Transcription
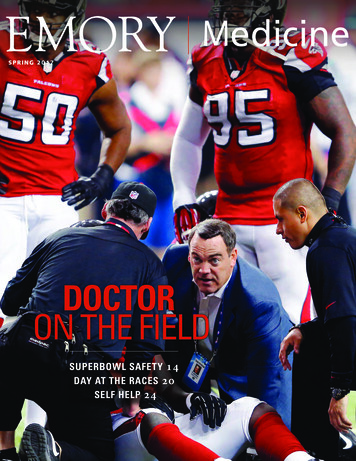
edicineSPRING 2017DOCTORON THE FIELDSUPERBOWL SAFETY 14DAY AT THE RACES 20SELF HELP 24Spring 20171
2EMORY MEDICINE
THE BIG PICTURESTREAMLINEDMadeline Locus, an Emorygraduate student in mathematics, competedin the Olympic trials in 2012 and 2016.“I love pushing myself to my limits atevery practice because I feel like I’mbecoming a better athlete and a betterperson every day,” she says. Young athleteswho specialize in highly competitive sportsneed to also schedule time for rest and restoration, say sports medicine physicians.See related article, p. 22
FROM THE DEANEndorphinsIt’s a great way to experience newplaces and to connect with the outdoors.I ran track and cross-country in highschool and was a hurdler during college,David Stephensand I’ve run in the Peachtree as well asInterim Dean, Emory Schoolof MedicineAtlanta and Chicago marathons.Studies indicate that moderateamounts of running can significantly extend your life expectancy, butthat has not been my motivation.Quite simply: Running never fails to energize me.We now know a lot more about the benefits of sports and stayingactive. At Emory, our faculty doctors care for athletes of all levels,from hobbyists like myself to the pros. Our sports medicine physicians, cardiologists, and others partner with Atlanta’s sports teamsto provide high-level care, and we recently started construction on asports medicine center and training facility with the Atlanta Hawks.“Emory is not just somewhere to go for cancer or heart disease—we also have a world-class musculoskeletal center and sports medicineprogram,” says Scott Boden, director of Emory’s Orthopaedics andSpine Center and professor of orthopaedic surgery. “Caring for themost elite and professional athletes in Georgia allows our sports medicine physicians to treat everyone with the highest level of care andexpertise, whether a professional athlete, an Olympian, a collegiate orhigh school star, or a weekend warrior.”Several of our School of Medicine researchers have also pioneeredways to keep athletes safer, from portable devices that instantly diagnose concussions to methods of reducing cardiovascular risk.We encourage wellness in our own community through events likefitness challenges in the workplace and the annual Winship 5K thatraises funds for cancer research.As I watched my grandson last week on the pitcher’s mound, I wasreminded of the benefits that sports confer on us, body and mind—but also of the need for new and better programs to keep athletes safe.Here’s to being active and healthy and getting those endorphins going.2EMORY MEDICINEDownload our iPad app (search underEmory Health magazines.) Bonus features areonline at emorymedicinemagazine.emory.edu.Emory MedicineEditor Mary LoftusArt Director Peta WestmaasDirector of Photography Jack KearseContributing Writers Carol Clark, Quinn Eastman, Marlene Goldman, MichelleHiskey, Robin Reese, Jessica Rollin, Melva Robertson, Kimber WilliamsProduction Manager Carol PintoAdvertising Manager Jarrett EppsWeb Specialist Wendy DarlingExec Dir, HS Creative Services Karon SchindlerInterim Associate VP, HS Communications Holly KorschunEmory Medicine editorialintern and Emory College juniorMelissa Mickiewicz 18C at theAtlanta Science March on April 22.Emory Medicine is published twice a year for School of Medicinealumni, faculty, and staff, as well as patients, donors, and otherfriends. Emory UniversityEmory University is an equal opportunity/equal access/affirmative actionemployer fully committed to achieving a diverse workforce and complies withall applicable federal and Georgia state laws, regulations, and executive ordersregarding nondiscrimination and affirmative action in its programs and activities.Emory University does not discriminate on the basis of race, color, religion, ethnicor national origin, gender, genetic information, age, disability, sexual orientation,gender identity, gender expression, or veteran’s status. Inquiries should bedirected to the Office of Equity and Inclusion, 201 Dowman Drive, AdministrationBldg, Atlanta, GA 30322. Telephone: 404-727-9867 (V) 404-712-2049 (TDD).Cover ShotDOCTOR ON THE FIELD: This shot, taken by AtlantaFalcons photographer Jimmy Cribb, captures Falcons headteam physician Spero Karas of Emory sports medicinetending to a Falcons’ player at the Georgia Dome.17-SOM-DEAN-0304I enjoy running, both onthe roads and trails aroundmy home and on unfamiliarpaths while traveling.
