Transcription
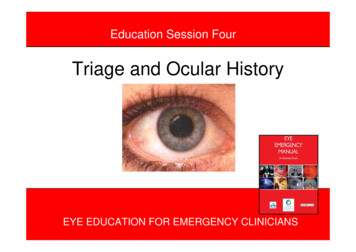
Education Session FourTriage and Ocular HistoryEYE EDUCATION FOR EMERGENCY CLINICIANSEYE EDUCATION FOR EMERGENCY CLINICIANS1
These presentations have beenprepared by: Jillian Grasso, Clinical Nurse Consultant,Ophthalmology Janet Long, Clinical Nurse ConsultantCommunity Liaison, Ophthalmology Joanna McCulloch, Transitional NursePractitioner, Ophthalmology Cheryl Moore, Nurse Educator, OphthalmologyFurther information contact us at SydneyHospital & Sydney Eye Hospital: 02 9382 7111Modules originally designed for emergency nurses as a component of the Eye Emergency Manual Project.December 2008EYE EDUCATION FOR EMERGENCY CLINICIANS2
Aim:To provide an overview of ocular triage andocular history takingObjectives:On completion of this session you will be ableto: define the appropriate triage categories forocular conditions ensure that patients are treated according totheir clinical urgency document an effective ophthalmic historyThis presentation is only focused on ocularemergency presentationsEYE EDUCATION FOR EMERGENCY CLINICIANS3
“the majority of (eye injuries) are superficial innature and transient in their effects, but placeconsiderable demands on A & E services”(MacEwan 1989)Corneal abrasionTriage 4Full thickness lid lacerationTriage 2EYE EDUCATION FOR EMERGENCY CLINICIANS4
VisionWorkingReadingTVOcular Historymyopic – retinaldetachmentMedicationhistoryOphthalmic HistoryExamples ofSpecific questionsFamily HistoryGlaucomaSquint/strabismusMedical HistoryDiabetes –VitreoushaemorrhagesSpecial questionsMechanism of injury Foreign bodyDischarge –infectionEYE EDUCATION FOR EMERGENCY CLINICIANS5
On Presentation to EmergencyThere are two important procedures for triage toperform at the same time:1.Eye Examination – refer to Education Session Two &Three for the process of Eye Examination and VisualAcuity.2.History TakingBoth of these will enable you to allocate patient’sappropriate triage category, and facilitate timelytreatmentEYE EDUCATION FOR EMERGENCY CLINICIANS6
Overview of Patient History Identify Presenting ProblemPatients Previous Ocular HistoryFamily Ocular HistoryGeneral HealthIf patient is a poor historian,culturally and linguistically diverse(CALD), or has difficultycomprehending the questions - basetriage category on eye examinationand visual acuity.EYE EDUCATION FOR EMERGENCY CLINICIANS7
Overview of Patient HistoryPlus EYE EXAMINATION: Provides more clues to fit provisionaldiagnosis Provides evidence to refute itIf the patient has one ‘good’ eye onlyand presents with symptoms in thegood eye, referral to an ophthalmologistfor review is required.EYE EDUCATION FOR EMERGENCY CLINICIANS8
Presenting Problem Record primary reason for visit – what is thepresenting problem? What prompted the visit? Has something new happened, or havesymptoms been ongoing for sometime? Why ispatient now worried?Caution: some patients may includenew symptoms to legitimise thepresentation.EYE EDUCATION FOR EMERGENCY CLINICIANS9
Presenting Problem (cont) First series of questions:– Visual acuity – was the change sudden or gradual,partial or total loss– Affecting one or both eyes– Current form of correction – is presenting problemcontact lens related?– Blurry or double vision– Red/sore/itchy eye– Flashes and floaters/ headaches– Recent eye surgery or traumaEYE EDUCATION FOR EMERGENCY CLINICIANS10
Patient’s Ocular History– Pre injury vision – has the eye always hadreduced vision? i.e. ‘lazy eye’– Ocular surgery - predispose to infection,wound dehiscence, Intraocular lens (IOL)displacement – sudden drop in visual acuity– Previous ocular trauma – Airbag related(may get flashes/floaters months later)– Use of eye drops – how often, when lastused, how long has the bottle been openEYE EDUCATION FOR EMERGENCY CLINICIANS11
Patient’s Ocular History (cont)– Conditions affecting the other eye.– Previous use of contact lenses – check foroverwear (using daily wear contact lens for 2 3 days instead of 1), using correct contactlens solution (not saliva to clean)– Ask if they have had corrective/refractiveeye surgery (when was their last follow upand when is their next follow up), be aware ofpeople having eye surgery overseas, may nothave arranged ocular follow upEYE EDUCATION FOR EMERGENCY CLINICIANS12
