Transcription
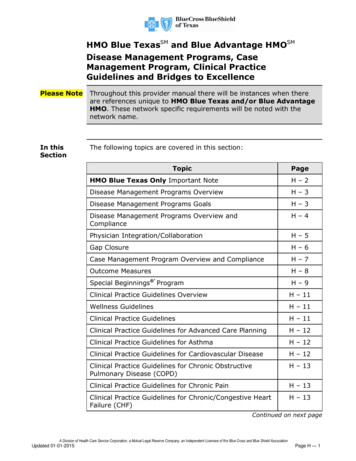
HMO Blue TexasSM and Blue Advantage HMOSMDisease Management Programs, CaseManagement Program, Clinical PracticeGuidelines and Bridges to ExcellencePlease NoteThroughout this provider manual there will be instances when thereare references unique to HMO Blue Texas and/or Blue AdvantageHMO. These network specific requirements will be noted with thenetwork name.In thisSectionThe following topics are covered in this section:TopicPageHMO Blue Texas Only Important NoteH–2Disease Management Programs OverviewH–3Disease Management Programs GoalsH–3Disease Management Programs Overview andComplianceH–4Physician Integration/CollaborationH–5Gap ClosureH–6Case Management Program Overview and ComplianceH–7Outcome MeasuresH–8Special Beginnings ’ ProgramH–9Clinical Practice Guidelines OverviewH – 11Wellness GuidelinesH – 11Clinical Practice GuidelinesH – 11Clinical Practice Guidelines for Advanced Care PlanningH – 12Clinical Practice Guidelines for AsthmaH – 12Clinical Practice Guidelines for Cardiovascular DiseaseH – 12Clinical Practice Guidelines for Chronic ObstructivePulmonary Disease (COPD)H – 13Clinical Practice Guidelines for Chronic PainH – 13Clinical Practice Guidelines for Chronic/Congestive HeartFailure (CHF)H – 13Continued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationUpdated 01-01-2015Page H — 1
HMO Blue Texas and Blue Advantage HMODisease Management Programs, CaseManagement Program, Clinical PracticeGuidelines and Bridges to Excellence, cont’dPlease NoteThroughout this provider manual there will be instances when there arereferences unique to HMO Blue Texas and/or Blue AdvantageHMO. These network specific requirements will be noted with thenetwork name.In thisSection,cont’dThe following topics are covered in this section:TopicHMO BlueTexas OnlyImportantNotePageClinical Practice Guidelines for DepressionH – 13Clinical Practice Guidelines for DiabetesH – 13Clinical Practice Guidelines for GeriatricsH – 13Clinical Practice Guidelines for HyperlipidemiaH – 13Clinical Practice Guidelines for Hypertension (HTN)H – 13Clinical Practice Guidelines for Metabolic SyndromeH – 13Clinical Practice Guidelines for Tobacco CessationH – 14Clinical Practice Guidelines for Weight ManagementH – 14Bridges to ExcellenceH – 15HMO Blue Texas physicians and professional providers who arecontracted/affiliated with a capitated IPA/Medical Group must contactthe IPA/Medical Group for instructions regarding referral andpreauthorization processes, contracting, and claims-related questions.Additionally, HMO Blue Texas physicians or professional providerswho are not part of a capitated IPA/Medical Group but who provideservices to an HMO Blue Texas member whose PCP iscontracted/affiliated with a capitated IPA/Medical Group must alsocontact the applicable IPA/Medical Group for instructions. HMO BlueTexas physicians or professional providers who are contracted/affiliated with a capitated IPA/Medical Group are subject to that entity’sprocedures and requirements for HMO Blue Texas physician orprofessional provider complaint resolution.Continued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationPage H — 2Updated 01-01-2015
HMO Blue Texas and Blue Advantage HMODisease Management ProgramsPlease NoteThroughout this provider manual there will be instances when there arereferences unique to HMO Blue Texas and/or to Blue AdvantageHMO. These network specific requirements will be noted with thenetwork name.DiseaseManagementProgramsOverviewThe HMO Blue Texas and Blue Advantage HMO DiseaseManagement Program provides chronically ill HMO Blue Texas andBlue Advantage HMO members with the resources to remain healthyand maintain their quality of life. The program is available to membersdiagnosed with asthma, chronic obstructive pulmonary disease,congestive heart failure, coronary artery disease and cardiovascularcondition clusters, diabetes, low back pain, metabolic syndrome,weight management, and/or those who need assistance with tobaccocessation. Member enrollment is voluntary; candidates are identifiedthrough continuous recruitment.HMO Blue Texas and Blue Advantage HMO takes a comprehensiveapproach to Condition Management by involving the patient, the Planand the attending physician in the education and counseling process.HMO Blue Texas and Blue Advantage HMO will notify physicians inwriting of their patients’ enrollment in the program and provideperiodic updates on patient progress as needed. When appropriate,HMO Blue Texas and Blue Advantage HMO will notify physicians ofchanges in their patients’ health status and encourage patients tomaintain open communication with their Physician.DiseaseHMO Blue Texas and Blue Advantage HMO has established theManagement following goals for the Disease Management Program:Programs Enhance member self-management skillsProgram Reduce intensity and frequency of disease-related symptomsGoals Enhance member quality of life, satisfaction, and functionalstatus Improve member adherence to the physician’s treatment plan Improve communication among member, physician, and healthplan Facilitate appropriate health care resource utilization Reduce avoidable hospitalizations, emergency room visits, andassociated costs related to the disease; and reduce workabsenteeism and medical claim costs Enhance member closure of condition specific gaps in careContinued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationUpdated 01-01-2015Page H — 3
