Transcription
ASSOCIATION OF COMMUNITY CANCER CENTERS/ 2017Patient&ASSISTANCEREIMBURSEMENTGUIDE VVRFLDWLRQ RI &RPPXQLW\ &DQFHU &HQWHUV7KLV SXEOLFDWLRQ LV D EHQH¿ W RI PHPEHUVKLS
ASSOCIATION OF COMMUNITY CANCER CENTERS (ACCC)Mark S. Soberman, MD, MBA, FACS2017-2018 PresidentChristian Downs, JD, MHAExecutive DirectorMonique J. MarinoSenior Manager, Publications & ContentAmanda PattonManager, ContentWill TrueWriter, EditorABOUT THE ASSOCIATION OF COMMUNITY CANCER CENTERSThe Association of Community Cancer Centers (ACCC) is the leading advocacy and education organization for the multidisciplinarycancer care team. Approximately 23,000 cancer care professionals from 2,000 hospitals and practices nationwide are affiliated withACCC. Providing a national forum for addressing issues that affect community cancer programs, ACCC is recognized as the premierprovider of resources for the entire oncology care team. Our members include medical and radiation oncologists, surgeons, cancerprogram administrators and medical directors, senior hospital executives, practice managers, pharmacists, oncology nurses, radiationtherapists, social workers, and cancer program data managers. Not a member? Join today at accc-cancer.org/membership or email:membership@accc-cancer.org. For more information, visit the ACCC website at accc-cancer.org. Follow us on Facebook, Twitter,LinkedIn, and read our blog, ACCCBuzz.
ASSOCIATION OF COMMUNITY CANCER ancial Counselors: A Must-Have in OncologyBy Gretchen Van DyckImplementing a Co-Pay Card, Foundation, andPatient Assistance Billing ProcessBy Ann KlinePAP Flow ChartPAP Quick Reference GuidePharmaceutical Company PatientAssistance & Reimbursement ProgramsAbbVieAmgen, Inc.ARIAD Pharmaceuticals, Inc.Astellas Pharma US, Inc.AstraZenecaBayer HealthCare Pharmaceuticals, Inc.Boehringer Ingelheim Pharmaceuticals, Inc.Bristol-Myers SquibbCelgene OncologyEisai Co., Ltd.EMD Serono, Inc.Genentech, Inc.Incyte Corporation26273031343739424547495154Ipsen Biopharmaceuticals, Inc.Janssen Biotech, Inc.Lilly OncologyMerckNovartis Pharmaceuticals CorporationPfizer, Inc.Pharmacyclics, LLCSandoz, Inc.Seattle GeneticsTaiho OncologyTakeda OncologyTesaro, Inc.Teva Oncology311161856586163666973747678798284Other Patient Assistance Programs & ResourcesAgingcare.com BenefitsCheckUp CancerCare CancerCare Co-Payment Assistance FoundationCancer Financial Assistance CoalitionCo-Pay ReliefGood DaysHealthWell Foundation8686868788888889The Leukemia & Lymphoma SocietyNeedyMedsPartnership for Prescription AssistancePatient Access Network FoundationPatient Advocate FoundationRxAssistRxHope Rx Outreach 9090919293949595ACCC 2017 Patient Assistance and Reimbursement Guide I accc-cancer.org / 1
Patient Assistance and Reimbursement Assistance Programsby Drug or ProductAbraxane (paclitaxel protein-bound particles) for injection41Actiq (oral transmucosal fentanyl citrate) [C-II]82Adcetris (brentuximab vedotin) for injection74Afinitor (everolimus) tablets64Alecensa (alectinib) capsules46Alimta (pemetrexed for injection)56Aloxi (palonosetron hydrochloride)44Alunbrig (brigatinib) tablets79Aranesp (darbepoetin alfa)23Aromasin (exemestane) tablets67Arzerra (ofatumumab) injection64Avastin (bevacizumab)46Bavencio (avelumab) injection49Bendeka (bendamustine hydrochloride) for injection82Blincyto (blinatumomab)23Bosulif (bosutinib) tablets67Camptosar (irinotecan hydrochloride injection)67Cotellic (cobimetinib) tablets46Cyramza (ramucirumab)56Darzalex (daratumumab)53Doxil (doxorubicin HCl liposome injection)53Ellence (epirubicin hydrochloride injection)67Emcyt (estramustine phosphate sodium capsules)67Emend (aprepitant)59Emend (fosaprepitant dimeglumine) for injection59Empliciti (elotuzumab)38Epogen (epoetin alfa)23Erbitux (cetuximab)56Erivedge (vismodegib)46Exjade (deferasirox) tablets64Farydak (panobinostat) capsules64Faslodex (fulfestrant)30Femara (letrozole) tablets64Fentora (fentanyl buccal tablet) [C-II]82Gardasil (Quadrivalent Human59Papillomavirus