Transcription
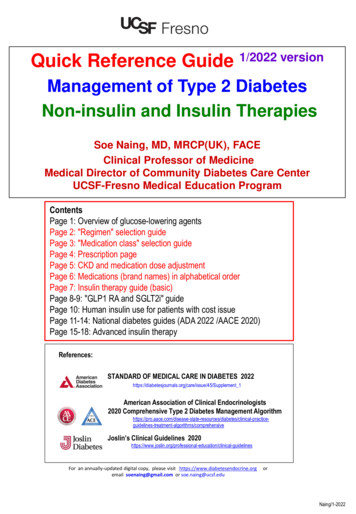
Quick Reference Guide 1/2022 versionManagement of Type 2 DiabetesNon-insulin and Insulin TherapiesSoe Naing, MD, MRCP(UK), FACEClinical Professor of MedicineMedical Director of Community Diabetes Care CenterUCSF-Fresno Medical Education ProgramContentsPage 1: Overview of glucose-lowering agentsPage 2: "Regimen" selection guidePage 3: "Medication class" selection guidePage 4: Prescription pagePage 5: CKD and medication dose adjustmentPage 6: Medications (brand names) in alphabetical orderPage 7: Insulin therapy guide (basic)Page 8-9: "GLP1 RA and SGLT2i" guidePage 10: Human insulin use for patients with cost issuePage 11-14: National diabetes guides (ADA 2022 /AACE 2020)Page 15-18: Advanced insulin therapyReferences:STANDARD OF MEDICAL CARE IN DIABETES plement 1American Association of Clinical Endocrinologists2020 Comprehensive Type 2 Diabetes Management -algorithms/comprehensiveJoslin’s Clinical Guidelines clinical-guidelinesFor an annually-updated digital copy, please visit https://www.diabetesendocrine.orgemail soenaing@gmail.com or soe.naing@ucsf.eduorNaing/1-2022
1Naing/1-2022
2Naing/1-2022
3Comparison of Glucose-Lowering Medications # 1Consider the factors in first column, that will impact the class selection.4 Major groups9 Classes(of 12 total)Insulin ioglitazone)3 classes (Amylin Mimetics, Bile Acid Sequestrant, Dopamine-2 Agonist) are not included in this table.Insulin ProvidersInsulin secretagoguesSulfonylureaNaing/1-2022Use this table to choose a class of medicationGLP1-based therapyInsulinDPP4InhibitorsGlinidesGlucose Absorption InhibitorGLP-1 ReceptorAgonistsSGLT2 Inhibitorsα GlucosidaseInhibitorsCostLowLowLowModerateLow - human insulinHigh - Analog insulinHighHighHighModerateHYPOglycemia risk NoNoYesYesYesNoNoNoNoWeight ChangeLoss GainGainGainGainNeutralLoss Potency:Sema Lira Dula ExenaLoss NeutralCV effect ifPotential benefitPotential benefitNeutralNeutralNeutralNeutralPreferred add-on ormono therapy Sema-,Dula- or Lira-glutide all SubQ , See page 8-9Preferred add-on or monotherapyEmpa- or Cana-gliflozinNeutralPreferred therapy ifSGLT2i contraindicatedSema-, Dula- or Liraglutide - all SubQ1st choice - preferred addon or mono therapy ifeGFR is adequate.Empa-,Cana- or Dapagliflozin See page 8-9 for detailNeutral1st choice - preferred addon or mono therapy ifeGFR is adequate.Empa-,Cana- or Dapagliflozin- See page 8-9Avoid if eGFR 30ASCVD or highrisk for ASCVDCV effect ifNeutral CHF riskNeutralNeutral CHF Risk withSaxagliptinCHF See page 8-9 for detailCKD (see page 5 fordetails)Contraindicated ifeGFR 30Do not start or toreduce currentdose if eGFR 45.No dose adjustmentneeded. risk of fluidretention .Avoid Glyburide(See page 5 for details)Repaglinidecan be used inadvancedCKD/ESRD.Lower doses requiredif eGFR Linagliptin – noneed to adjust dose.Others – to reducedose.Preferred therapy ifSGLT2i contraindicated.Sema-, Dula- or Liraglutide - all SubQSee page 8-9 for detailSee page 8-9 for detailSee page 5 for dosing based on eGFRHigh ( -1 to 2%)FBG PPBG High (-1 to 1.5%)FBG PPBG High (-1 to 2%)FBG PPBG High (-1 to 1.5%)FBG PPBG Highest (no ceiling)IntermediateHigh (-0.9 to 1.5%)Intermediate (-0.5-1.0%)Low (-0.5%)Basal: FBG PPBG Prandial: FBG PPBG (-0.5 to 0.8%)FBG PPBG FBG PPBG eGFR dependentFBG PPBG FBG PPBG RouteOralOralOralOralSQOralSQ /Oral (Semaglutide)OralOralOther benefitsExtensiveexperienceDurability, HDLExtensiveexperience Postmealglucose excursionUniversalResponseWell tolerated Postmeal glucoseexcursion BP Postmealglucose excursionOther risksB12 Nausea/DiarrheaLactic acidosisEdema/fluid retentionWeight gainHigh rate ofsecondaryfailureWeight gainFrequent dosingWeight gainAngioedemaUrticaria? Pancreatitis? Arthralgia? Bullous pemphigoidNausea, Vomiting Heart rate? PancreatitisMedullary thyroid cancerin animalsDKA, GU tract infection K, LDL, Cr (brief)Hypotension, DehydrationFournier gangrene risk of fractur withCanagliflozinFlatulenceDiarrheaFrequent dosingContraindicationseGFR 30AcidosisHypoxiaDehydrationNYHA III/IV heartfailureUse with caution inpatients with a h/opancreatitis.PMH or FH ofMEN2/Medullary thyroidcancerCaution in h/o pancreatitisor gastroparesis.eGFR 20 for Empagliflozin, 25 for Dapagliflozin, 30 forCanagliflozin, 45 forErtugliflozinCirrhosisEfficacy ( A1c)Effect on Fasting orPost-Prandial BGBenefit in NASH Fracture risk? Bladder cancer? Macular edemaTakes 2-4 weeks forfull benefitActive bladder cancerHepatic impairmentSevere renal orhepaticimpairmentInflammatorybowel diseaseIntestinalobstruction.
Naing/1-2022Comparison of Glucose-Lowering Medications # 2Use this table to prescribe a medication from the class chosen in previous table4 Major groups9 ClassesInsulin SensitizersBiguanideThiazolidinedione(of 12 nd tazone(Actos)Minimum –Maximum dose&DosingFrequency500mg qd1000 mg bid,poActos15-45 mg qd,poAvailablestrengthInsulin ProvidersInsulin secretagoguesSulfonylureaGLP1-based Repaglinide(Prandin),Nateglinide(Starlix)Meal insulin:Glipizide2.5-20 mgbid/ac, poGlimeperide1- 8 mg qamGlyburidePrandin0.5-4 mgtid/ac, poStarlix60-120 mgtid/ac, poNo maximumdoseAnalog or HumaninsulinBasal insulin:Analog or Humaninsulin1.25-20mgqam, po500, 850,1000 mgActos15, 30,45 mgGlipizide5, 10 mgGlimeperide1, 2, 4 mgGlyburide1.25, 2.5, 5mgDPP4InhibitorsMost Pens(U-100):3ml (300 Units)Vial:10ml (1000 Units)GLP-1 Receptor Agonists4Glucose Absorption InhibitorSGLT2 Inhibitorsα GlucosidaseInhibitorsSitagliptin (Januvia)Saxagliptin (Onglyza)Linagliptin (Trajenta)Alogliptin (Nesina)Semaglutide (Ozempic)Dulaglutide (Trulicity)Exenatide (Bydureon Bcise)Liraglutide (Victoza)Others:Semaglutide oral (Rybelsus)Lixisenatide (Adlyxin)Empagliflozin (Jardiance)Dapagliflozin (Farxiga)Canagliflozin (Invokana)Ertugliflozin (Steglatro)AcarboseJanuviaOzempic 0.25-1.0 mg qw, SubQTrulicity 0.75-4.5mg qw, SubQBydureon Bcise 2 mg qw, SubQVictoza 0.6-1.8 mg qam, SubQOthers:Rybelsus 3, 7 or 14 mg qam, POAdlyxin 10-20mcg qam, SubQJardiance 10-25 mg qam, poFarxiga 5-10 mg qam, poInvokana 100-300 mg qam, poSteglatro 5-15 mg qam, poPrecose orGlycet25-100 mgtid/ac, poOzempic 0.25/0.5, 1.0 mg penTrulicity 0.75, 1.5, 3.0, 4.5 mg penBydureon Bcise 2mgVictoza 0.6, 1.2, 1.8 mg penOthers:Rybelsus 3, 7 or 14 mg tabletAdlyxin 10, 20mcg penJardiance 10, 25 mgFarxiga 5, 10 mgInvokana 100, 300 mgSteglatro 5, 15mgPrecose