Transcription
PTSD Stabilisation GroupParticipant’s WorkbookWeek 1: Understanding PTSDName:Page 0 of 13
Welcome to the GroupThis 6-week group aims to teach you some practical skills to help you cope better with the symptoms ofPost-Traumatic Stress Disorder (PTSD).These skills can help you to feel better over the next few weeks, but will also prepare you for furthertherapy, if this is appropriate.One to one therapy aimed at helping you to process and make sense of your past experiences can bedifficult and upsetting at times.The techniques covered in these group sessions should make this process a little easier for you, by givingyou some skills to manage anxiety, distress, and re-experiencing symptoms.Think about when you learnt to ride a bike- you probably had stabilisers to help you balance until youbecame confident. The coping skills covered in these sessions can act like your own personal stabilisers.Course OutlineWeek123456TopicUnderstanding PTSDCoping with HyperarousalCoping with Flashbacks and DissociationCoping with Poor Sleep and NightmaresCoping with AvoidanceCoping with our Critical VoiceEach week there will be a task for you to complete between sessions, to help you try out the copingskills and find the ones that work best for you. For the coping skills to be effective, it is critical that youuse them.At the end of the 6 weeks, you will each be offered a one to one review with the group facilitator todiscuss your experience of the group, your plan for using the skills learnt in the sessions and options forfurther therapy.Your facilitator(s) is/are:*If you have any questions or concerns, need more support, or would like to talk about personal issues orexperiences, please do speak to your group facilitators, either before or after the group session, or bytelephone our Admin Team on: 0300 790 0542Page 1 of 13
Ground Rules and Online EtiquetteOne of the most valuable things about these groups is the support that you can give to each other. Tohelp everyone feel safe and comfortable, it is helpful for the group to agree some guidelines for thesessions. We will discuss and agree these as a group, but here are some suggestions below:What you can expect: Confidentiality: Please keep everything that everybody says on the course completelyconfidential. Don’t repeat it to anyone else. Please attend the online course in a private location inwhich other people won’t be able to overhear – please do not have other people in yourhousehold in the same room as you when you are in the session, as this breachesconfidentiality. Please do not record any part of the course. Respect and Kindness: Please don’t comment on what other people share or say in the groupunless invited to do so. Please don’t get involved in other activities, such as checking yourmessages or emails, whilst attending the course. Do your best to be present for everyone.Recovery: The aim of this group is to prepare you for one to one therapy. Most people willcontinue to one-to-one therapy but some people may have recovered or may decide that it is notthe right time for therapy given other struggles in their life (e.g. a court case). We will review thenext steps with you as a 30min individual call after the group and come up with an individual planfor you then. Timekeeping: Please attend on time, and stay for the duration of each session unless you havevery good reasons why you have to leave early. No pressure to talk: There is no pressure to contribute if you don’t want to, if you are ever askedfor your feedback you are welcome to just say “Pass”. We know from past experience that peoplewho interact and contribute more generally get more from these sessions as facilitators and othergroup members can more able to provide support. If you are comfortable in actively participating,please raise your hand if you would like to speak and wait until the trainer asks you to speakbefore talking. This is to stop us talking over one another, which is easy to do when we use theonline format for the course. Nobody is required to talk, and we greatly value everyone’scontributions. No Sharing of Trauma Details: You will not be directly asked in the group to talk about yourtraumatic experience. Everyone in the group will be present because they are seeing support inovercoming the trauma of a past experience but we don’t know what those experiences are.Please do not share any details of your own past experience, no matter how well intended, as thiscan be triggering for other people and we want this to be a place of safety. Should you requirefurther support following the end of the group, you will have the opportunity to talk in detailabout what happened should you wish. Support outside of groups: If we notice that your risk scores have changed we will give you a callafter the group to see if you are okay. However, not all risk issues are recorded in thequestionnaires so if you notice your risk changing or if you would like to talk about any issues thenplease let a facilitator know and we will give you a call after the group and support you as best wecan.Page 2 of 13