HMO Blue Texas and Blue Advantage HMODisease Management Programs, cont’dPlease NoteThroughout this provider manual there will be instances when thereare references unique to HMO Blue Texas and/or to BlueAdvantage HMO. These network specific requirements will be notedwith the network name.DiseaseManagementProgramsOverview andCompliancePeriodic assessments are conducted to identify diseases that have asignificant impact on members. To identify members appropriate fordisease management, risk stratification is performed using pharmacy,lab and medical claims as well as the predictive modeling tool. Basedon stratification results, targeted interventions are offered to addressmembers’ levels of disease severity.Members with mild severity may receive educational materials andother self-management tools to support their physician’s treatmentplan. Each member with the condition receives a seasonal mailer andan outbound call. Members with a moderate or severe condition areeligible for extended program components.The Blue Care Connection Program staff coordinate all chroniccondition participant services and collaborates with specialty staff toensure continuity and coordination of care for those members with amoderate or severe condition. The focus of the conditionmanagement program includes the management of chronicconditions; Diabetes, Coronary Artery Disease (CAD) andCardiovascular Condition Clusters, Congestive Heart Failure (CHF),Chronic Obstructive Pulmonary Disease (COPD), Low Back Pain, andAsthma. A hierarchy is used to determine which of multiple conditionsa member is experiencing has the highest priority to include themanagement and support of comorbid conditions.In addition, the Blue Care Connection Program staff has experience inand processes in place to manage chronic conditions, such ashypertension, metabolic syndrome, cancer and oncology relateddiagnosis, migraine headaches, gastroesophageal reflux disease, andosteoarthritis.Continued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationPage H — 4Updated 01-01-2015
HMO Blue Texas and Blue Advantage HMODisease Management Programs, cont’dPlease NoteThroughout this provider manual there will be instances whenthere are references unique to HMO Blue Texas and/or to BlueAdvantage HMO. These network specific requirements will benoted with the network name.PhysicianIntegration/CollaborationThe Blue Care Connection program plan of care is designed tosupport the physician’s treatment plan. The physician may becontacted by the clinician and/or Plan medical director for clinicianto clinician consultation as follows: Clarification of the member’s treatment plan including opengaps in care; Clarification of medications; Member is non-compliant with treatment; There are concerns related to member safety and/or qualityissues; Behavior or lifestyle is detrimental to the condition beingmanaged; Clinician cannot reach the member and has information thatcould be vital to share with the provider.Blue Care Connection resources can help a member plan andmanage their health, but does not replace the care of a physician.The intent of the physician collaboration is to alert the physician togaps in health care and outreach to the physician to involve themin facilitating condition specific gap closure. The physiciancollaboration is designed to respect the physician’s knowledge andstrengthen the relationship between the physician and theirpatient.A Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationUpdated 01-01-2015Page H — 5
