Transcription
75 Checklists for Skilled Nursing DocumentationBarbara Acello, MS, RNLynn Riddle Brown, RN, BSN, CRNI, COS-CInitial assessments can be tricky—without proper documentation, home health providers couldlose earned income or experience payment delays, and publicly reported quality outcomes affected by poor assessment documentation could negatively impact an agency’s reputation.All of the book’s 75-plus checklists are also available electronically with purchase, facilitatingagencywide use and letting home health clinicians and field staff easily access content no m atterwhere they are.THIS BOOK WILL HELP HOMECARE PROFESSIONALS: Easily refer to checklists, organized by condition, to properly assess a new patient Download and integrate checklists for use in any agency’s system Obtain helpful guidance on assessment documentation as it relates to regulatory compliance Appropriately collect data for coding and establish assessment skill proficiencyACELLO BROWNEnsure that no condition or symptom is overlooked and documentation is as accurate as p ossiblewith Home Health Assessment Criteria: 75 Checklists for Skilled Nursing D ocumentation.This indispensable resource provides the ultimate blueprint for accurately assessing patients’ symptoms and conditions to ensure regulatory compliance and proper payment. It will help agencies deliver more accurate assessments and thorough documentation, create better careplans and improve patient outcomes, prepare for surveys, and ensure accurate OASIS reporting.HOME HEALTH ASSESSMENT CRITERIAHOME HEALTHASSESSMENT CRITERIAHOME HEALTHASSESSMENTCRITERIA75 Checklists for SkilledNursing DocumentationHHAC7529134 Home Health Assesment Book Cover Front and Back.indd 1a divisionof BLR100 Winners Circle, Suite 300Brentwood, TN 37027www.hcmarketplace.comBarbara Acello, MS, RNLynn Riddle Brown, RN, BSN, CRNI, COS -C5/21/15 12:57 PM
Home Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation is published by HCPro, a division of BLR.Copyright 2015 HCPro, a division of BLRAll rights reserved. Printed in the United States of America. 5 4 3 2 1ISBN: 978-1-55645-717-3No part of this publication may be reproduced, in any form or by any means, without prior written consent of HCPro, or theCopyright Clearance Center (978-750-8400). Please notify us immediately if you have received an unauthorized copy.HCPro provides information resources for the healthcare industry.HCPro is not affiliated in any way with The Joint Commission, which owns the JCAHO and Joint Commission trademarks.Barbara Acello, MS, RN, AuthorLynn Riddle Brown, RN, BSN, CRNI, COS-C, AuthorTami Swartz, EditorErin Callahan, Senior Director, ProductElizabeth Petersen, Vice PresidentMatt Sharpe, Production SupervisorVincent Skyers, Design Services DirectorVicki McMahan, Sr. Graphic DesignerMichael McCalip, Layout/Graphic DesignKelly Church, Cover DesignerAdvice given is general. Readers should consult professional counsel for specific legal, ethical, or clinical questions.Arrangements can be made for quantity discounts. For more information, contact:HCPro100 Winners CircleSuite 300Brentwood, TN 37027Telephone: 800-650-6787 or 781-639-1872Fax: 800-785-9212 Email: customerservice@hcpro.comVisit HCPro online at www.hcpro.com and www.hcmarketplace.com
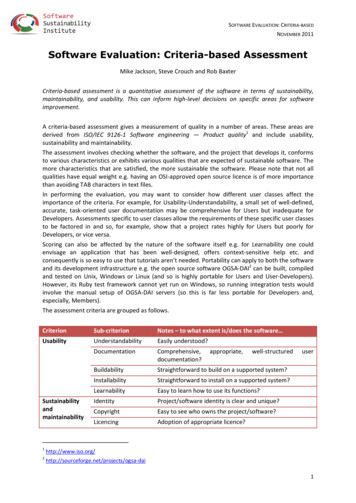
ContentsAbout the Authors. ixPurpose. xSection 1: Assessment Documentation Guidelines1.1. Medicare Conditions of Participation. 31.2. Determination of Coverage Guidelines. 81.3. Summary of Assessment Documentation Requirements. 141.4. Assessment Documentation for Admission to Agency. 201.5. Case Management and Assessment Documentation. 211.6. Assessment Documentation for Discharge Due to Safety or Noncompliance. 241.7. Start of Care Documentation Guidelines. 261.8. Routine Visit Documentation Guidelines. 311.9. Significant Change in Condition Documentation Guidelines. 351.10. Transfer Documentation Guidelines. 391.11. Resumption of Care Documentation Guidelines. 401.12. Recertification Documentation Guidelines.44Contents1.13. Discharge Documentation Guidelines. 48 2015 HCProHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentationiii
ContentsSection 2: General Assessment Documentation2.1. Vital Sign Assessment Documentation. 542.2. Pain Assessment Documentation. 572.3. Pain Etiology Assessment Documentation. 592.4. Change in Condition Assessment Documentation. 612.5. Sepsis Assessment Documentation. 652.6. Palliative Care Assessment Documentation. 672.7. Death of a Patient Assessment Documentation. 692.8. Cancer Patient Assessment Documentation. 71Section 3: Neurological Assessment Documentation3.1. Neurological Assessment Documentation. 763.2. Alzheimer’s Disease/Dementia Assessment Documentation. 793.3. Cerebrovascular Accident (CVA) Assessment Documentation. 813.4. Paralysis Assessment Documentation. 883.5. Seizure Assessment Documentation. 913.6. Transient Ischemic Attack (TIA) Assessment Documentation. 98Section 4: Respiratory Assessment Documentation4.1. Respiratory Assessment Documentation. 1014.2. Chronic Obstructive Pulmonary Disease (COPD) Assessment Documentation. 1044.3. Pneumonia/Respiratory Infection Assessment Documentation. 107ivHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation 2015 HCPro
ContentsSection 5: Cardiovascular Assessment Documentation5.1. Cardiovascular Assessment Documentation.1125.2. Angina Pectoris Assessment Documentation.1155.3. Congested Heart Failure (CHF) Assessment Documentation.1185.4. Coronary Artery Bypass Graft Surgery (CABG) Assessment Documentation. 1225.5. Coronary Artery Disease (CAD) Assessment Documentation. 1245.6. Hypertension Assessment Documentation. 1265.7. Myocardial Infarction Assessment Documentation. 1295.8. Orthostatic Hypotension Assessment Documentation. 1315.9. Pacemaker and Defibrillator Assessment Documentation. 133Section 6: Gastrointestinal Assessment Documentation6.1. Gastrointestinal Assessment Documentation. 1376.2. Cirrhosis Assessment Documentation. 1406.3. Crohn’s Disease Assessment Documentation. 1426.4. Hepatitis Assessment Documentation. 1446.5. Peritonitis, Suspected Assessment Documentation. 1486.6. Pseudomembranous Colitis Assessment Documentation. 150 2015 HCProContentsContents6.7. Ulcerative Colitis Assessment Documentation. 151Home Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentationv
ContentsSection 7: Genitourinary Assessment Documentation7.1. Genitourinary Assessment Documentation. 1557.2. Acute Renal Failure Assessment Documentation. 1567.3. Chronic Renal Failure Assessment Documentation. 1587.4. Urinary Tract Infection (UIT) Assessment Documentation. 160Section 8: Integumentary Assessment Documentation8.1. Integumentary Assessment Documentation. 1658.2. Skin Tear Assessment Documentation. 1718.3. Herpes Zoster Assessment Documentation. 1728.4. Leg Ulcer Assessment Documentation. 1738.5. Necrotizing Fasciitis (Streptococcous A) Assessment Documentation. 1778.6. Pressure Ulcer Assessment Documentation. 179Section 9: Musculoskeletal Assessment Documentation9.1. Musculoskeletal Assessment Documentation. 1869.2. Arthritis Assessment Documentation. 1889.3. Compartment Syndrome Assessment Documentation. 1929.4. Fall Assessment Documentation. 1939.5. Fracture Assessment Documentation. 198viHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation 2015 HCPro
ContentsSection 10: Endocrine Assessment Documentation10.1. Endocrine Assessment Documentation.20410.2. Diabetes Assessment Documentation. 207Section 11: Eyes, Ears, Nose, Throat Assessment Documentation11.1. Eyes, Ears, Nose, Throat Assessment Documentation. 21111.2. Dysphagia Assessment Documentation. 212Section 12: Hematologic Assessment Documentation12.1. Hematologic Assessment Documentation. 21512.2. Anticoagulant Drug Therapy Assessment Documentation. 21612.3. Deep Vein Thrombosis (DVT) Assessment Documentation. 21912.4. HIV Disease and AIDS Assessment Documentation.222Section 13: Nutritional Assessment Documentation13.1. Nutritional Assessment Documentation. 22913.2. Dehydration Assessment Documentation. 23013.3. Electrolyte Imbalances Assessment Documentation. 232 2015 HCProContentsContents13.4. Weight Loss, Cachexia, and Malnutrition Assessment Documentation. 243Home Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentationvii
ContentsSection 14: Psychosocial Assessment Documentation14.1. Psychosocial Assessment Documentation. 24814.2. Delirium Assessment Documentation. 25114.3. Psychotic Disorder Assessment Documentation.25414.4. Restraint Assessment Documentation. 257Section 15: Infusion Assessment Documentation15.1. Implanted Infusion Pump Assessment Documentation. 26115.2. Infusion Therapy Assessment Documentation.26415.3. Vascular Access Device (VAD) Assessment Documentation. 267viiiHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation 2015 HCPro
