stimulating Environment for Patients During Hospital AdmissionJordi Elings, PT, PhD11:40 AM- 12:05 PMQ&ALotte van Delft, PT, MS; Jordi Elings, PT, PhD12:05 PM- 12:55 PMLunchSession 2Session 3Hospital in MotionNursing Best Practices at the Bedside12:55 PM-1:10 PMThe AMP Journey in MedicineEleni Flanagan, DNP, MBA, RN, NEA-BC1:10 PM-1:25 PMIt's a Marathon, not a Sprint Mobility Best Practices in the Department of Surgical NursingStacey Danielczyk, MS, RN1:25 PM-1:40 PMNeurosurgery and Neurology PopulationLisa Klein, MSN, AGCNS-BC, CNRN1:40 PM-1:50 PMBreakWorkshopNursing Best Practices at the Bedside1:50 PM-2:35 PMDiscussionEleni Flanagan, DNP, MBA, RN, NEA-BC; Stacey Danielczyk, MS, RN; Lisa Klein, MSN, AGCNS-BC, CNRN, Josie Leal, BSN, RN2:35 PM-2:45 PMBreak2:45 PM-3:30 PMEnd PJ Paralysis: CanadaPaul Wright, RN, BScN, CNNC3:30 PM-3:50 PMThe Geriatric Surgery Program: Improving Outcomes for our Older PatientsSusan Gearhart, MD3:50 PM-4:10 PMEat, Walk, EngagePrue McRae, M Phil, Bphty4:10 PM-4:20 PMBreakSession 4WorkshopEngaging the Older Adult in MobilityEngaging the Older Adult in Mobility4:20 PM-5:00 PMDiscussionPaul Wright, RN, BScN, CNNC; Susan Gearhart, MD; Prue McRae, M Phil, Bphty5:00 PM-5:10 PMBreak5:10 PM-5:50 PMDiscussionCharles Brown, MD; Prue McRae, MPH, Bphty; Karin Valkenet, PhD, PT; and Erik Hoyer, MD5:50 PM-6:00 PMDaily CloseWorkshopPrecision Measurement, Behavioral Mapping, and Observation
SCHEDULE OF LIVE CONTENTMain ConferenceSaturday, April 24, 2021Welcome and Opening Remarks8:00 AM-8:10 AMSocial Media PrimerSapna Kudchadkar, MD, PhD8:10 AM-8:15 AMWelcomeMichael Friedman, PT, MBASession 1Balancing Falls, Mobility, and Safe Patient Handling8:15 AM-8:35 AMFall Prevention: Myths and RealitiesYuri Agrawal, MD, MPH, FACS8:35 AM-8:55 AMThe Tension Between Mobility and FallsSowmya Kumble, PT, MPT, NCS and Holley Farley, BSN, RN8:55 AM-9:05 AMRole of Mobility in Fall Risk AssessmentErik Hoyer, MD9:05 AM-9:20 AMThe Impact of Fall Risk Assessment on Patient MobilityCarmen Capo-Lugo9:20 AM-9:35 AMSafe Patient Handling and Employee InjuryAnita Stone, MS, CSPHA9:35 AM- 10:05 AMQ&AYuri Agrawal, MD, MPH, FACS; Sowmya Kumble, PT, MPT, NCS; Holley Farley, BSN, RN; Erik Hoyer, MD; Carmen Capo-Lugo;and Anita Stone, MS, CSPHA10:05 AM- 10:15 AMBreakSession 2Value-based Hospital Rehabilitation Delivery of Care Model10:15 AM- 10:30 AMValue and WasteMichael Friedman, PT, MBA10:30 AM- 10:45 AMRehabilitation Model DevelopmentAnnette Lavezza, OTR/L10:45 AM- 11:00 AMRehabilitation Model DeploymentAnnette Lavezza, OTR/L11:00 AM- 11:15 AMOpportunities and ChallengesMichael Friedman, PT, MBA11:15 AM- 11:25 AMBreakWorkshopValue-based Hospital Rehabilitation Delivery of Care Model11:25 AM- 12:15 PMDiscussionAnnette Lavezza, OTR/L and Michael Friedman, PT, MBA12:15 PM-Lunch1:15 PMSession 3Best Practices at the Bedside (Part 2)1:30 PMThe Physician Role in MobilityMelinda Kantsiper, MD1:30 PM1:50 PMPatient Engagement: Overcoming Patient RefusalsNicole Schechter, PsyD1:50 PM2:00 PMBalancing Falls and MobilityHolley Farley, BSN, RN2:00 PM2:15 PMCardiac Critical Care UnitDanielle Balsano, BSN, RN2:25 PMBreak1:15 PM2:15 PM--WorkshopBest Practices at the Bedside (Part 2)2:25 PM-3:15 PMDiscussionMelinda Kantsiper, MD; Nicole Schechter, PsyD; Holley Farley, BSN, RN; Danielle Balsano, BSN, RN3:15 PM-3:25 PMBreak3:25 PM-3:55 PMTools, Resources, and DiscussionMichael Friedman, PT, MBA; Annette Lavezza, OTR/L; and Eleni Flanagan, DNP, MBA, RN, NEA-BC3:55 PM-4:05 PMConference CloseWorkshopJohns Hopkins Activity and Mobility Promotion Tools and Resources