General Health Systemic conditions – especially vascular,inflammatory Medications - (anticoagulants), include allherbal supplements, vitamins, anti malarial Allergies – can have bearing on allergic eyeconditions i.e. lanolin can be used as a base ineye ointments Tetanus immunization status - (if eye trauma) If c/o headaches – is there a history ofmigraine, visual aura’s? Recent overseas trips – purulent discharge ? sexually transmitted infections (STIs)EYE EDUCATION FOR EMERGENCY CLINICIANS13
Thinking Points-when taking an ocular history Ask what the eye symptoms are, when first noticed, andwhat were they doing immediately beforehand(particularly if the onset was sudden) If eye scratched- what, when and force used If possible, test visual acuity at this stage– only excluded if serious life threatening condition or– chemical injury If chemical injury ask what chemical, time and previousfirst aidStart irrigation NOW! DON’T WAIT(Thinking points are adapted from Field & Tillotson 2008)EYE EDUCATION FOR EMERGENCY CLINICIANS14
Thinking Points-when taking an ocular history (cont) Record if patient has history of doing any dangerouswork. Occupation may give clue to eye problem – jackhammering, use of power tools (anything high velocity),ask about use of eye protection– Think of corneal foreign body, intraocular foreign body andcorneal abrasion. Have they been playing sport.– golf, squash & tennis balls fit perfectly in orbit – porentialruptured globe or fractured orbitEYE EDUCATION FOR EMERGENCY CLINICIANS15
Thinking Points-when taking an ocular history (cont) Document pain level and type – try to be accurate, usepain scale, ask detailed questions about exact type,locationIf analgesia has been taken, was it effective? Try todiscriminate between soreness, irritation and stinging–look out for photophobia (sensitivity to light), deep pain inand around eye, severe pain, nausea and vomiting –consider acute glaucoma Ask about family history of eye problems. Some eyeconditions can are inherited – Cataracts, Glaucoma,Retinal / Corneal Dystrophies and Retinal DetachmentEYE EDUCATION FOR EMERGENCY CLINICIANS16
Thinking Points-when taking an ocular history (cont) Ask about any previous eye problems. Especially ifhistory of poor vision in one eye since birth/childhood, orpossible reoccurrence of previous eye disease –inflammatory (uveitis), recent corrective eye laser(refractive surgery), high myopes (short sighted), retinalholes/detachment Has there been any recent illness? An upper respiratorytract infection may indicate viral eye conditionsEYE EDUCATION FOR EMERGENCY CLINICIANS17
Thinking Points-when taking an ocular history (cont) Age may be factor, some eye problems affect particularage groups:- circulatory problems may affect macularand cause degeneration; age related cataracts (gradualreduction of vision, glare); glaucoma (halos aroundlights, loss of peripheral vision) Check medications – these can further clarify presentingeye problem i.e. hypertension, diabetes and cardiacconditions may be associated with some vascular eyeconditions:- central retinal artery occlusion; diabeticretinopathyEYE EDUCATION FOR EMERGENCY CLINICIANS18
Suggested Triage CategoryBased on Australian Triage ScaleTriage 1 Immediate Life Threatening ConditionA patient should be allocated a higher triage categoryif discriminator in that category cannot be ruled out.Australian College of Emergency Medicine. (2000). The Australian Triage Scale. Carlton Vic. PublisherEYE EDUCATION FOR EMERGENCY CLINICIANS19
Triage Category 2Assessment and treatment within 10 minspotential threat to eye function or deterioratingvisual conditions. Chemical Burns (acid or alkali) needs immediateaction by nurse- Start irrigation NOW! DON’T WAIT.Penetrating eye injury (PEI) – if self evident don’ttouch except apply shield if appropriateSudden vision loss – central retinal artery occlusion,( 6/60)Severe eye pain – possible acute glaucomaEYE EDUCATION FOR EMERGENCY CLINICIANS20
Triage Category 2Acute Glaucoma – semi dilated pupilRed eye, cloudy cornea, painfulPenetrating Eye Injury –With iris prolapseEYE EDUCATION FOR EMERGENCY CLINICIANS21
Triage Category 2 Lid punctures - 3 days after being poked with fork endophthalmitisEYE EDUCATION FOR EMERGENCY CLINICIANS22