Recombinant Vaccine)Gardasil 9 (Human Papillomavirus 9-valent Vaccine, Recombinant) 59Gazyva (obinutuzumab)46Gilotrif (afatinib)35Gleevec (imatinib mesylate) tablets64Granix (tbo-filgrastim) for injection82Halaven (eribulin mesylate)44Herceptin (trastuzumab)46Ibrance (palbociclib)67Iclusig (ponatinib)26Idamycin (idarubicin hydrochloride) for injection67Idhifa (enasidenib)45Imbruvica (ibrutinib)71Imfinzi (durvalumab)34Imlygic (talimogene laherparepvec)23suspension for intralesional for injectionInlyta (axitinib) tablets67Intron A (interferon alfa-2b, recombinant) for injection59Iressa (gefitinib)30Istodax (romidepsin) for injection41Ixempra (ixabepilone)38Jadenu (deferasirox) tablets64Jakafi (ruxolitinib) tablets49Kadcyla (ado-trastuzumab emtansine)46Keytruda (pembrolizumab)59Kyprolis (carfilzomib) for injection23Lartruvo (olaratumab)56Lenvima (lenvatinib) capsules442/Lonsurf (trifluridine and tipiracil) tabletsLupron Depot (leuprolide acetate for deposit suspension)Lynparza (olaparib)Mekinist (trametinib) tabletsNeulasta (pegfilgrastim)Neupogen (filgrastim)Nexavar (sorafenib) tabletsNinlaro (ixazomib) capsulesNplate (romiplostim)Odomzo (sonidegib)Opdivo (nivolumab)Perjeta (pertuzumab)Pomalyst (pomalidomide)Portrazza (necitumumab)Procrit (epoetin alfa)Prolia (denosumab)Promacta (eltrombopag) tabletsRevlimid (lenalidomide)Rituxan (rituximab)Rydapt (midostaurin)Sandostatin (octreotide acetate) for injectionSandostatin LAR Depot (octreotide acetatefor injectable suspension)Sensipar (cinacalcet)Somatuline Depot (lanreotide) for injectionSprycel (dasatinib)Stivarga (regorafenib) tabletsSutent (sunitinib malate)Sylatron (peginterferon alfa-2b) for injectionSylvant (siltuximab)Synribo (omacetaxine mepesuccinate) for injectionTafinlar (dabrafenib) capsulesTagrisso (osimertinib)Tarceva (erlotinib)Tasigna (nilotinib) tabletsTecentriq (atezolizumab injection)Thalomid (thalidomide)Temodar (temozolomide)Torisel (temsirolimus) for InjectionTreanda (bendamustine HCl) for injectionTrisenox (arsenic trioxide) for injectionTykerb (lapatinib) tabletsVarubi (rolapitant)Vectibix (panitumumab)Velcade (bortezomib) for injectionVenclexta (venetoclax tablets)Vidaza (azacitidine)Votrient (pazopanib) tabletsXalkori (crizotinib) capsulesXeloda (capecitabine)Xgeva (denosumab)Xofigo (radium Ra 223 dichloride injection)Xtandi (enzalutamide) capsulesYervoy (ipilimumab)Yondelis (trabectedin)Zarxio (filgrastim-sndz)Zejula (niraparib)Zelboraf (vemurafenib)Zinecard (dexrazoxane) for injectionZolinza (vorinostat)Zykadia (ceritinib) capsulesZytiga (abiraterone acetate)ACCC 2017 Patient Assistance and Reimbursement Guide I 1466664642351383367595382643027, 67596453
TABLE OF CONTENTSFinancial Counselors:A Must Have in OncologyBy Gretc hen Va n D yc kAs an innovator in the oncology field, Green Bay Oncologyhas created a solid financial counseling program to ensurethat no patients have to carry the financial burden thatmay accompany a cancer diagnosis by themselves. Bysharing our story, the financial counseling team hopesother cancer programs can benefit from our experiencesto either develop their own financial counseling servicesor to enhance existing services.Our StoryThe financial counseling position at Green Bay Oncologybegan as a 1 person team 10 years ago when our groupconsisted of 7 physicians and 6 clinic locations. At a timewhen prior authorizations for IV chemotherapy were stillunheard of, the financial counselor’s basic responsibilities consisted of meeting with uninsured patients whoneeded to start treatment and working with the pharmaceutical companies to get free drug, if available. Over thenext few years, however, the financial counselor positioncontinued to grow along with patient demand and beganto include assistance for oral anti-cancer agents as well.Given the growing complexity of cancer care, along withthe increase in the number and cost of oral anticancertherapies, it is no surprise that the financial counselorprogram quickly became