INSIDE EMORY MEDICINE“Mascot going down!Pump him full of fluidsand cool him down.”—Dr. Ric Martinez, senior medicaladviser for the Super Bowl1422FEATURESSafety at the Super Bowl 14As senior medical adviser for the Super Bowl, which Atlanta will host in 2019,emergency medicine physician Ric Martinez and his team prepare for catastrophesfrom heart attacks to earthquakes to terrorism.Too Much Too Soon? 22Helping young, athletes reduce the risk of long-term injury.Self Help 24A non-surgical treatment for osteo-arthritis relies on the power of the body to heal itself.‘Nothing Matters More’ 3032True to its mission, the Seavey Clinic trains the next generation of ace diagnosticians.THE BARE BONESLetters4Experts Weigh InBriefsAND MORE5Investing in Discovery 34434 35 Windows of OpportunityGifts of NoteLast Word:Through My Patients’ Eyes 36Pediatrics resident Christine Belltries to see things from her patients’perspectives.11Visit us online at emorymedicinemagazine.emory.edu for bonus content. Send letters tothe editor to mary.loftus@emory.edu.7
THE BARE BONESLettersRecently, my mother had surgery at Emory Midtown, and I picked up the Winter2017 issue of your magazine. It took a while for me to get around to reading it, but now thatI have, I’m amazed. The content is incredible and every article was intriguing, managingto integrate social effects as well as the medical and science side of the story. The articleabout the baby who had surgery while still attached to the mother’s umbilical cord wastruly amazing! I also loved the excerpt from Mike King’s book. As a taxpayer, I wonder ifspending the money on mental health would prevent the astounding amount we spend tohouse people in prison.Tabetha DuncanAtlanta“A Future Without Antibiotics?”(Winter 2017) was a great article.AtlantaFind the Spring 2017 issue and more onlineemorymedicinemagazine.emory.eduNice article (“A Future Without Antibiotics?” Winter 2017), but it misses thecrux of the problem. It takes hundreds of millions of dollars to bring a drug to market. If acompany develops a great new antibiotic, the first thing that will happen is for hospitals toplace the drug on the restricted list and only use it in extreme circumstances. The result isthat the company is not going to sell enough of the drug to cover the costs of development,so there aren’t a lot of new antibiotics being developed.Roger Cole, MDSt. Louis, Mo.I read with interest the article about Lt. Col. Hofstetter (You Be the Doctor,“Double Trouble,” Winter 2017). I noticed that there was no mention if he wastested for thrombophilia. There are several not-so-rare disorders that make individualswho inherit them susceptible to deep vein thrombosis and pulmonary embolism. Testingis time sensitive. In an acute event patients often test falsely negative. It is estimated thatapproximately 5% of the white population is heterozygous for Factor V Leiden. Thereare major therapeutic and prognostic issues. Women who are Factor V Leiden have veryspecific guidelines for birth control to avoid a catastrophic event. I also read the blurb aboutGrady and Emory. My “ancestor” Dr. John Guilford Earnest was one of Atlanta’s morecolorful physicians, one of the first doctors at Grady, and taught at Emory medical schoolfor decades. He also owned the first automobile in Atlanta. We always joke when someonecomplains about the traffic in Atlanta to “blame it on Cousin John.”Robert Rhea Earnest 65C 68MWaynesville, N.C.We like to hear from you. Send us your comments, questions, suggestions, and castigations. Address correspondence to Emory Medicinemagazine, 1762 Clifton Road, Suite 1000, Atlanta, GA 30322;call 404-727-0161; or email mary.loftus@emory.edu.4EMORY MEDICINE“All adults should be vaccinated against influenza annually,receive a booster of a tetanus vaccineevery 10 years, two different types ofpneumococcal vaccine when they turn65, and a vaccine to prevent shingleswhen they reach age 60.”Infectious disease physicianWalter Orenstein, associate director of the EmoryVaccine Center, calling adultvaccine rates “disappointing,” Reuters Health NewsI’m proud of the Emory initiatives. Now Ihave a suggestion: Do another article directed at us alumni on the topic of clinicaloveruse. We should be the leaders.Joe Massey 67MExperts Weigh In“Having this convesationis a wonderful opportunity forparents to remind childrenthat everyone has variouschallenges and strengths.”Psychologist Matt Segall,encouraging parents totalk with children abouttheir autism, U.S. Newsand World Report“Hypertension is a modifiable risk factor for Alzheimer’sdisease, in contrast to other knownrisk factors such as advanced age,female gender, and family history.Therefore, there is the ability to makelifestyle changes.”Felicia Goldstein,Emory professor ofneurology, ReutersHealth News
