Transcription
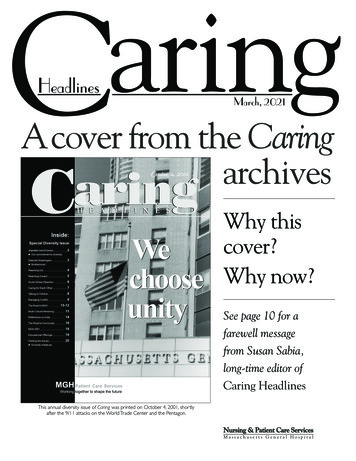
aringC HeadlinesMarch, 2021A cover from the CaringarchivesWhy thiscover?Why now?See page 10 for afarewell messagefrom Susan Sabia,long-time editor ofCaring HeadlinesThis annual diversity issue of Caring was printed on October 4, 2001, shortlyafter the 9/11 attacks on the World Trade Center and the Pentagon.Nursing & Patient Care ServicesMassachusetts General Hospital
Debbie Burke‘Rounding with purpose,’ aninvaluable opportunity to heardirectly from staff— by Debbie Burke, RN, senior vice president for Patient Care, and Peter Slavin, MD, president, MGHFrom Debbie Burke:I’ve always enjoyed rounding onunits and attending staff meetings.When I assumed this role, it wasimportant to me to incorporaterounding into my practice. It hasallowed me to learn from staff whatthey value about working at MGH,and to hear their helpful suggestionsabout how we can improve.This past year, rounding took ongreater significance during the pandemic. Dr. Slavin and I beganPeter Slavin, MDpresident, MGHDebbie Burke, RN, seniorvice president for Nursing& Patient Care Servicesrounding together, which made the experience even more meaningful.I call what we’re doing, ‘rounding with purpose.’ It gives us theopportunity to speak with individuals from all role groups andhear directly from them aboutwhat’s working, what needs tobe fixed, or what they mayneed from us. It’s also an opportunity for us to share information with staff to reinforcethe messages we want to getout — about topics like vaccinations, or visiting hours, etc.continued on next page(Photo by Kate Flock)MGH president,Peter Slavin, MD(left), and seniorvice presidentfor Patient Care,Debbie Burke,RN, rounding onthe Lunder 9Oncology Unit.Page 2 — Caring Headlines — March, 2021
Debbie Burke (continued)It has been so rewarding to be ableto thank staff in person for theamazing work they’re doing; to letthem know we understand what adifficult year it has been and howmuch we appreciate their efforts.After spending an hour or so withstaff in clinical areas, we often leavewith a lengthy ‘to-do’ list related tothe questions and concerns thatwere raised — anything from increased need for patient sitters toparking challenges with reducedcommuter rail service; vaccineavailability; growing stress in someclinical areas; and how we’re working as a system to care for COVIDpatients.in the pandemic, many of ourrounding conversations focusedon stress, anxiety, and fatigue. Aftermonths of working together in this‘new normal,’ our conversationsnow reflect much more hope andoptimism.From Peter Slavin:Rounding with Debbie has been atruly enriching experience. I thinkwe’ve both been moved by the levelof talent and dedication we see onour visits to units.Those to-do lists provide vital guidance on what issues need to be addressed, and we follow up on everyitem as quickly as we can.Every team, every unit, has a uniqueperspective, and staff seem eager toshare their thoughts with us. I lookforward to the days we round because I know I’m going to hear freshideas and impassioned suggestionsabout what we can do to make thepractice environment better.Dr. Slavin and I both appreciate thegreat strength and unity that comesfrom teamwork among staff. EarlyOver the past few weeks, we’vebegun to see spirits brighten as thenumber of COVID cases is decreas-In this IssueA Cover from the Caring Archives. 1Debbie Burke. 2-3Rounding with Dr. Slavin The Dorothy A. Terrell Endowed DiversityNursing Leadership Fellowship . 4Ash Wednesday during COVID. 52020 PCS Scholarships. 6-7Clinical Narrative. 