Transcription
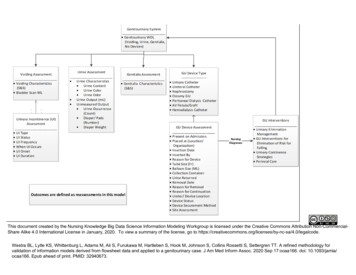
This document created by the Nursing Knowledge Big Data Science Information Modeling Workgroup is licensed under the Creative Commons Attribution Non-CommercialShare Alike 4.0 International License in January, 2020. To view a summary of the license, go to legalcode.Westra BL, Lytle KS, Whittenburg L, Adams M, Ali S, Furukawa M, Hartleben S, Hook M, Johnson S, Collins Rossetti S, Settergren TT. A refined methodology forvalidation of information models derived from flowsheet data and applied to a genitourinary case. J Am Med Inform Assoc. 2020 Sep 17:ocaa166. doi: 10.1093/jamia/ocaa166. Epub ahead of print. PMID: 32940673.
ConceptSynonymsDefinitionsGenitourinaryWithin DefinedSynonymsNo problems with voiding, urine, genitalia 80335‐3associated with voiding, nor any GUWithin DefinedLimits (WDL)WDL dingCharacteristicsSigns (objective data) or symptomsChanges in voiding80332‐0(subjective experience) of a genitourinarypatternsAlterations in voiding disease or change in conditionVoiding signs andsymptomsUse pain assessment conceptsAcute pain(abdomen, pelvis,back)AnuriaBladder fullnessBladder spasmDribblingDysuriaLA25308‐0Sensation of fullness a Persistent and strong desire to urinatewithout the fear of losing urineBladder muscle squeezes suddenlywithout warning, causing an urgent needto release urine.Post Micturition Dribble Uncontrolled leakage of urine.LA25310‐6Painful, Burning,discomfort: Painfulurination/micturitionSCT IDSCT TermGenitourinaryAssessmentWDLAssessment of the patient's ability toeliminate urineNonpassage of urine, in practice isdefined as passage of less than 100milliliters of urine in a dayVolume 500–600 mlBladder distensionLOINC NamePain, discomfort, or burning whenurinatingLA17661‐2Voiding PatternAnuria2472002 Anuria (finding)54768000 Bladder distention(finding)247335009 Sensation as if bladderstill full (finding)16844001 Painful urging to urinate(finding)DribblingDysuria58972000 Dribbling of urine(finding)49650001 Dysuria (finding)
EnuresisWetting/ involuntaryurination at nightloss of bladder control in children 3 andolderLA25319‐7enuresisFrequencyIncreased daytimefrequencyUrinating often during the dayLA25315‐5HesitancyDifficulty startingstream, strains to voidTrouble starting or maintaining a urinestreamLA25309‐8Increased urinaryfrequencyHesitancyLoss of bladder controlLA7445‐5Incontinence42112009 Urinary incontinence ofnon‐organic origin(finding) ‐‐ enuresis162116003 Increased frequency ofurination (finding)5972002 Delay when starting topass urine (finding) ‐‐synonym urinaryhesitancy48340000 Incontinence (finding)Nocturia139394000 Nocturia (finding)Urine output 1 mL/kg/h in infants, 0.5 LA25321‐3mL/kg/h in children, and 400 mL or 500mL per 24h in adults - this equals 17 or21 mL/hour. 3 Liters / dayLA25323‐9Inability to completely or partially emptythe bladderOliguria83128009 Oliguria (finding)Inability to urinateLA25325‐4Unable to voidSudden, compelling urge to s urge to voidNocturiaOliguriaPolyuriaRetention/ilExcessive night timeurinationLow output of urineExcessive urinationAbsence of urinaryeliminationUnable to voidUrgencyBladder Scan (mL)Numeric ValueOveractive bladderA decrease in the sensation of needing tovoidWaking up at night 2 timesLA25318‐9Amount of urine in the bladder aftervoiding, normla 100 mLPolyuria28442001 Polyuria (finding)130951007 Bladder retention ofurine (observableentity)44949100012 Unable to void urine4101 (finding)75088002 Urgent desire to urinate(finding)
UrinaryIncontinenceAssessmentUrinaryIncontinence t of issues that influenceincontinence which is the involuntary lossof urine in sufficient quantities as to be aproblemUnderlying causes and patterns ofinvoluntary loss of urineInvoluntary loss of urine due to nongenitourinary functional deficits includingaltered mobility, dexterity, cognitive orenvironmental barriersExperiences more than one type ofurinary incontinence i.e. stress and urge.is the complaint of involuntary leakageassociated with urgency and also withexertion, effort, sneezing or coughing.Involuntary loss of urine associated withbladder over-distention caused by underactive detrusor muscle or outletobstruction. Conceptual:Complaints ofinvoluntary loss of urine that occursunderconditions in Incontinenceassociated withwhich the bladder was not completelyemptied, what can be related to highresidual volume after urination and/or notpainful bladder, which is palpable ormaltreated after urination (Staskin et al.,2013). Operational: Note or report ofextravasation of urine due to excessivevolume in the bladder.InvoIuntary loss of urine with activitiesthat increase intra-abdominal pressure(e.g. coughing, sneezing, etc.)129847007 Functional urinaryincontinence (finding)413343005 Mixed incontinence(finding)397878005 Overflow incontinenceof uring (finding)22220005 Genuine stressincontinence (finding)
