Transcription
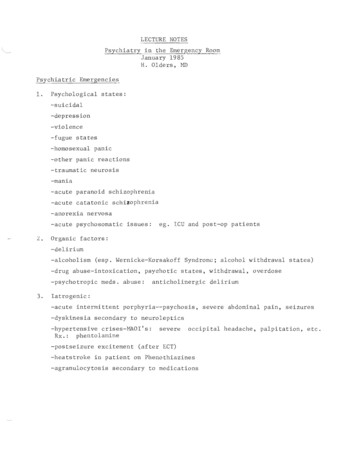
LECTURE NOTESPsychiatry in the Emergency RoomJanuary 1985H. alders, MDPsychiatric Emergencies1.Psychological states:-suicidal-depression-violence-fugue states-homosexual panic-other panic reactions-traumatic neurosis-mania-acute paranoid schizophrenia-acute catatonicschi ophrenia-anorexia nervosa-acute psychosomatic issues:L.ego ICU and post-op patientsOrganic factors:-delirium-alcoholism (esp. Wernicke-Korsakoff Syndrome; alcohol withdrawal states)-drug abuse-intoxication, psychotic states, withdrawal, overdose-psychotropic meds. abuse:3.anticholinergic deliriumIatrogenic:-acute intermittent porphyria--psychosis, severe abdominal pain, seizures-dyskinesia secondary to neuroleptics-hypertensive crises-MAOI's:Rx.:phentolaminesevereoccipital headache, palpitation, etc.-postseizure excitement (after ECT)-heatstroke in patient on Phenothiazines-agranulocytosis secondary to medications
-2 Child Psychiatry Emergencies-accidental poisoning (many are repeaters)-hyperkinesis-school phobia-adoption:adolescence crises of running away, psychosis, sexualacting out-child battering-anorexia nervosa-fire setting-sexual assault-bereavement-fatal illnessPsychiatric Problems you can handle yourself-transient/situational anxiety, ego work problems-patients with chronic problems who run out of meds (often missedan appointment)-people wi th longs tanding problems \.;rhich can be deal t \oJi th via theOPDSectorization-hospitals responsible for geographic area for psychiatric treatment-for JGH:Cote St. Luc, Hampstead, some of Snowdon, English-speakingpopulation of St. Laurent, Laval-patients belong to hospital where they have had psychiatric treatment(exc. ER) within past 6 months-if no psychiatric treatment in 6 months, then sector based on patient'saddressIntern's role in the ER-chief complaint-HPI-brief function a lenquiry-mental status-physical exam-determine need for psychiatric consult-fill out c onsult form-speak to the consultant personally-use the consultant as a learning resource
-3 Examrmed before-must befor a psychiatric consult, except:ical in past 6 weeks, results are in chartin's medical condiego an ODand there is no-patient transferred from anotherital, if the accompanyingdocuments include record oflealtoo violent ortated, exam may be deferred only until patientis sedated o transfers to otheror FHA withoutieal ote:in the Consult Form-dateccurrent and pasttreatment,-patient'sand/or your majorion-yourconsult, ie the question you would like the-rationale forconsultant to answerlike to end it all" or-no evidence that this-instead, patientself-destructive1asked "do you feel so bad that you would" or other wordstherelieved by invitation to talk re-if answer is yes, go on to ask morenature,availabilor atts-must----- tleave are asuicidal, itsrisk patient aloneRisk factors for Suicide-more than 45 years-male-divorced, widowed, or-1alone-choice of highly lethal method, firearms, jor retiredbe asked to stay until patient has been calmed orrestrained
-4 -the police, not psychiatry or the orderlies or the security guards,should deal with: -patients who claim to h ve weapons-patients who claim to be Karate experts-violent criminals-if more than one violent patient arrives at thesame time-if police not there already, they should be called for such situationsEvaluating the Risk of Violence-pay particular attention to:-threats of violence-a history of violence-paranoia and fear-cultural background where violence is frequent-your own reaction:if patient induces fear inyou, don't ignore it, deny it, misinterpret it,or try to overcome it--consider it a veryimportant warning signalCode V-Roman numeral V stands for "Violence"-when a Code V is called (paf,ed throughout hospital) a team oforderlies, specially trained as a team in safely restraining violentpatients, corne running-the psychiatrist on call is the captain of the team--doesn'tphysically participate but directs the proceedings-a code V can be called by you if necessary"Discretion is the Better Part of Valour"-potentially violent patients are often also themselves frightened- if they feel cornered or trapped, this may trigger violence-therefore always make sure you leave an escape route--don't getbet\veen the patient and the way out-if there is a risk of violence, let the patient run away if he bolts- don't try to stop him--call the policePatients who have left the building-our responsibility as doctors is limited to the building-whether on the hospital grounds or on the street, our relationship toviolent patients or patients creating a disturbance is that of an ordinarycitizen, therefore we can call the security guards or the police-remember that the patients' family or friends can request a court orderto have the patient brought to hospital by police--Crgences Sante isbest way