8-9Christina Ly, RNing. Staff are feeling more comfortable with new routines, and as morepeople get vaccinated, we reallyare seeing a return to ‘normalcy.’We’ve been particularly impressedwith unit and clinic leadership —their authenticity, selflessness, andthe trusting relationships they’veforged with staff.Seeing teams working so seamlessly on behalf of patients andfamilies; feeling the spirit of teamwork and camaraderie — it’s nothing short of breathtaking to witness first-hand.Debbie and I plan to continuerounding together, meeting employees from all disciplines androle groups, hearing their thoughts,and thanking them for their service. They are an inspiration, andtruly, the everyday heroes thatmake Mass General great.Journals of Hope. 12Munn Center Research Review. 13The Effects of COVID-19-Related School Closures Practice Update. 14Circle Up HuddlesInpatient Suicide Precautions Infection Control. 15Hand Hygiene Professional Achievements. 16-17 Announcements. 18A Note from the Editor. 10-11Partner with Police & Security. 20(Debbie Burke’s head shot by Joshua Touster)March, 2021 — Caring Headlines — Page 3
Education/SupportThe Dorothy A. TerrellEndowed Diversity NursingLeadership Fellowship— by Marie Borgella, RN, nursing directorThe Dorothy A. Terrell Endowed Diversity Nursing Leadership Fellowship is an opportunity for nursesof diverse backgrounds to gain exposure to leadership experiences that can inform and shape their careers.Fellows can pursue mentorship in one of three tracks: administrative, practice, or education. Fellows will learnabout key aspects of their chosen track, such as, personnel management; operations; creating a strongprofessional practice environment, and much more.After holding several positions in other organizations,Tashika ‘Tash’ Evans, RN, began her career at MassGeneral in the EmergencyDepart ment, where shequickly demonstrated hercommitment to family-centered care, collaboration, andleadership. Always lookingfor opportunities to contribTashika ‘Tash’ Evans, RNute, Evans served as an eCarechampion in the lead-up toeCare implementation in 2015. She is a frequent preceptor to new staff and served as ‘T-nurse’ (throughputnurse, managing defined areas in the ED). When EDNursing and Hematology launched an initiative to identify and provide best practices to patients with sickle celldisease, Evans volunteered to represent ED Nursing inthe effort. Frequently consulted by medical staff and clinicians from other disciplines, Evans has come to be regarded as a go-to nurse in managing difficult patient situations and capacity overload. She is quick to supportnew nurses of diverse backgrounds, and is a member ofthe ED Nursing Diversity, Inclu sion & Equity Committee.This past summer, Evans shared her experiences as ablack nurse in the ED in hopes of making the work environment a safer and more welcoming place for diversestaff and patients.Stacy TurnbullHazeth, RN, beganher career at MassGeneral as a patientcare associate beforeearning an associate’sdegree then her BSin Nursing and becoming a nurse onthe Phillips 21 Gyn ecol ogy Oncol ogy/Stacy Turnbull Hazeth, RNGeneral SurgeryUnit. TurnbullHazeth is described as a motivating presence onthe unit, encouraging colleagues to perform attheir highest level. She often serves as preceptorto new staff and is highly regarded in her role asadjunct clinical faculty at the MGH Institute ofHealth Professions. Turnbull Hazeth is a CPR instructor and co-founder of a non-profit organization geared at keeping families together and celebrating their cultures of origin. She is an advocatefor culturally competent care and an avid educator around complex issues like, implicit bias,micro-aggression, and racism. Turnbull Hazethbecame a member of the PCS Equity & InclusionCommittee to help bring understanding to theissues of race and ethnicity among patients, providers, staff, and community.For more information about The Dorothy A.Terrell Endowed Diversity Nursing LeadershipFellowship, contact nursing director, Marie Borgella, RN, at 3-6398.Page 4 — Caring Headlines — March, 2021