orGlycet25,50,100 mg25-100 mg qam, poOnglyza2.5-5 mg qam, poTradjenta5 mg qam, poNesina6.25-25mg qam, poPrandin0.5, 1, 2 mgStarlix60,120 mg3 classes (Amylin Mimetics, Bile Acid Sequestrant, Dopamine-2 Agonist) are not included in this table.Januvia25,50,100 mgOnglyza2.5, 5 mgTradjenta5 mgNesina(Precose),Miglitol(Glyset)6.25,12.5,25 mgCombinationMetformin & TZD can be nsWITH ACTOS:Actoplus Met XR(Actos Metformin)15/1000, 30/1000mg, qam (XR)15/500, 15/850 mg, bid (generic)Duetact (Actos Amaryl)30/2, 30/4 mg, qamOseni (Nesina Actos)25/15, 25/30 or 25/45 mg, qamDo not use Sulfonylurea &Glinides together.Do not use mealinsulin & insulinsecretagoguestogether.Do not use DPP4 inhibitors & GLP1 RA together.WITH DPP4 inhibitor:JanuMet XR (Januvia Metformin)50/500, 50/1000, 100/1000 mg, qamKombiglyze XR(Onglyza Metformin)2.5/1000, 5/500, 5/1000 mg, qamKazano (Nesina Metformin)12.5/500, 12.5/1000 mg, bidOseni (Nesina Actos)25/15, 25/30 or 25/45 mg, qamJentadueto (Tradjenta Metformin)2.5/500, 2.5/850, 2.5/1000 mg, bidWITH a basal insulin:XultophyDegludec (Tresiba) liraglutide(Victoza)Soliquaglargine (Lantus) lixisenatide(Adlyxin)WITH SGLT2 inhibitor:Synjardy XR (Jardiance Metformin)5 or 10 or 12.5 or 25/1000 mg, qamGlyxambi (Jardiance Tradjenta) 10/5, 25/5 mg, qamTrijardy XR (Jardiance Trajenda Metformin)5/2.5/1000, 10/5/1000, 25/5/1000 mg, qamInvokamet XR (Invokana Metformin)50/500, 150/500, 50/1000 or 150/1000 mg, qamXigduo XR (Farxiga Metformin)2.5/1000, 5/500, 5/1000, 10/500 or 10/1000 mg, qamQtern (Farxiga Onglyza) 5/5, 10/5 mg qamSegluromet (Steglatro Metformin)2.5/500, 2.5/1000, 7.5/500 or 7.5/1000 mg, bidSteglujan (Steglatro Januvia) 5/100 or 15/100 mg, qam
5Naing/1-2022
6Naing/1-2022
7Step 1Management of Type 2 Diabetes : Guide for Insulin Initiation and TitrationInsulin regimensStarting doseOne injection dailywith a basal insulinBasal insulin therapy:Start 0.2 Unit/kg body weightor 10 units QHS.To cont’ metformin, GLP1 RA othernon-insulin agents(Lantus/Toujeo/Basaglar, Levemir, Tresiba or NPH)Basal 1 regimen:Add one dose of prandial insulinbefore main meal of the day.Step 2Two injections dailywith Basal 1 regimen orPre-mixed insulinTo cont’ metformin. Considerstopping other non-insulin agents.Start 0.1 U/kg, 4 units or 10% of current basal dose.Pre-mixed insulin therapy:Change basal insulin to pre-mixed insulin bid/ac.Divide current basal dose into ½ AM ½ PM or ⅔AM ⅓ PM orStart 0.5 U/kg in 2 divided doses.For patients on basal insulin or basal 1 regimen:Add prandial insulin before each meal or tid/ac.Start 0.1 U/kg, 4 units or 10% basal dose per mealMultiple injections dailywith Basal Prandial TherapyTo cont’ metformin. Considerstopping other non-insulin agents.Patients may adjust the dose by 1 unit every night orby 2-3 units or 10-15% every 3 nights until targetfasting BG of 80-130 mg/dl is achieved.Consider adding prandial insulin if A1c is not at goalthough the patient has been taking at least 0.5 unit/kgof basal insulin or fasting BG has been at goal.Patients may adjust the prandial insulin doseby 1 unit every day or by 2 units or 10-15% every 3days until 1-2 hours post-meal BG of 100-160 or nextpre-meal BG of 80-130 is achieved.