UrgeOveractive bladderinvoluntary loss of urine with a strongurge to void. is the complaint ofinvoluntary leakage accompanied by orimmediately preceded by urgency.UrinaryIncontinenceActiveResolvedCurrent state of presence of urinaryincontinenceUse existing code for type (above)This needs discussionUrinary OccurrenceFrequency ofUrinaryIncontinenceOnce a day or less1-2 times a day3 times a day ormoreFrequency or incidence of occurrence ofurinary incontinenceWhen UrinaryIncontinenceOccursDaytime onlyUrinary Occurrence422058003 Number of urinaryincontinence episodes(observable entity)28017001 Daytime (qualifiervalue)2546009 Night time (qualifiervalue)224943009 Night and day (qualifiervalue)Both day and nightSuddenUse one ofaboveThe time of day/night when urinaryincontinence occursNighttime onlyUrinaryIncontinence OnsetGradual87557004 Urge incontinence ofurine (finding)The length of time for the start of UI61751001 Gradual onset (qualifiervalue)385315009 Sudden onset (qualifiervalue)
Subjective estimate of how long theurinary incontinence has been occurringUrinaryIncontinenceDuration 6 months64748‐7SymptomsDuration (PhenX‐‐TRIAL)162442009 Time symptom lasts(observable entity)Clumps of blood in urineUrine is free from particles, ‐7CloudyLA25329‐6Mucous threads276409005 mucus in urine 6009 Urinary sediment(dfinding)276408002 stone in urine (finding)6 months to 1 year 1 yearUnknownUrine Assessment SynonymsAssessment of urine - both the qualityand quantityUrineCharacteristicsSynonymsQuality of urine (content, color, and odor)UrineCharacteristics:Urine ContentBlood clotsClearUrine ContentDefinitions: Refers to how clear the ntRed flecksSedimentDepositVisible particles or material in urineAppearance and persistence of multiplelayers of small to medium white bubblesin voided urinePresence of mucous or mucous threadsin urineWhitish color to urineRed blood cells in urineMatter in urineStonesCalculiHard masses of minerals in urineMucous167236000 Urine looks clear(fidning)7766007 Cloudy urine (finding)44947100012 Urine consistency frothy4102
UrineCharacteristics:Urine ColorAmberBlueBrownDark redGreenOrangePale yellowPinkRedUrine is a transparent (clear) fluid orfreshly voided urine is light yellow oramber in color.Normal color for urine caused by apigment called urochrome, possibledehydrationBlue urine is typically caused byMethylene blue ingestion[Discoloration can stem from numerouscauses of red urine. Old clot sedimentcan appear brown when suspended inurine of a certain concentration. Likewise,myoglobinuria and hemoglobinuria oftenappear brown.Hematuria, red orRed includes the colors like pink; shadespinkof red, brown orange or even blackdepending upon who views the sample.Urine discoloration can also produce agreen urine hue when combined with theyellow color urochrome produces.Orange urine discoloration results frommedication useStrawNormal color for urine caused by apigment called urochrome , well-hydratedPink color to urine, may be caused byeating beeets, blueberries or rhubarbBloody, dark red, hemaRed urine discoloration due tohemoglobinuria may present in hemolyticdisorders, as in “march hematuria”observed in troops.ed urine can range inintensity from a pink lemonade color(clear light pink) to that of tomato soup(active thick bleeding) to a deep opaquemerlot color (liquefying clot). Hematuria,or blood in the urine5778‐6 Color of Urine102867009 Discolored urine(finding)44913100012 amber colored urine4105 (finding)449111000124104449101000124102blue colored urine(finding)brown colored urine(finding)44909100012 green colored urine4108 4107449051000124102orange colored urine(finding)straw colored urine(finding)pink colored urine(finding)red colored urine(finding)