About the AuthorsBarbara Acello, MS, RN, is an independent nurse consultant and educator in Denton, Texas. She is amember of the Texas Nurses’ Association (TNA), NANDA International, and the American College ofHealthcare Administrators (ACHCA), where she was honored with the Educator of the Year Award for2007 and Journalism Award for 2009. Her employment has evolved since her graduation in 1971.She has worked as a director of nursing, administrator, long-term care facility consultant and educator,and has held numerous corporate-level positions in eight states. Presently, she is involved with freelance consulting, lecturing, and writing. She has written many textbooks, journal articles, andother materials related to acute and long-term care nursing, and nursing assistant practice andeducation. Although she has worked in acute care, emergency room, and EMS, long-term care is herpreferred practice setting. She is committed to improving working conditions, education, and professionalism for nurses and nursing assistants in long-term care facilities. She may be contacted atbacello@spamcop.net.Lynn Riddle Brown, RN, BSN, CRNI, COS-C, graduated in 1981 from The University of NorthCarolina at Chapel Hill with a B.S. in nursing. She practiced oncology nursing in Charlotte, N.C., forabout 10 years, holding positions as a floor nurse, inpatient hospice unit, and charge nurse. Duringthis time she held certification in oncology nursing through the Oncology Nursing Society.Brown first became involved with homecare in 1990, eventually moving five years later to Charleston,S.C., where she continues to work in the field. She currently holds the position of patient care coordinator and serves as the infusion nurse specialist for Roper St. Francis Home Care, a hospital-basedhome health company in Charleston. Brown holds certifications in Certified Registered NurseInfusion through the Intravenous Nursing Society and received a Certificate for OASIS Specialist-ContentsAbout the AuthorsClinical through the OASIS Certificate and Competency Board in 2010. 2015 HCProHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentationix
PurposeDocumentation has always been a large and important part of homecare. Clinicians are representingtheir profession and providing the care ordered by the physician, with little back up other than whatcan be reached by phone. Homecare works in an autonomous fashion, yet is heavily regulated by various organizations due to this very fact. It is imperative to the survival of an agency, that these regulations are followed and evidenced by documentation and outcomes of the patients.Clinicians must be proficient in their assessment skills so that the plan of care can be developed tomeet the patient’s needs and show improvement through the course of care of the patient. Not only theassessment skills must be proficient but also the skill to document patient assessments for support ofthe plan of care. Review of the documentation must provide a clear picture of the patient’s condition,needs, and interventions provided to meet established goals.Assessment of the homecare patient not only includes the physical assessment of body systems butalso the psychosocial assessment. This includes the patient’s environment, available caregivers, patient/caregiver compliance, safety needs, financial needs, spiritual and/or cultural needs or constraints toname a few. Assessment needs also can vary with the patient. There is no cookie cutter assessment thatcan be applied to all patients. It is in the assessment skills of the clinician to identify the needs of eachpatient.Know your agency’s policy and procedures for documentation requirements. Remember that documentation policy and procedures are there for a purpose and are requirements from regulatory agencies. They help protect you and the agency in a time of tough economic struggles and increasedlitigation. It is no guarantee against litigation but only with the presence of complete and accuratedocumentation can protection against litigation be found.The purpose of this book is to educate the clinician on assessment requirements of regulatory agenciesand to provide guidelines for the assessment of the homecare patient. It should be used as an aide foridentifying needs of the patient for development of the plan of care. Every patient is an individual withxHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation 2015 HCPro