an important part of GreenBay Oncology. In 2015, Green Bay Oncology aligned withHospital Sisters Health System St. Vincent Hospital,becoming part of the regional cancer center and makingus the largest oncology group in northeast Wisconsin.Today, we have a team of 6 counselors assisting 9 medical oncologists, 3 pediatric oncologists, 3 radiationoncologists, 1 gynecology oncologist, 8 nurse practitioners, and 3 physician assistants across 6 cancer centerlocations in northeast Wisconsin and the Upper Peninsulaof Michigan.In our comprehensive cancer program, financial counselors follow patients from the start to the completionof their treatment journey and are an integral part ofthe patient’s experience. We act as a liaison between thepatient, the provider, and other clinic departments, aswell as the patient’s insurance carrier. Efficient communication between all of these individuals and departments is the core of our program’s success. We are alsofortunate to have providers who understand the keymessage concerning financial toxicity and its potential to impact patient outcomes. “Medicine in general,and oncology in particular, used to believe that moneyshouldn’t be a consideration in treatment,” said GreenBay Oncology provider Mitch Winkler, MD. “This led us toact as if ‘money was no object’ where cancer treatmentwas concerned. We feared that considering financialACCC 2017 Patient Assistance and Reimbursement Guide I accc-cancer.org / 3
TABLE OF CONTENTSfactors would harm our patients or impede their care. Butby neglecting financial factors in cancer treatment, we’veexposed our patients to terrible harm.”Our ProcessThe financial counselor’s job begins before the patient stepsfoot in our clinic. Acting as an advocate for patients, ourbenefits specialist will first verify their insurance benefits to ensure patients are in-network with our physicians.Once treatment is prescribed, whether IV, oral, or radiation therapy, the financial counselor will immediatelyverify that the treatment is indicated for the patient’sdiagnosis, checking the National ComprehensiveCancer Network (NCCN) Compendium and/or theMedicare Compendium.Next, we verify whether the patient’s insurance requiresprior authorization. If so, we initiate the authorization process immediately to ensure that treatment canstart within three to five days. Once we’ve obtained theauthorization approval, we continue to follow the patientto ensure that if treatment continues longer than anticipated, the approval does not lapse. We are able to generatea notification in our electronic health record (EHR) thatwill alert us of an expiring authorization two weeks beforethe expiration date. We can then go into the patient’s chartand determine if reauthorization is needed.For patients treated with oral therapies, our financialcounselors initiate the first prescription fill withspecialty pharmacy to verify insurance approval andmake sure the medication is affordable for the patient.The financial counselors first meet with patients whilethey are in the clinic, explain how specialty/mail-orderpharmacies operate and—depending on theirinsurance—discuss co-pay assistance.After meeting with the patient, we fax the prescriptionalong with the patient’s demographics, current medication list, and copies of insurance cards to our singlepoint of contact at the specialty pharmacy. Becausewe have a pre-existing relationship with this point ofcontact, communication is often quick and easy, helpingto ensure that the medication gets to the patient in atimely manner.Our pharmacy contact will notify us if an authorizationis required. Once we receive that notification we thensubmit to the insurance company for the approval. Whenapproval has been obtained, we notify the pharmacy andthe financial counselor is then given a date when thepatient is scheduled to receive his or her medication.We then verify that the patient has an appointmentscheduled for a toxicity evaluation within 10 daysfrom the