RustyDark orange or brown color, may be apossible symptom of jaundice,rhabdohyolysis or dehydrationNormal color for urine caused by apigment called urochrome and howdiluted or concentrated the urine isYellowUrineCharacteristics:Urine OdorAmmoniaUrine OdorRefers to the smell from your urineFecal odorFruitysmell of fecesSweet smelling urine (f smells sweet or like fruitMalodorousMalodorous urine (find smells unpleasant or foulUrine OutputUrine OutputUnmeasuredOutput: UrineOccurrenceUnmeasuredOutput: Diapers/Pads (Number)162134004 urine looks normal(finding)34533‐0Odor of Urinesmell of ammonia10579003 Finding of odor of urine(finding)167248002 urine smellsammoniacal (finding)773318006 sweet smelling urine(finding)278017001 malodorous urine(finding)The amount of urine excreted by thekidney usually measured in mLUrine Output (mL)Unmeasured UrineOutput44925100012 rusty colored urine4106 (finding)9187‐6 Urine OutputIndirect methods to measure urine Usedfor unmeasured urine output (e.g.incontinence or unable to measure(missed the collection device but didvoid)Count of the frequency of incontinenceepisodesThe number of diapers or pads countedas a measure of urine output252109000 Number of times(qualifier value)
Wet diaper weight - dry diaper weightmeasured in grams and translated tomilliliters (1 gram 1 ml)UnmeasuredOutput: sessmentBleedingAssessment of genitalia associated withor influencing urinationrelease of blood from the circulatorysystemflow of substance from where it has beenconfinedpenile, vaginalDiscomfortEnlarged scrotumpainScrotal swellingUse pain assessment conceptsSwelling or edema of the scrotumExcoriationAbrasion, scratchingdamaged part of the surface of the skinItchingLesionsIrritation or pruritisMassLumpexperience an itcha region in an organ or tissue which hassuffered damage through injury ordisease, such as a wound, ulcer,abscess or tumora coherent, typically large body of matterwith no definite shapeRednessFluid outputurinaryincontinenceEstimatedAssessment of genitalia associated withor influencing urinationDischargeRash9185‐0an area of reddening of a person's skin,sometimes with raised spots, appearingespecially as a result of allergy or illnessthe quality or state of being red orreddish131148009 Bleeding (finding)307488001 Discharge ‐ substance(substance)271687003 Swelling of Scrotum(finding)723016004 Acute excoriation ofskin (finding)418290006 Itching (finding)300582001 Multiple lesions(finding)300848003 Mass of body structure(finding)827160004 Rash (finding)386713009 Redness (finding)
Swellingan abnormal enlargement of a part of thebody (not edema)GU DeviceAssessmentSynonymsGU Device TypeObservation at a point in time of a type ofmedical product that can be invasive ornon-invasive intended for the care ortreatment of GU condition.A type of indwelling urinary catheterwhich has a slightly angled or curved tipand is used for patients where it isdifficult to insert a regular straight tipCondom catheterCatheter placed outside the body,LA25314‐8typically for men. A device that looks likea condom covers the penis head and atube leads from the condom device to adrainage bag. An external urinarycatheter also exists for women.Urethral catheter, doubA soft plastic, silicone or rubber tube witha balloon attached that is inflated to keepthe catheter in place in the bladder. Thecatheter is inserted through the urethraand is used to decompress a distendedbladder, collect urine, and monitor patienturine outputStraight catheterA small hollow, flexible tube that is usedto empty urine from the bladderintermittentlyCoudeExternal urinarycatheterIndwelling urinarycatheterIntermittentcatheter65124004 Swelling (finding)Assessment criteria related to use of amedical product that can be invasive ornon-invasive intended for care ortreatment of a GU condition.Condom Catheter337636000 Incontinence sheath(physical object)23973005 Indwelling urinarycatheter, device(physical object)470027009 Intermittent urethraldrainage catheter, non‐sterile (physical object)
NephrostomyCatheter (simple angiographic, pigtail, orself-retaining) placed percutaneously orsurgically for external drainage of therenal collecting system in a patient with ahigh-grade urinary tract obstruction,provision of an access route forplacement of a ureteral stent, provision ofa route for extraction of a renal orureteral calculus, treatment of a urinarytract infection superimposed on a urinaryobstruction, or treatment of urinary tractleaks and fistulas.Ureteral catheterCatheter that is designed to be placed toaid access for delivery of contrast or aguidewireUrostomyPouch, Ostomy (urine) Surgically created opening to drain urine LA25328‐8after the bladder has been removed orbypassed.SuprapubicIndwelling urinary catheter which isLA25324‐7placed surgically or percutaneously in theabdomen and are typically sewn in placeand attached to a drainage bag. Usuallyused for long-term urinary drainage.Triple lumenCatheter with a third channel