unique needs and every situation to requiring assessment cannot be listed in a resource, but with the 2015 HCProPurposePurposeuse of an effective assessment tool, we can better identify these unique needs of the patient.Home Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentationxi
Section 1Assessment andDocumentation Guidelines 2015 HCProHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation1
Section 1Contents1.1. Medicare Conditions of Participation1.2. Determination of Coverage Guidelines1.3. Summary of Assessment Documentation Requirements1.4. Assessment Documentation for Admission to Agency1.5. Case Management and Assessment Documentation1.6. Assessment Documentation for Discharge Due to Safety or Noncompliance1.7.Start of Care Documentation Guidelines1.8. Routine Visit Documentation Guidelines1.9. Significant Change in Condition Documentation Guidelines1.10. Transfer Documentation Guidelines1.11. Resumption of Care Documentation Guidelines1.12. Recertification Documentation Guidelines1.13. Discharge Documentation Guidelines2Home Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation 2015 HCPro
1.1Medicare Conditions of ParticipationIntroductionMedicare Conditions of Participation govern what a homecare agency must document to qualify forMedicare reimbursement. The documentation in the patient’s record must support the need for servicesnot only for Medicare but also for Medicaid, the numerous Medicare and Medicaid HMOs, and otherinsurances. Documentation must show the need for services and that services are skilled and necessary.Documentation must reflect the patient’s needs services furnished in the home environment due tohomebound status. Some insurances may approve services for the non-homebound patient, but themajority follow Medicare’s homebound criteria. Documentation needs to reflect the nursing process,show care provided follows acceptable standards of practice, and follows the physician ordered planof care. It should be accurate and complete to support care provided and outcomes of the patient.Documentation needs to be able to stand up in a court of law. We all need to remember, “If it is notdocumented, it was not done.” Unfortunately, we now are in a healthcare society where documentationholds an equal importance to the care provided. It is important to know and understand the Conditionsof Participation. It is in understanding the why that helps us with documentation requirements.DefinitionsThe following are definitions given in the Medicare Conditions of Participation: Clinical note means a notation of contact with a patient that is written and dated by a member ofthe health team, and that describes signs and symptoms, treatment and drugs administered and thepatient’s reaction, and any changes in physical or emotional condition Progress note means a written notation, dated and signed by a member of the health team, thatsummarizes facts about care furnished and the patient’s response during a given period of time Summary report means the compilation of the pertinent factors of a patient’s clinical notes andprogress notes that is submitted to the patient’s physician Supervision means authoritative procedural guidance by a qualified person for the accomplishmentof a function or activity 2015 HCProHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation3
Conditions of ParticipationThe following are the Conditions of Participation that are related to the documentation required thatan agency must adhere to.Plan of careMust cover the following: Pertinent diagnoses Mental status Types of services Equipment required Frequency of visits Prognosis Rehabilitation potential Functional limitations Activities permitted Nutritional requirements Medications Treatments Safety measures to protect against injury Instructions for timely discharge of referral Any other appropriate itemsPeriodic review of plan of care Plan of care reviewed as often as the severity of patient’s condition requires, but at least every60 days Physician alerted promptly to any changes that suggest a need to alter plan of careConformance with physician orders Drugs/treatments administered only as ordered by the physician4Home Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation 2015 HCPro