HMO Blue Texas and Blue Advantage HMODisease Management Programs, cont’dPlease NoteThroughout this provider manual there will be instances whenthere are references unique to HMO Blue Texas and/or to BlueAdvantage HMO. These network specific requirements will benoted with the network name.Gap ClosureGap closure focuses on showing improvement in the member’scare through engaging them and their physician in bettermanagement of health outcomes. The Blue Care Connectionclinical staff can identify opportunities from claims that a physicianmay not be able to identify during a normal office visit. To identifygap closure and health improvement opportunities, the clinicianresearches a member’s claims history through review of claimshistory available in the medical management system platform.Gap closures and health improvement opportunities may includethe following: DiabetesoooooNo physician office visit in 6 monthsNo HbA1C in the past 12 monthsNo low density lipoprotein in the past 12 monthsNo microalbuminura in the past 12 monthsNo ACE inhibitor or ARB in the past 6 months fordiabetes with hypertension Asthmao Not on controller medications Chronic Obstructive Pulmonary Disease (COPD)o Congestive Heart Failure (CHF)o No physician office visit in the past 6 monthsCoronary Artery Disease (CAD) and CardiovascularCondition Clusterso Bronchodilator adherenceNo low density lipoprotein in the past 12 monthsLow Back PainoNo evidence of medication adherence or compliancewith therapyContinued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationPage H — 6Updated 01-01-2015
HMO Blue Texas and Blue Advantage HMOCase Management ProgramPlease NoteThroughout this provider manual there will be instances whenthere are references unique to HMO Blue Texas and/or to BlueAdvantage HMO. These network specific requirements will benoted with the network plex Case Management Programs focus on the one to twopercent (1% - 2%) of the population with late stage chronic orcatastrophic conditions such as: transplants, major trauma, rarediseases, and end of life issues. The Utilization Management andBlue Care Connection staff members are trained on medicalevents that may trigger a referral to complex Case Management.Care Coordination and Early Intervention Program is atransition of care model that fosters clinical improvement. Theprogram provides pre-admission, inpatient, and post-dischargeoutreach designed to provide educational and safety support tomembers having an admission for a targeted diagnosis orprocedure code that has been identified as having a high potentialfor readmission and/or post discharge complications. The programfocus is to reduce readmissions, emergency room visits, andimprove member health outcomes.NICU. The NICU program is administered internally by specialtyR.N.s along with an assigned neonatologist. The assignedspecialist is not an employee of BCBSTX, but is a credentialed,practicing specialist. The focus of the programs is on enhancingand supporting the physician’s treatment plan and on assisting themember with navigation through the medical care system whilemaximizing their benefit dollars.Program components include the following: Weekly telephonic case review with the Plan medicaldirector, an assigned neonatologist, and the NICU R.N.Ongoing telephonic contact between the Plan medicaldirector and the attending neonatologist to discuss theappropriate level of care and treatmentCoordination of home health and DMESocial service support for assistance in addressing barriersto dischargeContinued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationUpdated 01-01-2015Page H — 7
HMO Blue Texas and Blue Advantage HMOCase Management Program, cont’dPlease NoteThroughout this provider manual there will be instances whenthere are references unique to HMO Blue Texas and/or to BlueAdvantage HMO. These network specific requirements will benoted with the network name.OutcomeMeasuresThe Case Management Program is URAC accredited and meetsstate regulatory requirements for case management. Standardreports are produced periodically and summarize: Resource utilization Goals met Overall member satisfaction Quality of life and functional statusContinued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationPage H — 8Updated 01-01-2015
HMO Blue Texas and Blue Advantage HMOCase Management Program, cont’dPlease NoteThroughout this provider manual there will be instances whenthere are references unique to HMO Blue Texas and/or toBlue Advantage HMO. These network specific requirements willbe noted with the network name.SpecialBeginnings ’ProgramChildbirth-related expenses have become one of the largestcomponents of health care costs today. To maintain costs and toassist female members in achieving healthy pregnancyoutcomes, BCBSTX offers the Special Beginnings program, ourobstetrical wellness program, to most of our HMO Blue Texasand Blue Advantage HMO members. This program monitorsHMO Blue Texas and Blue Advantage HMO members fromprogram referral through the first six weeks of the infant’s lifewith a goal of achieving healthier families through proactive preand post- natal health education. In addition, BCBSTX provideshigh-risk pregnancy case management services to all HMO BlueTexas and Blue Advantage HMO members.Program Overview — The Special Beginnings program includesa