ACTIVITY DIRECTORMichael Friedman, PT, MBADirector of Strategic Program DevelopmentPhysical Medicine and RehabilitationJohns Hopkins MedicinePLANNING COMMITTEEMichelle Cvach, MSOperations Project LeadJohns Hopkins Health SystemAnnette Lavezza, OTR/LTherapy Manager Acute CareTherapy Consult ServicesThe Johns Hopkins HospitalHolly Russell, MS, OTR/LRehabilitation Team LeaderJohns Hopkins MedicineJOHNS HOPKINS SPEAKERSYuri Agrawal, MD, MPH, FACSProfessorShirley Ansari, BSN, RN, CNRNStaff Nurse IIISamantha Babiarz, ADN, RNStaff Nurse – RN IIDanielle Balsano, BSN, RNStaff Nurse – RN IILarissa Bell, BSN, RN, PCCNLead Clinical NurseCharles Brown, MDAssociate ProfessorShelby Cahill, BSN, RNLead Clinical NurseCarmen Capo-Lugo, PT, PhDAssistant ProfessorKelly Casey, OTD, OTR/L, BCPR,ATP, CPAMOccupational TherapistMichelle Cvach, MSProject AnalystKelly Daley, PT, MBAProgram Coordinator ClinicalInformaticsEleni Flanagan, DNP, MBA, RN,NEABCAssistant Director of NursingAlphonsa Rahman, DNP, APRN,CNS, CCRNClinical Nurse SpecialistSusan Gearhart, MDAssociate Professor of SurgeryMelissa Richardson, MBAVice President, Care Coordination &Clinical Resource ManagementStephanie Hiser, PT, DPTJHU Research FellowErik Hoyer, MDAssistant ProfessorMelinda Kantsiper, MDAssistant ProfessorLisa Klein, MSN, AGCNS-BC,CNRNClinical Nurse SpecialistSapna Kudchadkar, MD, PhDAssociate ProfessorSowmya Kumble, PT, MPT, NCSClinical Recourse AnalystAnnette Lavezza, OTR/LInpatients Rehabilitation ManagerJosie Leal, BSN, RNLead Clinical NurseDale Needham, MD, PhD, FCPAProfessorStacey Danielczyk, MS, RNNurse EducatorJessica Peters, BSN, RNSenior Clinical NurseHolley Farley, BSN, RNCoordinator FU Nursing ProgramAshley Pleiss, RNLead Clinical NurseSaundra Roberts, RNStaff Nurse – RN IIDiana Sanchez, BSN, RNStaff Nurse – RN IINicole Schechter, PsyDAssistant ProfessorTenise Shakes, MSN, RN,CNRNNurse ManagerAnita Stone, MS, CSPHAAssociate Director of Health, Safety,and EnvironmentNozomi Tahara, BSN, RN, CNRNStaff Nurse – RN IIIKalli Veldman, MSN, RNStaff Nurse – RN IIGina Vickery, BSN, RNStaff Nurse – RN IIIDaniel Young, PT, DPT, PhDAssociate Professor
GUEST SPEAKERSKatherine Denlinger, PT, DPT,PCSPhysical TherapistCertified Clinical SpecialistAnn & Robert H. Lurie Children’sHospitalChicago, IllinoiMichael DiMare, PT, DPT,GCS, MSOMOperations ManagerRehabilitation ServicesGeisinger Wyoming Valley andGeisingerSouth Wilkes Barre, Scranton,PennsylvaniaPrue McRae, MPH, BphtyPhysiotherapistStatewide Program ManagerEat Walk Engage ProgramAustraliaAlison Mudge, PhD, FRACPProfessorRoyal Brisbane and Women’sHospitalQueensland HealthAustraliaLauren Murphy, DNP, RN,ACNS-BCNursing Quality Improvement andResearch SpecialistGeisinger Wyoming Valley andGeisinger Community MedicalCentersWilkes Barre, PennsylvaniaEmily Sacca, PT, DPTPhysical TherapistAssistant Director Baptist HealthLexington, KentuckyKathy Tussey, MSN, RNExecutive Director ofAdministrative ServicesBaptist HealthLexington, KentuckyKarin Valkenet, PhD, PTSenior ResearcherDepartment of RehabilitationUniversity Medical CentreUtrecht, the NetherlandsLotte van Delft, PT, MSPhysiotherapistUniversity Medical CentreUtrecht, the NetherlandsCharlie Workman, MSPT, MBAExecutive DirectorBaptist Health LexingtonWilmore, KentuckyPaul Wright, RN, BScN, CNNCRegistered NurseCalgary, AlbertaJordi Elings, PT, PhDPhysical TherapistRegional HospitalOrthopedic Departmentthe Netherlands
The Maryland Board of Social Work Examiners certifies that this program meets the criteria for 26 credit hours of . DNP, MBA, RN, NEA-BC 3.3. The Role of Rehabilitation Annette Lavezza, OTR/L 3.4. . Module 4 Hospital Programs: United States Michael Friedman, PT, MBA 4.1. Geisinger System Wide Mobility and Home First