(Novolog, Fiasp, Humalog, Admelog, Lyumjev, Apidra , HumuLIN R, NovoLIN R)(Novolog 70/30, Humalog 75/25 or human insulin 70/30)Step 3TitrationFor patients on Pre-mixed insulin therapy:Use 80% of current total daily dose and give50% as basal insulin 50% as prandial insulin in 3divided doses.For insulin-naïve patients:Start total daily insulin dose of 0.5 U/kg and give 50% asbasal insulin 50% as prandial insulin in 3 divided doses. ORStart basal insulin 0.2 U/kg prandial insulin 0.1 U/kg tid/acBreakfast dose:Patients may adjust the dose by 1 unit every day orby 2 units or 10-15% every 3 daysuntil pre-dinner BG of 80-130 mg/dl is achieved.Dinner dose:Patients may adjust the dose by 1 unit every day orby 2 units or 10-15% every 3 daysuntil fasting BG of 80-130 mg/dl and/or bed-time BG of130-180 mg/dl is achieved.Consider giving pre-mixed insulin tid/ac if bid/ac fails.Patients may adjust the prandial insulin dose by 1 unitevery day or by 2 units or 10-15% every 3 daysuntil 1-2 hours post-meal BG of 100-160 mg/dl or nextpre-meal BG of 80-130 mg/dl is achieved. Once insulin is initiated, the physician should readjust thedose by 10-20% every 1-2 weeks and/or advise the patientto self-titrate the dose until BG targets are met. For hypoglycemia, determine the cause and reduce thecorresponding dose by at least 10-20%.Naing/1-2022
Guidance for managing ASCVD, HF, and DKD Risk in patients with T2DM using SGLT2 inhibitors and GLP-1RAs # 18See next page - page # 9 for detailsFigure 1, 2, 32020 Expert Consensus Decision Pathway on Novel Therapies for Cardiovascular Risk Reduction in Patients With Type 2 Diabetes:A Report of the American College of Cardiology Solution Set Oversight CommitteeJ Am Coll Cardiol. 2020 Sep, 76 (9) 1117–1145. 05.037Naing/1-2022
9Guidance for managing ASCVD, HF, and DKD Risk in patients with T2DM using SGLT2 inhibitors and GLP-1RAs # 2(AMI, stroke, or cardiovascular death)*Contraindication: eGFR 20 mL/minute/1.73m2 for Empagliflozin, eGFR 25 for Dapagliflozin, eGFR 30 for Canagliflozin, eGFR 45 for ErtugliflozinTable 62020 Expert Consensus Decision Pathway on Novel Therapies for Cardiovascular Risk Reduction in Patients With Type 2 Diabetes:A Report of the American College of Cardiology Solution Set Oversight CommitteeJ Am Coll Cardiol. 2020 Sep, 76 (9) 1117–1145. 05.037Naing/1-2022
Using Human insulin in patients with cost issue10Insulin RxStart with a basal insulinAnalog basal insulin qhsStart at 0.2U/Kg body weightTitrate until 0.5U/Kg or target FBG is achieved.UNCONTROLLEDSplit human basal insulin (NPH) qhs to bidCOST ISSUE Switch tohuman basalinsulin (NPH)bid.UNCONTROLLEDAdd analog rapid-acting insulin10% of current BASAL dose or 4 Ubefore each meal.COST ISSUE Naing/1-2022COST ISSUE Human basal insulin (NPH) qhsStart at 0.2U/Kg body weightTitrate until 0.5U/Kg or target FBG is achieved.Use 80-100% of current total BASAL dose –To split into 2/3 qam 1/3 qhs or ½ qam ½ qhsUNCONTROLLEDAdd human short-acting insulin (Regular insulin)10% of current BASAL dose or 4 Ubefore each meal.Switch to human short-acting insulin(Regular insulin)Same dose of analog rapid-acting insulinbefore each meal.