What we expect: Attend every session: Can miss a max of 2 sessions. If you do not contact us with a valid reasonthis will result in an automatic discharge. If you can’t attend: If you are not going to be able to attend a session, please let us know byresponding to the reminder email you received about the course or by phoning our cancellation lineson:Bournemouth: 01202 390365 Poole and Purbeck & East Dorset: 01202 651943 Southampton:02380 272000 West Dorset: 01305 762513 Please complete the online questionnaires before each session. Camera On: Please have your webcam turned on during the session, this serves multiplepurposes. It enables us to see that you are actually present and listening to what is being said andenables us to see that you are in an appropriate environment. Most importantly, it enableseveryone in the group to know they are in a safe place as they can see for themselves that no oneis present who has previously done them harm. The Mute Button: The software we use has a “mute button” that allows you and the trainers toturn your microphone on and off. The microphones on most devices are very powerful and tendto pick up lots of background noise. We ask people to keep their microphones muted unless theyare speaking. No substance use: Please do not attend the group under the influence of drugs or alcohol. As arule of thumb please could you act as if this was a face to face group where we were all meetingtogether. Be in a confidential space: This is for your benefit so that you are not distracted, but also for thebenefit of the group so that they are comfortable to share without strangers listening in.Are there any other Ground Rules that the group has identified?:Page 3 of 13
Safety PlanIf you are feeling very low and need some support between sessions, there are a number of places thatyou can turn to: In Dorset you can call CONNECTIONS on 0300 1235440. This is a 24/7 helpline for people needingurgent mental health support In Southampton the Solent MIND “Lighthouse” service can be accessed by text 'Lighthouse' andyour postcode between 4.30pm and midnight, for example: 'LIGHTHOUSE SO14 0YG' to 074 51276010 Text SHOUT to 85258. SHOUT is a 24/7 crisis support text based service The Samaritans are available 24/7 on 116123 You can call the NHS helpline on 111 Contact your GP surgery and request an urgent appointment Call 111 for medical or mental health advice 24 hours a day Go to A&E if you are worried about yours/others safetyUseful Telephone Numbers:e.g. my GP surgery, close family or friendMy Personal Safety PlanSigns that my mood is deterioratingWhat steps can I take to manage this? Where can I get support?Page 4 of 13
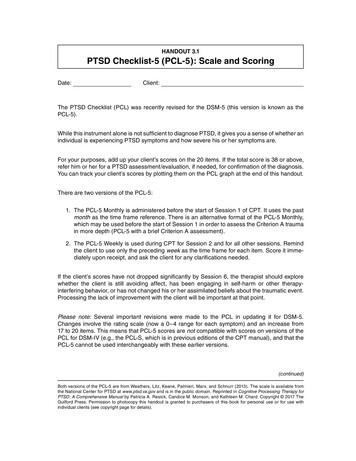
Week 1 – Introduction to PTSDStarting the group with a grounding / relaxation exerciseEach week we will start the group with a grounding or relaxation exercise. Here’s a couple that you cantry from today:Grounding videohttps://www.youtube.com/watch?v 1ao4xdDK9iEWhat is PTSD: How does it develop?"Post-traumatic stress disorder (PTSD) may develop after someone experiences a traumatic event/s. Whensomething traumatic happens in your life it rocks you to the core. The world is no longer a safe place. It becomessomewhere that bad things can and do happen.“ www.mind.org.ukOn this course and in treatment, we think it is important for you to have an understanding of what PTSDis. Knowing what PTSD is and what the symptoms means also gives us an idea of how we might work with andovercome these symptoms so doing this bit of education can be helpful in this sense.Research shows us that PTSD is very biologically based so to understand why we’re feeling the way we are; we haveto look at what’s happening in our brain. Not all of us may be very knowledgeable about the science of ourbrain so we’re going to try to explain this in laymen’s terms as much as we can.Page 5 of 13