which isurinary catheterused for continuous bladder irrigation orfor instillation of medication. Also calleda 3 way catheter.Indwelling urinary catheter which has aTemperatureelectrically insulated thermistor probe in amonitoring urinarysecondary lumen with a sensor near thecathetertip of the catheter to monitor the patient'surine (body) temperature.286628000 Nephrostomy tube(physical object)47528002 Ureteral catheter,device (physical object)Urostomy344088002 Urostomy bag (physicalobject)Suprapubiccatheter286861005 Suprapubic catheter(physical object)470611003 Indwelling urethraldrainage/irrigationcatheter (physicalobject)466565001 Temperature‐monitoring indwellingurethral drainagecatheter (physicalobject)
GU Device Preexisting DevicePresent OnAdmissionYesNoA GU device is present on admission to ahospital or other type of health careorganizationGU Device Placedat Location/OrganizationOutside facilityOutside hospitalHome (selfcathing)EMSCurrent facilityUnknownPre-existingInsertion DateUse Fuzzy dateLocation or an organization where patientwas when a GU device was placedInsertion Date/Time thisencounterDate /Timecalendar date and time of catheterinsertionInserted byDepartment where patient was locatedwhen a GU device was insertedDepartment in a hospital whereinterventional cardiac procedures areperformedDepartment in a hopsital wherehemodialysis is performedCath labDialysis unit38810001751 Clinical finding present03 on admission (situation)fuzzy date (less than complete date) ofcatheter insertion72052‐4Date catheterplacement418518002 Dialysis unit(environment)
EmergencydepartmentDepartment in a hospital whereemergency care is providedEmergencymedical servicesPre-hospital care staff who provideemergency servicesInfusion roomDepartment in a hospital or clinic whereinfusions are administered to patientsDepartment in a hospital where patientsare treatedDepartment in a hospital or clinic whereoperative and interventional proceduresare performedDepartment in a hospital or clinic whereradiological studies are performed440654001 Inpatient environment(environment)225738002 Operating theatre(environment)Reason for DeviceRationale for why a device was used.410665000 Indication for (attribute)AnesthesiaPatient is receiving anesthesiaAnticipated largevolume infusions ordiureticsAssist in healing ofperineal & sacralwounds inincontinent patientChemotherapy withincontinenceClose urine outputmonitoringPatient will be given large amounts ofintravenous fluid or diuretics to increaseurine outputPatient has perineal or sacral woundswith incontinence. The device is insertedto prevent the effects of incontinence andaid wound healingPatient has urinary incontinence and isreceiving chemotherapyThe patient's urinary output needs to beclosely monntored by the treatment teamto determine effectiveness ofinterventions and overall statusThe patient is near the end of life and thedevice will prevent additional discomfort421642003 Under anesthesia(finding)718402002 Increased urine output(finding)Inpatient unitOperating roomRadiologyEnd of life/ comfortcare225728007 Accident andEmergency department(environment)409971007 Emergency medicalservices (qualifier value)request code309964003 Radiology department(environment)183001000 Incontinence care(regime/therapy)183001000 Incontinence care(regime/therapy)130953005 Rate of urine output,function (observableentity)385736008 Dying care(regime/therapy)
Gross hematuriaNeurogenicbladderObstructionRetentionThe patient has blood in their urine whichthey can seeA number of urinary conditions in peoplewho lack bladder control due to a brain,spinal cord or nerve problem. Problemswith these nerves cause overactivebladder (OAB), incontinence, andunderactive bladder (UAB) or obstructivebladder, in which the flow of urine isblocked.The patient has an inability to voidbecause of an obstruction in the urinarytractThe patient retains urine after voidingPost-surgicalprocedureTransplantThe patient has had a surgical procedureThe patient has received a transplantParalytic agentsThe patient is receiving a paralytic agentTube Size (Fr)Catheter outer diameter in millimeters-French scale197941005 Frank hematuria(disorder)398064005 Neurogenic bladder(finding)7163005 Urinary tractobstruction (disorder)130951007 Bladder retention ofurine (observableentity)do not code77465005 Transplantation(procedure)do not codeNumericBalloon Size (mL)NumericCatheter balloon size in millilitersGU DeviceCollectionContainerBelly bagDefinition: Type of urine collectioncontainerDrainage bagAlternative to a leg bag, collects urineand is attached to the abdomenUrinary drainage bag Bag used to collect urine30968007 Drainage bag,