Spiritual CareAshes to ashes, dust to dustObserving Ash Wednesday during COVIDF— by Alice Cabotaje, director, Spiritual Care and EducationTo many, Ash Wednesday marks acleansing and preparation for thewilderness journey of Lent, a timeof prayer, sacrifice, and good worksas they move toward reconciliation,service, and Easter.Adhering to this tradition during apandemic required some quick andinnovative thinking. Said spiritualcare provider, Julie Supple, “Giventhe need for physical distancing, Iwondered how we could offer thisritual safely. Ultimately, it challenged me to experience Lent in anew way and think creatively abouthow we could safely provide ashesto staff and patients.”Supple came up with the idea ofoffering beautiful, lavender-coloredcards affixed to envelopes containing ashes that had been blessed.Each card contained the traditionalprayers along with instructions onhow to self-administer the ashes.One staff member was moved totears as she traced the sign of thecross on her forehead. Given herrecent encounters with grief andloss, the ashes reminded her that,“Just as new growth emerges fromthe destruction of a forest fire, sotoo, new growth is promised to us.”Said Supple, “Ashes are an outwardsign of God’s love and of our lovefor one another.”For more information about the services offered by the department ofSpiritual Care, contact director,Alice Cabotaje, at 617-724-3227.(At left): RoseVisco, physicaltherapy practiceaccess coordinator,administers ashesto herself.(Below): spiritualcare provider, JulieSupple, staffs thetable she set upto distributeashes on AshWednesday.(Photos by Michelle Rose)February 17, 2021, was Ash Wednes day, a reminder to Roman Catholicsand Christians that, “for dust thouart, and unto dust shalt thou return.”To honor the occasion, the MGHSpiritual Care team distributedashes to more than a thousand patients and employees, many of whowaited in line outside the Chapeland many others who receivedashes in their rooms.March, 2021 — Caring Headlines — Page 5
Education/Support2020 PCS Scholarshiprecipients— submitted by Julie Goldman, RN, professional development program managerThrough the generosity and support of our donors, Patient Care Services was able to provide66 scholarships in 2020, the most ever presented by Patient Care Services in a single year.The Charlotte and Gil MinorNursing and Health Profess ions Scholarship to AdvanceWorkforce Diversity in PatientCare: Daniel Carvalho, CCT, pursuinga BSN at Massachusetts Collegeof Pharmacy and Health Sciences Sarbesh Chalise, RN, pursuing anMSN at Simmons University Kerry Chen, RN, pursuing anMSN at Simmons University Angela Chyn, RN, pursuing aDNP at MGH IHP Ashley Cruz, PCA, pursuing anADN at Laboure College Merisier Dianhie, PCA, pursuingan ADN at Laboure College Mirphael Guerrier, RN, pursuinga BSN at Laboure College Madelin Lizama, pursuing anADN at Bunker Hill CommunityCollege Gina Mahoney, pursuing anADN at Lawrence Memorial/Regis College Nursing Program Maybelle Mbiatem, RN, pursuingan MSN at Walden University Stephanie Medor, PCA, pursuinga BSN at MGH IHP Yvonne Muturi, RN, pursuing anMSN at UMass, Boston Thanh Nguyen, RN, pursuing anMSN at Simmons University Xandra Orogo, RN, pursuing anMSN at Walden University Rakhi Pun, PCA, pursuing anADN at Laboure College Elda Salazar, pursuing a BSN atLawrence Memorial/RegisCollege Nursing Program Melissa Sanchez, pursuing anADN at Lawrence Memorial/Regis College Nursing Program Ashley Serpas-Granados, PCA,pursuing a BSN at UMass, Boston Kaina Siffra, UC, pursuing a BSNat Curry CollegeThe Cathy GouzouleOncology Scholarship: Jennifer Duran, RN, pursuing anMS in Education at MGH IHP Molly Geary, RN, pursuing anMSN at UMass, Boston Brenda Morano, RN, pursuing anMSN at Curry College Leanne Santos, RN, pursuing anMS in Informatics at VanderbiltUniversityThe Pat Olson, RN, NursingScholarship: Halle Cabral, PCA, pursuing aBSN at Curry CollegeThe Norman Knight DoctoralNurse Scholarship: Rachel Carey, RN, pursuing