Naing/1-2022112022 Standards ofMedical Care in DiabetesPharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2022; Diabetes Care 2022;45(Suppl. 1):S125–S143; ement ic-Treatment
2022 Standards of Medical Care in DiabetesInsulin therapy12Naing/1-2022Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2022; Diabetes Care 2022;45(Suppl. rticle/45/Supplement ic-Treatment
13Diabetes Management Algorithm: American Association of Clinical Endocrinologists orithms/comprehensiveNaing/1-2022
14Diabetes Management Algorithm: American Association of Clinical Endocrinologists orithms/comprehensiveNaing/1-2022
Advanced Insulin TherapyTips for successful insulin therapy NO SLIDING SCALE INSULIN Start conservatively and adjust frequentlyMaintain “50%-50% ratio” rule for basal and prandial insulin dosesFirstly, lower the fasting BG with the basal insulin.–– Consider adding prandial insulin when basal insulin dose is 0.5U/Kg.Adjust the dose frequently until the desired FASTING BG (usually 80-130) is achieved.Secondly, lower the post-meal BG with the prandial insulin.–Try to match carbohydrate amount and prandial insulin dose – Fixed prandial insulin dose with consistent amount of carbohydrate (consider using a platemethod)Flexible prandial insulin dose based on Insulin-to-Carbohydrate Ratio (ICR) (consider using asmart phone app for carb counter)Adjust the dose frequently until the desired 1-H or 2-H post-meal BG (usually 160)or next pre-meal BG (usually 80-130) is achieved.Prandial insulin is for carbohydrate, and it should be given before a mealbased on the meal (carbohydrate) size. Do not base on pre-dose BG level.–––Naing/1-2022No meal no prandial insulinSmaller meal lower dose of prandial insulinLarger meal higher dose of prandial insulin15
16Overview of Insulin Therapy (Advanced)To use together with next page # 17Step 1Step 22 to 3 injections dailywith“Basal 1” or “Basal 2” regimen1 injection dailywith a basal insulin2 to 3 injections dailywith Pre-mixed insulinbid/ac or tid/acAddGLP-1 Receptor Agonistto basal insulin2 ways to match carbohydrate amount and prandial insulin doseStep 3Multiple injections dailywith Basal Prandial TherapySimplemethodAdvancedmethodStep 4Severe insulin resistance orhigh insulin dose ( 150 Units daily)Humulin R U-500 concentrated insulinbid/ac or tid/ac (see page 17)Fixed prandial insulin dose before each mealandconsistent amount of carbohydrate (plate method)Flexible prandial insulin dose before each mealbased onInsulin-to-Carbohydrate Ratio (ICR) (see page 17)Flexible prandial insulin dose before each mealbased onICR and Insulin Sensitivity Factor (ISF) (see page 17)INSULIN PUMPNaing/1-2022
Supplement to "Overview of Insulin Therapy (Advanced)" at page 1617Insulin-to-Carbohydrate Ratio (ICR) based on body weight in LbsPatient’s weight in LbsICR ratio100-1091:16 (1 unit insulin for 16 grams carb)110-1291:15 (1 unit insulin for 15 grams carb)130-1391:14 (1 unit insulin for 14 grams carb)140-1491:13 (1 unit insulin for 13 grams carb)150-1691:12 (1 unit insulin for 12 grams carb)170-1791:11 (1 unit insulin for 11 grams carb)180-1891:10 (1 unit insulin for 10 grams carb)190-1991:9 (1 unit insulin for 9 grams carb) 200 pounds1:8 (1 unit insulin for 8 grams carb)(carbohydrate in grams)Naing/1-2022
18Simplified for primary care providers from “The Management of Type 1 Diabetes in Adults. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes(EASD)” . Diabetes Care 2021;44:2589–2625. https://doi.org/10.2337/dci21-0043Naing/1-2022
Quick Reference Guide 1/2022 version19NoteFor an annually-updated digital copy, please visit https://www.diabetesendocrine.orgor email soenaing@gmail.com or soe.naing@ucsf.edu
15-45 mg qd, po Glipizide 2.5-20 mg bid/ac, po Glimeperide 1 -8 mg qam Glyburide 1.25-20mg qam, po Prandin 0.5-4 mg tid/ac, po Starlix 60 120 mg tid/ac, po No maximum dose Januvia 25-100 mg qam, po Onglyza 2.5-5 mg qam, po Tradjenta 5 mg qam, Nesina 6.25-25mg , po Ozempic 0.25-1.0 mg qw, SubQ Trulicity 0.75-4.5mg qw, SubQ Bydureon Bcise 2 mg qw .