Cure FermE'e-any patient who is or may be dangerous to the health or safetyof himself or others, may be "committed", ie put under closetreatment or "cure fermee"-normally done by a psychiatrist, but any physician can do itif no psychiatrist available-the PSY-l04 form is good for 96 hours-examination by a second psychiatrist extends it for 21 days-"cure fermee" does not authorize treatment, only containment-the police need to see the signed form in order to bring apatient back to the hospital-if you have any doubts about a patient who demands to leave, youhave the legal responsibility and authority to keep the patientuntil assessed by psychiatryCourt Order-the most frequent court orders are those for a psychiatricexamination--read the document carefully to make sure theJGH is specifically mentionned.If not, attempt to have thepolice bring the patient to his sector hospital-occasonally, y ou may get a municipal court order to hold apatient for 30 days (usually a\.,aiti g trial).These patients,if the JGH is the designated hospital, need to be admittedReferrals to Psychiatry OPD-for patients vhose problem can stand a wait of 3 to 4 weeks,you yourself can refer the patient to the OPD--ask them tocall the Institute of Community and Family Psychiatry, tel.340-8210 and ask for the "Screening Clinic"--they will begiven an appointment-remember to let them know that they can return to the ER ifthings get worseCrisis Service-the OPD includes a crisis service which can see patientsusually within 2-3 days, but always within a week-if the patient's problem is of crisis proportion, where thecrisis service is necessary, it would usually be the psychiatristwho makes the referralprug Abuse-JGH psychiatry department does not have a detoxification program;we do have a list of resources which we can pass on to you, tosuggest to the patient who requests detoxification-acute intoxication:treated by medicine; normally, psychiatrywill only assess the patient when no longer intoxicated, egofree of ataxia or slurred speechRape Cases-refer directly to MCH or MGH, depending on age
-6 -rapphysical and medical statusassess age and-tentative differentialqiismeds (incl.hour and prior to)isof choice:and in parenteral formsavailable in PO and in PO 15-10 mgs. qus, ego EPSb-most side effects are1 hr- q 1 hr., max. 80 mgs.-lower dose for delirium or aBS-control means nobell-sedation (ie.) is not theAlcohol:BDZ aresof choice for withdrawal; thiamine IVfor Wernicke's.safer.AvoidECT may be treatment of choice.Serious(severe EPS,themia.functions)--up to 20% mortalityaltered consciousness,(increased HR,tic-induced catatonia withmay lead to death fromtics;males.Treatmentacute dystonic RXNs:-cogentin 1 or 2 mgs. 1M or IV) 50 mgs. 1M or IV10 mgs. IVia-abnormallips, jaw, face, choreoathetotic movementsthe trunk; common:, protrusion ofof cheeks-often appears on withdrawal of-may also see a time-limitedtic meds, or decrease inia"
-7 -there are a number of uses of phenothiazine drugs, egoantiemesis, Gilles de la Tourette, which may not be seen aspsychiatric problems, therefore, diagnosis of T.D. may bemissed-an interesting presentation may be T.D. involving therespiratory muscles, may see respiratory compromise especiallyif medication has been suddenly stopped. Parenteral haloperidolis diagnostic as well as rapidly therapeuticConsultation Psychiatry-consider carefully whether the problem may be neurological, asocial service problem, or something truly psychiatric-Psychiatry cannot do much for OBS patients except to sedatethem adequately--we do not transfer them to 4-East-we do not treat alcoholics in JGH psychiatry:they shouldbe r e ferred directl y to MGH without involving us-for patients who refuse treatment--clarify patient's complaintbefore concluding it's a psychiatric problem; it may be amisunderstanding or one of many thingsSedation-consider possibility of inducing a toxic delirium in elderlypatients with long half-life BDZ's-low dose ego 1-2 mgs. 2-3x/day of high potency neurolepticsego haloperidol are often effective in treating agitation andtroublesome behaviour in dementia patients-remember, more brain damage means greater sensitivity topsychotropic drugs-consider possibility of pseudodementia(depression causingcognitive impairment )-extrapyramidal side effects can be treated with antiparkinsonmeds. but be careful re anticholinergic deliriumSedation of the Older Person-consider that l -life for BDZ's may be 3-4x longer than for youngadults-also, elderly are more sensitive to psychiatric tropic meds-BDZ with long }-lives, ego diazepam, flurazepam have activemetabolites with 100 hours lives--4 days in young, 2 weeksin elderly-takes several 1-lives for steady state, therefore, won't see finaleffect for weeks, example: okay initially, but confused weeks later- seemingly no cause--effect; no change when stop meds for weeks
LECTURE NOTES . Psychiatry in the Emergency Room January 1985 . H. alders, MD Psychiatric Emergencies . 1. Psychological states: -suicidal -depression -violence -fugue states -homosexual panic -other panic reactions -traumatic neurosis -mania -acute paranoid schizophrenia -acute catatonic . schi ophrenia -anorexia nervosa -acute psychosomatic issues: ego ICU and post-op patients . L.