Duties of registered nurse Makes initial evaluation visit Regularly re-evaluates Initiates the plan of care and necessary revisions Furnishes services requiring specialized nursing skill Initiates appropriate preventive and rehabilitative nursing procedures Prepares clinical and progress notes Coordinates services Informs physician and other personnel of changes in patient’s conditionClinical records Contains pertinent past and current findings Contains appropriate identifying information Name of physician Drug Dietary Treatment Activity orders Clinical and progress notes Summary reports Discharge summaryComprehensive assessment of patients Provides patient-specific, comprehensive assessment Reflects patient’s current health status Includes information that may be used to demonstrate the patient’s progress toward achievementof desired outcomes Identifies the patient’s continuing need for homecare Meets the patient’s medical, nursing, rehabilitative, social, and discharge planning needs Verifies homebound status Incorporates OASIS-C items 2015 HCProHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation5
Initial assessment visit Determines the immediate care and support needs of the patient Determines eligibility for the Medicare home health benefitDrug regimen review Comprehensive assessment includes a review of all medications to identify any potential adverseeffects and drug reactions including: Ineffective drug therapy Significant side effects Significant drug interactions Duplicate drug therapyUpdate of the comprehensive assessment Must be updated and revised as frequently as the patient’s condition warrants due to a majordecline or improvement in the patient’s condition Includes OASIS-C items Not less frequently than: Every second calendar month beginning with the start of care date Within 48 hours of the patient’s return to the home from a hospital admission At dischargeIncorporation of OASIS data items Must be incorporated into the agency’s own assessment Includes: Clinical record items Demographics and patient history Living arrangements Supportive assistance Sensory status Integumentary status6Home Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation 2015 HCPro
Respiratory status Elimination status Neuro/emotional/behavioral status Activities of daily living Medications Equipment management Emergent care Items collected at admission or discharge only 2015 HCProHome Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation7
1.2Determination of Coverage GuidelinesIntroductionMedicare has specific guidelines on determining if a patient qualifies for homecare. Determination ofcoverage is solely based on documentation, therefore accurate and complete documentation is essential.The decision of coverage is based on the patient’s plan of care, OASIS-C information, and the medicalrecord of the patient. If there is not supporting documentation in these areas to demonstrate care is reasonable and necessary, Medicare can deny coverage for the patient. The following identifies the mostimportant coverage guidelines and how documentation plays a major role. Care must be taken in interpretation of the following guidelines where coverage for the patient is questionable. Consult with supervisors or directors of your agency to determine if the patient qualifies for services under Medicare.A patient MUST meet these Conditions of Participation to qualify for home health care: Confined to home Under the care of a physician Receiving services under a plan of care established and reviewed by a physician Need of skilled nursing care on an intermittent basisPatient Confined to Residence Definition of residence: Private dwelling Apartment Relative’s home Home for the aged Vacation home Caretaker’s home The following residences as long as inpatient services are not provided: Personal care home Assisted living facility Group home8Home Health Assessment Criteria: 75 Checklists for Skilled Nursing Documentation 2015 HCPro
A patient may be transported between residence for care if Medicare requirements for homeboundstatus are met There exists a normal inability to leave the residence Leaving the residence would require a considerable and taxing effort Absences from the residence are infrequent or for periods of relatively
Clinicians must be proficient in their assessment skills so that the plan of care can be developed to meet the patient’s needs and show improvement through the course of care of the patient. Not only the assessment skills must be proficient but also the skill to document patient assessments for suppo