Triage Category 2 & 3Triage category 2Alkali BurnTriage category 3Hypopyon, central corneal scarEYE EDUCATION FOR EMERGENCY CLINICIANS23
Triage Category 3Assessment and treatment within 30 minutes.Potential for adverse outcome, or relief of severediscomfort/distress. Painless loss of vision – central retinal vein occlusionHistory which indicates penetrating eye injury (PEI)Hypopyon – pus in front chamber of eyeHyphaema (total) – blood in front chamber of eyeEYE EDUCATION FOR EMERGENCY CLINICIANS24
Triage Category 3 & 4Triage category 4Foreign body – metalTriage category 3HyphaemaEYE EDUCATION FOR EMERGENCY CLINICIANS25
Triage Category 4Assessment and treatment start within 60 minutesThere is a potential for an adverse outcome, orsevere discomfort and distress. Foreign body – non penetratingPainful red eyeFlash burn (welder flash) – often the pain is delayedSudden increase in numbers of floaters, especiallywith previous retinal history - Retinal detachment Flashes - Retinal detachment, especially if previousretinal history Small hyphaema - blood in front chamber of eyeEYE EDUCATION FOR EMERGENCY CLINICIANS26
Triage Category 5Assessment and treatment within 2 hoursLess urgent – condition is chronic or minor, clinicaloutcome will not be affected by delay in treatment. ConjunctivitisBlepharitisChalazionDry eyesLong term history of floaters (with no previous retinalhistory) Subtarsal foreign bodies – no eye redness.EYE EDUCATION FOR EMERGENCY CLINICIANS27
Triage Category 5Subtarsal Foreign BodyChalazionEYE EDUCATION FOR EMERGENCY CLINICIANS28
Documentation Identification– Name, Address, DOB– Date of arrival/time– Name of relatives with child Examination– Examination of both eyes Management– Investigations– Treatment– Follow-up arrangements History– When, where, and howthe injury occurred– Ocular symptomscaused by the injury– First Aid treatmentgiven– Previous oculardisorders and theireffect on vision– Whether glasses,contact lenses orprotective eye wearwas worn– Tetanus statusCheng, H. 1997, Emergency Ophthalmology, BMJ Publishing Group, London, pg 133.EYE EDUCATION FOR EMERGENCY CLINICIANS29
Summary Reiterate a summary of presenting problems tocheck for misunderstandings If possible perform and document a visual acuityand eye examination as soon as possible – thismay help in the assessment Use clinical judgement based on clinicalpresentation, the information presented is aguide onlyEYE EDUCATION FOR EMERGENCY CLINICIANS30
Differential Diagnosis of the Red Eyes – Appendix 1ConjunctivitisIritisAcute GlaucomaKeratitis(foreign bodyabrasion)MARKEDNoneNoneSlight or t to markedMARKEDMARKEDVisual AcuityNormalReducedReducedVaries with site of thelesionPupilNormalSMALLER orsameLARGE OVAL andFIXEDSame or SMALLERDischargeEYE EDUCATION FOR EMERGENCY CLINICIANS31
Conjunctivitis – Appendix 2BacterialSymptomsSignsTreatmentViral (usuallyadenoviral)AllergicRedness,FB sensation,Itching is lessIrritatingSuperficially soreItching,Burning,FB sensationCan have recent URTIStarts one eyeWithin 2days fellow eyeaffectedItchy,Watery discharge,History of allergies Purulent discharge Chemosis Caution:Gonococcal Conjunctivitis(sudden onset 12 – 24 hrs)Conjunctival folliclesPalpable preauricularlymph nodes,Watery mucus dischargeRed oedematous eyelids,Chemosis,Red oedematous eyelids Antibiotics – culturalsensitivityLid hygieneHighly contagious – stressimportance of personalhygiene – to avoid crossinfection LubricantsCold compressesAntibiotics if requiredHighly contagiousPersonal hygiene Compresses – coldLubricants withoutpreservativesRemove pathogen ifknownEYE EDUCATION FOR EMERGENCY CLINICIANS32
ReferencesAustralian College of Emergency Medicine. (2000).The Australian Triage Scale. Carlton Vic.PublisherCheng, H. 1997, Emergency Ophthalmology, BMJPublishing Group, London.Field.D,. & Tillotson.J., (2008) Eye Emergencies –The practitioner’s guide, M & KMarsden.J. (2006) Ophthalmic Care, WileyMacEwan. 1989EYE EDUCATION FOR EMERGENCY CLINICIANS33
Overview of Patient History Identify Presenting Problem Patients Previous Ocular History Family Ocular History General Health If patient is a poor historian, culturally and linguistically diverse (CALD), or has difficulty comprehending the questions - b