The Caveman storyBackground: We use examples of cavemen and Lions as hopefully none of your traumas are to do with Lions andyou won’t be triggered by the stories. Please let us know now if talking about Lions will be a problem for anyone.One day a caveman was walking through the bush. As he turned a corner hestumbled across a lion fast asleep under a tree. His brain instantly recognisedthe danger and the caveman knew that he needed to get away. Luckily the liondoesn’t wake up and the caveman gets away.In the split second of seeing the lion his brain did something really clever. Itused his 5 senses to create an “early warning memory”. His brain noticed whatcolour the lion was, it noticed what type of tree the lion was sleeping under, itabsorbed the smell of the lion, it absorbed the sound that the lion made, itnoted a whole lot of information about the surrounding that the lion was in.The brain is constantly scanning our surroundings in the background andcomparing the 5 senses information coming in with our “early warningmemories” to see if it recognises anything dangerous. If it matches a 5 sensesinput to an “early warning memory” then the alarm bells go off and we enterinto fight or flight mode. This is an automatic process and we are notconsciously aware of it as it is happening in the background.Now let us imagine that a week later the caveman comes back to the same areawhere he saw the lion. The lion has now moved on but is brain recognises thesame tree as before using the “early warning memory” that it stored. His brainwill set off the alarm bells “This is where the lion was before and it could stillbe here!” The brain will also show him an image of the lion from before to tellhim why he is in danger. The alarm bells create a fear response and thecaveman will want to run away. This is good and helps to keeps the cavemansafe from danger.Let us say that the lion doesn’t come back to this place and over the next fewweeks the caveman walks passed this tree a number of times. His brain shouldregister that the danger has now gone and the “early warning memory” shouldfade in his brain and turn into a “normal memory”.But with PTSD this doesn’t happen! With PTSD the “early warning memory” getsstuck and doesn’t fade. If this caveman had PTSD he would still get the alarmbells going off years later even though the lion has never been back.Page 6 of 13
The different parts of the brain (follow on from the story above)Going back to the caveman story, the part of the brain that stores the “early warning memory” is called theAmygdala. The place where normal memories go is called the Hippocampus. Hippocampus memories are filed asstories in a filing cabinet. In order to store them away in the Hippocampus filing cabinet we need to know wherethey fit in the story of our life and how they are connected to other experiences (we call this context). Amygdalamemories are different to Hippocampus memories in a few ways: They are linked to the 5 senses – e.g. if someoneexperienced pain at the time of their trauma, theyoften get a strong memory of the pain when theAmygdala memory is triggered.Amygdala memories are fragmented (we tend to getsnippets of things that happened rather than thewhole story). This is because they are missing thecontext of how they fit into the Hippocampus.They feel like they are happening in the presentmoment. This is one of the ways that we can tell ifsomeone has PTSD.The Amygdala acts off instinct – in other words wewill do things without thinking for a few minutes andthen later when the logical brain kicks back in placeand we question our actions. Thus leading to a sense of going crazy.Videohttps://www.youtube.com/watch?v yb1yBva3XasPage 7 of 13
What are the Symptoms of PTSD?Flashbacks – Week 3Flashbacks are part of the trauma memory which have not beenprocessed yet. They are thus stored as an emotional memory inthe amygdala and have not passed through the hippocampus yetto be stored as an autobiographical memory. Thus they oftenhave a strong sensory component (images, sensations, smellsetc.) and a strong sense of ‘nowness’. They can be quitefrightening because the body reacts as if the memory ishappening in real time.Re-experiencingDissociation – Week 3Dissociation is where the brain temporarilyswitches into autopilot. There are two types ofdisassociation:1. The first type is where the brain switches intoautopilot as a way of recharging. This is commonwith all people not just people with PTSD. Someonewith PTSD is likely to have this type of dissociationmore often as hyperarousal is exhausting and thebrain is always looking for moments to recharge.2. The second type of dissociation is where thingsbecome overwhelming, for example when a verytraumatic memory is coming into yourconsciousness. Our brain has the ability todissociate and switch into autopilot as a way ofprotecting us from the memory. In some casespeople have no memory of the event due to thisdissociation.AvoidancePTSD Nightmares – Week 4Like flashbacks, nightmares emerge fromunprocessed parts of the memory. The brain triesto naturally shift the problematic memory fromthe Amygdala to the Hippocampus at night whenwe sleep. More specifically this happens duringour REM (Rapid Eye Movement) sleep, which iswhen we tend to dream. If the brain fails inshifting the memory across (which