aDNP at UMass, Boston Tricia Crispi, RN, pursuing a PhDat Endicott CollegePage 6 — Caring Headlines — March, 2021 Paula Knots, RN, pursuing aDNP at MGH IHP Allison Weafer, RN, pursuing aDNP at UMass, BostonThe Luella Hamilton PeaseScholarship: Tatiana Angrisano, pursuing aBSN at UMass, Boston Elvida Arias, pursuing a BSN atLaboure College Kellie Gay, pursuing a BSN atMassachusetts College ofPharmacy and Health Sciences Brooke Matacunas, CST,pursuing an ADN at LawrenceMemorial/Regis College NursingProgram Diana Mendez, PCA, pursuing anADN at Bunker Hill CommunityCollege Victoria Skarbinski, pursuing aBSN at Simmons UniversityThe Norman Knight NursingScholarship: Alyssa Abbott, RN, pursuing anMSN at Salem State University Caitlin Coveney, RN, pursuingan MSN at Framingham StateUniversity Dawn Crescitelli, RN, pursuinga BSN at Southern New Hamp shire University Alexa Daniels, RN, pursuing anMSN at Northeastern Universitycontinued on page 15
The future of health careRecipients of the 2020 PCS scholarshipsMarch, 2021 — Caring Headlines — Page 7
Clinical NarrativeCaring for COVID patient iscause for hope and reflectionM— by Christina Ly, RNMy name is Christina Ly, and I havebeen a nurse since 2015, specializing in the care of gynecology, oncology, and surgical patients. InApril, 2020, my unit began accepting medically sick COVID patientsso the focus of my care shifted.After much preparation, training,and education, I was assigned tocare for the first confirmed COVIDpositive patient admitted to ourunit. In report I learned that ‘Sarah’was already on 5L of oxygen via nasalcannula to maintain oxygen saturation. At 34 years old, she had presented 34 weeks pregnant with mildhypertension, fevers, chest pain,and shortness of breath, which hadnecessitated the Cesarean deliveryof her baby girl, who was now beingcared for in the NICU.Sarah had no other significant medical history, but I couldn’t imaginethe toll this illness would have onher and her family. She had beentransferred to our unit due to persistent fevers and an increasingneed for oxygen.At 7:30pm, I walked into Sarah’sroom. She appeared stable. Shecould converse in full sentences. Icongratulated her on the birth ofher baby and asked how she was doing. She told me she hadn’t actuallyseen her baby yet but had been ableto watch her on her phone. She re-Page 8 — Caring Headlines — March, 2021ported that her husband and uncle,whom she lived with, were alsosick. I asked if she’d be pumpingmilk for the baby, but she declined.I offered her ice packs or a tight,surgical bra if she felt any discomfort, but she said she was fine. Iasked if she had named her babyyet. She smiled and said, “Valerie.”I arranged for Sarah to have one ofthe new iPads that had been provided for COVID patients. The responding clinician and medical senior video-called while I was in theroom with Sarah. They said theywere okay with the level of oxygenSarah was receiving via nasal cannula (they’d be okay with up to 6L,the maximum amount allowed bynasal cannula before going to higherlevels of oxygen) as long as it wasn’tsustained and could be weaned backto 5L. This surprised me because Iknew patients in the ICU were being intubated when they requiredmore than 4L. They told me to letthem know if anything changedand that they’d stay close.I stayed with Sarah and continuedto assess her. After a while, sheasked if she could get up to use thebathroom. As I escorted her, I repeatedly checked with her to see ifshe was dizzy or short of breath. Ileft the oxygen in place. She wassteady on the way into the bathroom but her breathing became labored on exertion, and it took awhile for her to catch her breathChristina Ly, RNstaff nurse, Phillips 22Gynecology/Oncology/Surgical Unitwhen she returned to bed. But heroxygen requirement stayed at 5L.I left the room to get a bedside commode for next time, and when I returned, Sarah was