date the medication is received.Financial Assistance for IV & OralTherapyIf the physician is ordering a treatment that is not yetFDA approved for the patient’s diagnosis, or not indicated(i.e., off-label), we will always try to get approval throughthe insurance company first. If we receive a denial fromthe insurance company, we then go straight to the pharmaceutical company and apply to the patient assistanceprogram in hopes to receive free drug assistance for ourpatients. We do not ask patients to fill out any patientassistance forms; all forms are completed and sent in bythe financial counselor. All that is needed from patientsis their signature and, if required, income documentationto ensure eligibility.When patients are first diagnosed and prescribed treatment, one of their first concerns is usually “How am Igoing to afford this?” Most will have insurance to assistcontinued on page 64/ACCC 2017 Patient Assistance and Reimbursement Guide I accc-cancer.org
TABLE OF CONTENTSCommercial policyUnderstanding Your Health Insurance BenefitsDate Prepared:Patient Name: Date of Birth:Insurance Carrier: Policy Number:In Network?YesNoPrimary Policy?YesNoHealth care expenses can vary from patient to patient. The following is prepared to assist you inunderstanding your health care terms and benefits. Co-Pay: A fixed amount you pay for a healthcare service, paid when you receivethe service, i.e. office visits. As this is a specialist office, this amount may be higher than what younormally pay for your primary care physician visits. Co-pays are due at the time of service. Annual Deductible: A specified amount of money that the insured (you) must paybefore an insurance company will pay a claim.Deductible met: Deductible remaining: % Co-Insurance: Your share of the costs of a healthcare service. This is usually figuredas a percentage of the amount your insurance carrier allows to be charged for services. You startpaying coinsurance after you’ve paid your plan’s deductible. Out-of-Pocket Maximum: The most you will have to pay for covered healthcareservices in a plan year through deductible and coinsurance before your insurance plan begins to pay100% of covered healthcare services. Co-Pays and deductibles may or may not apply to this amount,this varies by insurance plan.Out-of-Pocket Maximum met: Out-of-Pocket Maximum remaining: Do co-pays apply to my out-of-pocket maximum?YESNONotes:Financial Counselors are available to assist you with any insurance or financial related questionsduring the course of your treatment. Please feel free to stop in or call 920-884-3135 (toll free 866-8843135) to speak with a Financial Counselor.This is not a guarantee of benefits; we have made every effort to obtain correct benefit information from your insurancecarrier. Final determination of your benefits will be dictated by your insurance company at the time claims areprocessed. Therefore, your patient responsibility may be different.ACCC 2017 Patient Assistance and Reimbursement Guide I accc-cancer.org / 5
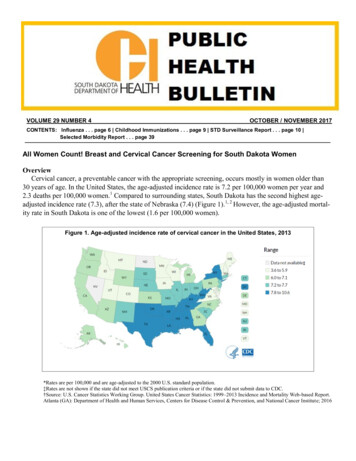
TABLE OF CONTENTScontinued from page 4them with their treatments and appointments but, aswe all know, the out-of-pocket maximums on insuranceplans just keep getting larger. It is important to meetwith patients before they start treatment and discusscost and options to help alleviate any financial burdensof cancer treatment.Depending on the type of treatment, we will go overoptions, such as foundation assistance on the nationallevel (Patient Advocate Foundation, Patient AccessNetwork Foundation, CancerCare, etc.) or on the local level.For example, in northeast Wisconsin we have some greatlocal foundations, such as Ribbon of Hope and the OvarianCancer Community Outreach (OCCO), to help reduce notonly treatment costs, but everyday living costs as well.Once approved, we will add these foundations tothe patient’s EHR and take care of all submissions forpayment. Claims are sent to the foundation beforepatients