And Your Brain Says Is therapy or medication the best way to treat your depression? A brain scan might be the most efficient way todecide.Specific patterns of activity on brain scans may help cliniciansidentify whether psychotherapy or antidepressant medication is morelikely to help individual patients recover from depression, a recentstudy has found.The study, called PReDICT, randomlyassigned patients to 12 weeks of treatmentwith one of two antidepressant medicationsor with cognitive behavioral therapy. At thestart of the study, patients underwent afunctional MRI brain scan, which was thenanalyzed to see whether the outcome oftherapy or medication depended on thestate of the brain prior to treatment.The imaging study was led by HelenMayberg, professor of psychiatry, neurology,and radiology, and the Dorothy C. FuquaChair in Psychiatric Imaging and Therapeutics at Emory’s School of Medicine.“All depressions are not equal, and like different types of cancer,different types of depression will require specific treatments. Usingthese scans, we may be able to match a patient to the treatmentthat is most likely to help them, while avoiding treatments unlikely toprovide benefit,” Mayberg says.Mayberg and co-investigators Boadie Dunlop, director of theEmory Mood and Anxiety Disorders program, and W. Edward Craighead, J. Rex Fuqua Professor of Psychiatry and Behavioral Sciences,are hoping to develop methods for a more personalized approach totreating depression.Current treatment guidelines for major depression recommendthat a patient’s preference for therapy or medication be consideredin selecting the initial treatment approach.The PReDICT study, however, showed thatpatients’ preferences were only weaklyassociated with outcomes—preferencespredicted treatment dropout but notimprovement.These results are consistent with priorstudies showing that personalized treatment for depression will likely dependmore on identifying specific biologicalcharacteristics in patients than relying ontheir symptoms or treatment preferences.The results from PReDICT suggest thatbrain scans may offer the best approach forpersonalizing treatment going forward.In recruiting 344 patients for the study from across the metroAtlanta area, researchers were able to convene a more diverse groupof patients than previous studies, with roughly half of the participantsself-identified as African American or Hispanic.—Robin ReeseReady for an Outbreak?It’s only a matter of time before another epidemic like Ebola strikes,say infectious disease expertsTo advance preparedness efforts, a 12 milliongrant awarded two years ago to establish the National Ebola Training and Education Center (NETEC)has been doubled to 24 million. The federal grant wasawarded to Emory, the University of Nebraska MedicalCenter, and NYC Health Hospitals/Bellevue. “Thisadditional money will help us educate and train morehealth care workers and develop a national researchconsortium with other centers across the country,”says Bruce Ribner, principal investigator of NETEC andmedical director of the Serious Communicable Diseases Unit at Emory University Hospital.When Ebola hit West Africa in 2014 and severalpatients were flown to the U.S. to be treated, theUniversity of Nebraska, Emory, and otherinstitutions were left to independently try todetermine the best drug for treatment.“It was inefficient. We weren’t using thesame protocols, and there was no consistency to the research,” says Chris Kratochvil,co-principal investigator of NETEC forUniversity of Nebraska Medical Center.“Now we can all collaborate to developmedical countermeasures together.” nSpring 20175
THE BARE BONESDetecting Concussions“The device is incredibly novel,” Wright says, “leveragingan immersive heads-up display with noise reduction headphones and virtual reality to interrogate brain function in realconcussions are not something to just shake off, that theretime in austere environments.”are significant short- and long-term consequences, and thatThe iDETECT technology allows testing of multipleyouth athletes are at the highest risk and have the most todomains known to be impaired after a concussion, such aslose from repetitive injury,” Wrightcognition (memory and executivesaid. “It’s time to create a culture offunction), reaction time, balance, andsafety by carefully examining activoculomotor function. The test can beities that put kids at risk, acknowlcompleted in about 15 minutes andedging when an injury occurs, anddoes not require a trained examiner.improving rules and coaching tech“Mild traumatic brain injuries inniques as well as technologies thatyouth, college, and professional sportsmakes the game safer. We must alsohave the potential for life-changing,keep kids from returning to the gamelong-term consequences,” says Wright.too early after injuries.”“The iDETECT system integrates mulWright, associate professor oftiple concussion testing capabilitiesemergency medicine at Emory, and anwithin one platform and allows rapidexpert on sports concussions, trauand reliable assessment at the locationmatic brain injury, and stroke, workswhere the injury occurred.”Dr. David Wright (right) and biomedical engineerclosely with an elite team of engineersAn estimated 1.6 to 3.8 millionMichelle LaPlaca demonstrate iDETECT, a portabledevice for diagnosing concussions, on a footballthrough the Coulter Biomedical Engisports- and recreation-related concusplayer.neering Department at Georgia Techsions occur each year in the Unitedand Emory.States. Repetitive concussions, WrightHe co-developed iDETECT, a portable screening system forsays, are suspected to be linked to long-term disorders