it does withPTSD) then the trauma memory bounces backand features in our dreams as a nightmare. Inweek 4 we speak about how to understand sleepbetter and we give you tips and hints on how toimprove sleep.HyperarousalAvoidance – Weeks 5 and 6Hyperarousal – Week 2Having flashbacks and PTSD symptoms is verydistressing. It is understandable that we would wantto avoid anything that would trigger this response.The problem is that the more we avoid the more ourlife shrinks down and we are able to do less and less.Week 5 talks about the practicalities of avoidanceand how we can get some of our life back again.While in week 6 we tackle our internal critical voiceor internal bully, which also holds us back.Hyperarousal is often described as being on edgeall the time. This is because the Amygdala isscanning for danger all the time with PTSD. Thissets of the ”fight-or-flight” response. We look athow to calm this symptom down in week 2.Hyperarousal can also make it difficult to sleepwhich is something we look at in week 4.Page 8 of 13
What are MY symptoms of alActivityEmotionsThoughtsPage 9 of 13
Why do some people get PTSD and others don’t?Research has shown that of all people who go through a traumatic experience, 10% are more likely to developpersistent PTSD symptoms. There are various theories explaining why this may happen:Theory 1: By avoiding looking and thinking about the trauma, the brain cannot form the necessary connectionsneeded for it process this memory in the Hippocampus.Theory 2: The Hippocampus has shrunk. This then limits the person’s ability to process the trauma memory. Brainscans of people with PTSD consistently show that they have reduced hippocampal volume. Hippocampal volumecan reduce in one of 3 ways: We are born that wayTrauma or extreme stress during childhood can inhibit the growth of the hippocampusProlonged exposure to stressful situations can reduce hippocampal volume in adults (which could explainwhy war veterans are prone to PTSD). Brain scans on military personal before and after entering a war zoneshow a shrinking of the hippocampus.Theory 3: the type of trauma: One of the things that we know is that the type of trauma plays a significant role inwhether it becomes PTSD or not. A God-made trauma such as a natural disasters e.g. an earthquake - around 2.5-3.5% for an earthquakeA non-personal Man-made e.g. a car accident, a war zone – around 4-7% for war zone]Interpersonal trauma i.e. one person attacking another person e.g. assault? [Ans 30-54% depending onthe type of assault]The good news: all the parts of the brain are able to shrink and expand depending on how we use them. The partsof the brain work like a muscle – the more we use them the stronger they get and the more we don’t use them theweaker they get (we call this ‘neuroplasticity’).How do we treat PTSD?Both EMDR and CBT have been shown to increase hippocampal volume after a course of treatment.CBT: By changing the trauma from pictures (as stored in the Amygdala) into language (spoke or written) thememory is changed into a format that the Hippocampus is able to receive. The next step is to help theHippocampus to make connections to that memory (i.e. form context around it). This is done by your therapist whowill ask questions to help the Hippocampus work out where that memory needs to go.EMDR Definition: Eye Movement Desensitization and Reprocessing is an alternate way of processing traumamemories. The brain scan of someone having a flashback shows that one side of the brain is more active than theother side. EMDR mirrors our REM sleep (where our eyes move left and right). This bi-lateral stimulation helps to“wake up” the other side of the brain which in turn helps to increase processing and helps the trauma memory toshift to the Hippocampus.Page 10 of 13
Task for the week:1. Go over the information from today to make sure you understand it. Bring back any questions that you mayhave next week2. (Optional) Try to explain PTSD to a friend or family member (If you can explain it then it shows that youunderstand it)Summary of the session: We can use our 5 senses to calm down our symptoms (we call this grounding)We’re not alone – otherpeople also have PTSD symptomsThe brain is doing a helpful thing by creating “early warning memories”. It just becomes a problem whenthe “early warning memory” gets stuck and the alarm bells go off at the wrong time.Early warning memories are triggered by the 5 senses. They are different to normal memories in that theyfeel like they are happening in the present. These memories are often senses based and fragmented, ratherthan a coherent story.The part of the brain that stores the early warning memory is called the AmygdalaThe part of the brain that stores normal memories is the