receive a bill. This process is in place to alleviateas much of the financial burden as we can from patientsin hopes of reducing any anxiety caused by additionalbills and/or collection phone calls.For commercially-insured patients who do not qualifyfor foundation assistance and/or for whom there are nofunds available for their diagnosis, we will turn to pharmaceutical company co-pay cards. These drug-specificcards can be a great option for reducing out-of-pocketcosts. There is no income limitation for these cards solong as patients give us their consent to enroll them;financial counselors can take care of everything,including submitting charges on their behalf.In 2015 alone, we saved our patients 573,328.50 on theiroral chemotherapy co-pays. This amount is only fromthree of the main specialty pharmacies we use: Accredo,Diplomat, and Community Pharmacies. Recently, in 2016,the financial counseling team worked closely with thehospital’s charity foundation and reached out to donorsto create a specific fund for our patients on oral therapythat could be used when all other foundation fundswere exhausted.6/With the constant increase of insurance plans’ yearlyout-of-pocket maximums, the amount of money ourprogram saves our patients each year continues to grow.Figure 1, page 7, illustrates exactly what was paid to ourclinic from foundations and pharmaceutical co-pay cards.This does not reflect the full grant amount that wasissued to patients. In 2015, between IV and oral chemotherapy assistance, the financial counselors at Green BayOncology saved patients more than 1 million dollars!Financial Assistance for RadiationOncologyUnfortunately the radiation oncology world is a littlebit different in terms of financial assistance. There isvery limited access to patient assistance for radiationoncology patients when it comes to treatment; for thatreason we like to meet with these patients before theystart radiation therapy.Our financial counselors provide patients with anoverview of their insurance coverage, including theirout-of-pocket responsibility, what they’ve met, andhow much they have remaining. Also, specific forms (seepage 5) are given to each patient, depending on theirtype of coverage, i.e., commercial, Medicare Advantage, orMedicare and a supplement. This information helps givepatients an idea of how much they may be responsible for.We also talk to these patients upfront regarding paymentplans, as well as Community Care/Charity Care if theyfeel this is something they would be eligible for. Patientsare also made aware that a financial counselor willbe given their treatment plan in order to verify thateverything is indicated and authorized prior to theirbeginning therapy.Due to the success of these forms in our radiationoncology department, our goal is to meet with andprovide these same benefits to all patients in themedical oncology clinic by 2017.At Green Bay Oncology, our financial counselors do notjust handle the above-mentioned duties. Financial coun-ACCC 2017 Patient Assistance and Reimbursement Guide I accc-cancer.org
TABLE OF CONTENTSAssistance for IV Therapy 450,000.00 436,483.68 400,000.00 350,000.00 340,604.81 300,000.00 281,512.31 250,000.00 200,000.00 150,000.00 167,807.35 168,863.3620112012 100,000.00 50,000.00selors are constantly involved in projects, creating newprocesses and building teams within other departmentsto continue driving our cancer program forward.Financial counselors work closely with social workersand nurse navigators to make sure patients are takencare of both inside and outside of the clinic, includingensuring patients have all the necessary appointmentsscheduled, transportati
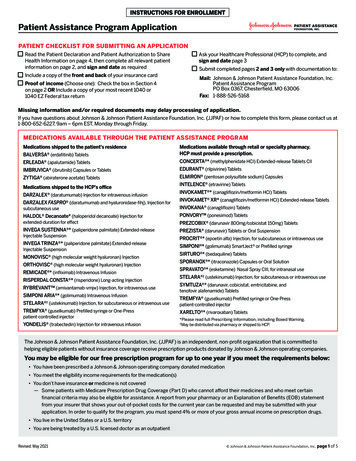
Implementing a Co-Pay Card, Foundation, and Patient Assistance Billing Process By Ann Kline 11 PAP Flow Chart 16 PAP Quick Reference Guide 18 AbbVie 26 Amgen, Inc. 27 ARIAD Pharmaceuticals, Inc. 30 Astellas Pharma US, Inc. 31 AstraZeneca 34 Bayer HealthCare Pharmaceutica