likesideline evaluation of concussion injuries, with Michelle Ladepression and early dementia (such as chronic traumaticPlaca, associate professor of biomedical engineering at Georgiaencephalopathy). In the last decade, emergency departmentTech. The technology won the GE NFL’s Head Health Challenge visits for mild traumatic brain injury among vulnerable popII for new innovations in 2014 and is now being used by theulations like children and developing youth have increased bymilitary to study concussion in combatants and paratroopers.more than 60%. nFitrah Hamid, Georgia TechAt last year’s spring Atlanta Science Festival, emergencymedicine physician David Wright was asked to speak aboutthe evolving science of sports safety. “We now know thatTurning the KeyA cancer diagnosis and accompanying explanations about tests and treatmentscan be overwhelming. Bioethicist Rebecca Pentz, professor of hematology and medicaloncology in research ethics at Emory, and colleagues have discovered that simple metaphors are helpful in explaining molecular testing to cancer patients. Pentz’s team evaluated 66 conversations between oncologists and patients at Winship Cancer Institute. In25 of the conversations, patients reported hearing a metaphor. One example:“For thiscancer, the food was estrogen and progesterone. So we’re going to focus on blocking thehormones because that way we starve the cancer of its food.” Other metaphors used bydoctors included: bus driver, battery, circuit, broken light switch, gas pedal, key openinga lock, and traffic jam. Of the patients asked about the metaphor, 85% said it was usefuland were able to demonstrate better understanding. “Metaphors provide a commonlanguage,” says Ana Pinheiro, an Emory medical student who worked on the study. “Themore grounded and straightforward the metaphor, the more likely patients are to followalong and understand.” The study was published in The Oncologist. n6EMORY MEDICINE
Left: At 20, Sol Kaslowwas the youngest ofthe 13-member crewon his PT boat duringWWII.Far left: Now 92, Kaslowis healing well after hisrecent TAVR procedure.“He came through withflying colors, and plansto be on the restoredPT-305 when it launches,” says his daughter.“Our entire family willget to experience thisspecial moment withhim.”The SurvivorIT TOOK SOL KASLOW FIVE DECADES TO TALK ABOUT BEINGPART OF THE INVASION OF NORMANDY AS A YOUNG NAVY SIGNALMAN ON A PATROL TORPEDO (PT) BOAT. “I couldn’t handlewithin three years. In the past, the only alternatives for thesepatients were hospice and palliative care.”“I’ve had a good life and wanted a few more years if possible,”talking about it,” he says. “You live like it just happened.”Kaslow says.Then, for his 80th birthday, he and his wife, Florence, returned“We all recognized that the decision for someone at my dad’swith a tour group to Normandy, where Allied Forces landed on the age to undergo such a procedure is a complex one. We had a lotnorthern coast of occupied France on Juneof questions about the risks and the bene6, 1944, in a well-planned invasion againstfits,” says his daughter, Nadine Kaslow, chiefGermany.psychologist at Grady Hospital and a professorAs the tour guide started talking about theand vice chair of psychiatry and behavioral sciassault—which remains the largest amphibiences at Emory. She knew her dad wouldn’t beous military invasion in history—Kaslow said,happy with a sedentary life. “He played tennis“Let me tell it, I was there.”until he was 90,” she says, “and exercised fiveNow 92, Kaslow, the only living membertimes a week, right up until the surgery.”of his PT crew that was in the NormandyWith TAVR, patients do not have to haveinvasion, plans to be on the world’s onlytheir chest opened, their heart stopped, orrestored PT-305 when it launches in Newgo on a cardiopulmonary bypass machine.Orleans this spring.Instead, during the procedure a team ofIt’s a chance he wouldn’t have hadcardiologists and cardiac surgeons thread awithout the TAVR heart procedure to address areplacement valve up through an artery in theSol and Florence Kaslow tour thesevere narrowing of his aortic valve.restored PT-305 boat, scheduled topatient’s groin and into place in his heart. Thelaunch this spring in New Orleans.“My cardiologist said I didn’t have long totechnique allows patients to recover morego, because there wasn’t enough blood circuquickly with less complications.lating,” says Kaslow, of Palm Beach Gardens, Florida, who had beenOriginally used to treat only those patients deemed high risk,feeling more tired than normal. “I had no pain, so I wasn’t aware of TAVR has proven to be an effective treatment for intermediate-riskhow serious it was. He said I might have a few more years, or I could patients and is in clinical trials with low-risk patients. Emory hasgo at any minute if I didn’t have it.”performed 2,000 TAVR procedures, more than anywhere else inAfter consulting with cardiologist Vasilis Babaliaros at Emory, the Southeast. Babaliaros trained in France with Alain Cribier, the
“Emory is not just somewhere to go for cancer or heart disease— . True to its mission, the Seavey Clinic trains the next generation of ace diagnosticians. . who inherit them susceptible to deep vein thrombosi