Hippocampus. Memories in the Hippocampushave context which helps us know they are in the past.The Amygdala acts off instinct – in other words we will do things without thinking for a few minutes andthen later when the logical brain kicks back in place and we question our actions. Thus leading to a sense ofgoing crazy.The symptoms of PTSD are: hyperarousal (feeling on edge), flashbacks (reliving the event in the present),dissociation (going into auto-pilot), nightmares and avoidance.Each of the symptoms is addressed in a different week of the course.Having trauma doesn’t mean you will get PTSD. The size of the Hippocampus and the nature of the traumaboth impact how likely people are to develop PTSDPTSD can be treated. The two best therapies to treat PTSD are CBT therapy and EMDR therapyNotes:Page 11 of 13
APPENDIX – Further ReadingGrounding – 5 senses (what can you see/hear etc.)Use your room and your surroundings to help ground yourself. Name:5 Things you can See4 Things you can Feel3 Things you can Hear (e.g. pens and paper in front of you)2 Things you can Smell1 Thing you can Taste (e.g. tea of taste a biscuit)Further explanation on PTSD What we know is that our brain processes the things that we go through every day and there are two key areasthat are involved in that processing that we look at when understanding PTSD:The hippocampus – in charge of all our long-term memories. This means that every day, when you’re doing things,the hippocampus is filing them all way for later recall. When the hippocampus files things away, it has a system – itfiles things according to the time and context they were happening in. So for example, if you think back to therestaurant you ate at last week, it is your hippocampus which is responsible for the memory of where you went,what you ate, who you were with etc.The amygdala – in charge of our fight/flight/freeze response. This part of the brain is working everyday with ourfive senses to take in information about what is going on around us, and making an assessment on how we shouldrespond to this (fight/flight/freeze). So for example, if you were at the restaurant and a lion suddenly appeared,the amygdala would be storing via the 5 senses what that experience was like (smells, sounds, sights etc). It wouldthen use this sensory information as an early warning system for future danger. This means in the future, if we seesomething that matches the sensory experience of the lion in the restaurant, we may start to feel the same way wedid at that time (e.g. fear, urge to flee etc).So, we have these two areas of the brain working every moment of every day to keep us aware, informed andresponsive to our environment.We know that when we go through a traumatic event, our memory of it can become ‘stuck’ in the amygdalaregion. This means that long after we’ve escaped our trauma, our amygdala (which is our early warning system)may still use the 5 senses information from the traumatic event as an indication of real danger. We can see howthis might cause problems. So, in our example, witnessing a lion in a restaurant could be a traumatic experiencefor us. However, once the lion has been removed, that restaurant logically is a safe place again. However, in PTSD,the way our unprocessed trauma memories affect us is that they make us feel like there is a sense ofimmediate danger if we encounter any matching sensory triggers – so going back into that restaurant or maybe anysimilar looking restaurant might provoke fear or even flashbacks.Again, it is important to remember that this is our brain trying to help us and keep us safe by reminding us throughflashbacks, fear etc. that this is a dangerous situation.We know that if we can get our trauma memory to be better processed and put into our long-term storage (thehippocampus), we can reduce our fear and other symptoms of PTSD.The good news is that the brain is able to correct itself. Most of the time this is a natural process where the personadjusts to the sensory triggers and the trauma memory gets converted to a normal memory (i.e. searched in anormal hippocampal way) through adding time and context to the memory. However, for some of us, this doesn’thappen naturally, the memory gets stuck and this is what we know as PTSD.Thankfully, there are evidence-based strategies in talking therapies to help people do this important processing aswell as manage the symptoms of PTSD in the meantime.Page 12 of 13
Participant's Workbook Week 1: Understanding PTSD Name:_ Page 1 of 13 Welcome to the Group This 6-week group aims to teach you some practical skills to help you cope better with the symptoms of Post-Traumatic Stress Disorder (PTSD). These skills can help you to feel better over the next few weeks, but will also prepare you for further .