pregnancy risk assessment, educational materials, andtargeted outreach during the pregnancy and for six weeks afterdelivery. Program participants also have access to an obstetricalregistered nurse case manager throughout the program.Risk Assessment — When the plan is notified of a member’spregnancy, the member is contacted to determine her interest inparticipating in the voluntary Special Beginnings program. If shechooses to participate, an individualized risk assessment isconducted and follow-up monitoring of her pregnancy iscoordinated through a scheduled series of follow-up calls withprogram staff. The call schedule varies according to the risk levelof the pregnancy; however, women with normal pregnanciesreceive a minimum of two calls before and one call afterdelivery. During the call made within 4-6 weeks after delivery, adepression screening is completed to ensure any issues relatedto post-partum depression are addressed. If the screening ispositive, additional outreach is made until the issue is resolvedor stabilized with treatment.Educational Materials — All participants receive acomprehensive educational book covering a multitude ofpregnancy and infant care related topics. The Special Beginningswebsite accessed through Blue Access for Members also providesa wealth of pregnancy related information.Continued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationUpdated 01-01-2015Page H — 9
HMO Blue Texas and Blue Advantage HMOCase Management Program, cont’dPlease NoteThroughout this provider manual there will be instances whenthere are references unique to HMO Blue Texas and/or toBlue Advantage HMO. These network specific requirements willbe noted with the network name.SpecialBeginningsProgram,Note: To ensure HMO Blue Texas and Blue Advantage HMOmembers have the opportunity to participate in the SpecialBeginnings Program, physicians must contact the Medical CareManagement Department at 800-441-9188 or access theiExchange Web application, immediately, with notification of anypregnancy for their HMO Blue Texas and Blue AdvantageHMO members. Members may also call 888-421-7781 directlyto enroll.cont’dA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationPage H — 10Updated 01-01-2015
HMO Blue Texas and Blue Advantage HMOClinical Practice GuidelinesPlease NoteThroughout this provider manual there will be instances whenthere are references unique to HMO Blue Texas and/or toBlue Advantage HMO. These network specific requirementswill be noted with the network name.ClinicalPracticeGuidelinesOverviewClinical Practice Guidelines will be reviewed and revised, asappropriate, at least every two years. Guidelines may bereevaluated and updated more frequently, depending on theavailability of additional data and information relating to theguideline topic.Clinical Practice Guidelines are reviewed and adopted as thefoundation for its Disease Management Programs, qualityinitiative and provider tools. The guidelines are based uponnationally recognized clinical expert panels, and are availableto assist Physicians in clinical practice.WellnessGuidelinesPromotion of preventive health is a major objective of theBCBSTX Quality Improvement Program. The Adult, Infant,Child and Adolescent, and Prenatal Wellness Guidelines havebeen adopted by BCBSTX and are provided to HMO BlueTexas and Blue Advantage HMO members. The WellnessGuidelines are available on the BCBSTX Provider website atbcbstx.com/provider, under Clinical Resources.ClinicalPracticeGuidelinesClinical Practice Guidelines (CPGs) are also available foradvanced care planning, asthma, cardiovascular disease,chronic obstructive pulmonary disease, chronic pain,chronic/congestive heart failure, depression, diabetes,geriatrics, hyperlipidemia, hypertension (HTN), metabolicsyndrome, tobacco cessation and weight management.To assist in patient education, these guidelines are available toPhysicians by calling the Disease Management Department at800-462-3275, or you may access the guideline referenceson the BCBSTX Provider website at bcbstx.com/provider, underClinical Resources.Continued on next pageA Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield AssociationUpdated 01-01-2015Page H — 11
HMO Blue Texas and Blue Advantage HMOClinical Practice Guidelines, cont’dPlease NoteThroughout this provider manual there will be instances whenthere are references unique to HMO Blue Texas and/or toBlue Advantage HMO. These network specific requirementswill be noted with the network name.Clinic
Jan 01, 2015 · The Blue Care Connection Program staff coordinate all chronic condition participant services and collaborates with specialty staff to ensure continuity and coordination of care for those members with a moderate or severe condition. The focus of the condition management