having a fit ofcoughing; she was having troublecatching her breath. But her oxygenation was still stable. I felt bad. Itold her the good news was that shehad successfully used the bathroomand her bladder was working perfectly. I told her I’d get her somecough medication. She reassuredme that she felt okay and thankedme for, ‘being so nice.’Sarah was enrolled in a researchstudy that had very specific requirements, one of which was getting anoropharyngeal swab. According toour unit guidelines, though, wedidn’t perform oropharyngeal swabs.Ulti mately, the research nurses, ourpractice nurse specialist, and resource nurse said it was up to me if Icontinued on next page
Clinical Narrative (continued)felt comfortable swabbing her. I did,so I donned my N-95 mask. Even as Iswabbed her throat, triggering hergag reflex and causing her to tear up,she called me an angel for takingsuch good care of her.Sarah spiked a fever of 101o andwas tachycardic (had a racing heartbeat). But due to the research-studyguidelines, she couldn’t have anyTylenol. And because of COVIDprotocols, she wasn’t allowed to takeIbuprofen. I felt helpless to ease hersymptoms. All I could do was offerher ice packs and cool compresses.And still, she thanked me for everything I did.Because Sarah was part of the research study, I was scheduled togive her what could either be thetrial drug or a placebo. I couldn’thelp wondering, ‘Will this evenhelp? How will they know whichmedication or combination ofmedications is helping?’I thought we were going to make itthrough the night without anyacute changes, but at 4:30am, Sarahasked to use the bedside commode.I helped her out of bed. I had learnedthat she needed 6L of oxygen forany out-of-bed activity, which theteam was okay with. This time,though, Sarah was not able to settleback to 5L afterward, so she was puton a face mask with 10L of oxygen.When she required increasinglymore oxygen, the team decid ed totransfer her to the ICU to be intubated.I was the only person in the roomwith Sarah at the time, so I told herthe plan. I could see the worry onher face. The responding cliniciancame in to talk to Sarah about con-tacting her family and ensuringthere was a health care proxy inplace.Sarah was originally going to go tothe Surgical ICU but due to someadministrative issues, she ended upgoing to the Neuro ICU. As I saidgood-bye to Sarah, she spoke aboutwho she wanted her children’sguardian to be if she and her husband both became too sick to carefor them.The transfer was quick and smooth.Both teams were responsive. One ofmy co-workers, a new nurse, commented on how calm I seemed. Itold her it was because we were allon the same page and we all knewthe plan. But though I was calm onthe outside, inside, my heart achedfor Sarah.We hadn’t even been an officialCOVID unit for 24 hours yet. Myshift wasn’t even over, and I’d already sent a patient to be intubatedand placed on a ventilator. I couldn’thelp thinking how scared Sarahmust be, how she’d put on a braveface and was so grateful for everything I’d done.It seemed as though everything hadchanged. Caregivers talking to patients via electronic devices. Distanc ing ourselves from patients whenwe’ve been trained to stay withthem in critical situations. I questioned the effectiveness of my thinsurgical mask. Policies and procedures for COVID patients wereevolving moment by moment as welearned more about the disease. Iwondered if we’d run out of ventilators like they had in Italy.At 6:00am, before the end of myshift, the NICU nurse called to tellme she’d taken some pictures ofSarah’s baby. She wanted to comeshow them to t
DNP at UMass, Boston Tricia Crispi, RN, pursuing a PhD at Endicott College Paula Knots, RN, pursuing a DNP at MGH IHP Allison Weafer, RN, pursuing a DNP at UMass, Boston The Luella Ha


![[Page 1 – front cover] [Show cover CLEAN GET- AWAY 978-1 .](/img/13/9781984892973-6648.jpg)