Leg bagBag used to collect urine which isattached to the legBag used to collect urine from aurostomyUrostomy bagRemoval DateDatecalendar date of catheter removalReason forRemovalDevice damagedReason for removal of deviceDevice has been damaged in some wayso it no longer functions as expectedThe therapy or treatment that requiredthe device has been completedThe device is no longer needed and canbe removedThe device is occluded and no longerfunctions as expectedThe device is causing pain to the patientTherapy/treatmentcompletedNo longer indicatedOccludedPainPer patient/familyrequestPer protocolRemoved bypatientSuspectedinfectionReason forContinuationAccurate intake &outputPer order338000001 Leg bag (physicalobject)344088002 Urostomy bag (physicalobject)72051‐6Date catheter removal182992009 Treatment completed(situation)request code263823007 Occluded (qualifiervalue)22253000 Pain (finding)do not codedo not codeDevice has been removed by the patientInfectionThere is a suspected infection which maybe related to or caused by the deviceReason (necessity) for not removingFoley catheterMeasurement of a patient's fluid intake bymouth, feeding tubes, or intravenouscatheters and output from kidneys,gastrointestinal tract, drainage tubes, andwounds473130003 Suspected infectiousdisease (situation)63061008 Measuring intake andoutput (procedure)
AnesthesiaAssist in healing ofperineal & sacralwounds inincontinent patientComfort care/endof lifeContinuous bladderirrigationEpidural/intrathecalcatheterState of controlled, temporary loss ofsensation or awareness that is inducedfor medical purposes.Patient has perineal or sacral woundswith incontinence. The device is insertedto prevent the effects of incontinence andaid wound healingCare to prevent or alleviate suffering nearthe end of lifeProcedure used continuously to flush sterilefluid through your catheter and into yourbladderGross hematuriaIntrathecal administration is delivereddirectly into the CSF and into thesuperifical spinal cord; epiduraladministration diffuses through the durainto the CSF, and thus has a sloweronset of action.Visible blood in urineImmobilized patientDecreased ability to moveIncontinenceInvoluntary leakage of urineKnown orsuspected urinarytract obstructionBlockage that inhibits the flow of urinethrough its normal path (the urinary tract),including the kidneys, ureters, bladder,and urethra. Blockage can be completeor partial.Lack bladder control due to a brain,spinal cord or nerve problemNeurogenicbladder421642003 Under anesthesia(finding)183001000 Incontinence care(regime/therapy)385736008 Dying care(regime/therapy)771555004 Monitoring ofcontinuous bladderirrigation(regime/therapy)30610008 Epidural catheter,device (physical object)197941005 Frank hematuria(disorder)257884004 Immobilization ‐ action(qualifier value)165232002 Urinary incontinence(finding)7163005 Urinary tractobstruction (disorder)398064005 Neurogenic bladder(finding)
Paralytic agentsBlockage of neuromuscular transmissionat the neuromuscular junction, causingparalysis of the affected skeletalmuscles.Inability to empty bladder of all urineRetentionPer policyThe patient meets criteria in aninstitution's policy to continue use of anindwelling urinary catheterGU Device Ureter /Device LocationLeft ureterPhysical location of the device or bodylaterality of the device locationureter on the left side of the bodyRight ureterureter on the left side of the bodyDevice StatusClampedState of a device related to intactnessDevice is clamped, allowing no drainageGU DeviceSecurementMethodPhysical attachment of device to preventaccidental removal, reduce trauma (tothe urethra and bladder), and/or reduceinflammation of urinary tissues.Strap used to secure a urinary catheterdrainage bag to the patient's legSupply used to secure a urinary drainagecatheter to the patient's body, usually thethighLeg strapSecuring deviceTapeSecuring deviceGU Device SiteAssessmentBleedingAssessment of the bodily location when adevice is in useRelease of blood from the circulatorysystemdo not code130951007 Bladder retention ofurine (observableentity)do not code26559004 Structure of left ureter(body structure)25308007 Structure of right ureter(body structure)request code448439004 Catheter stabilizationdevice (physical object)401604001 Catheter retainer strap(physical object)131148009 Bleeding (finding)
BlisteredSmall pocket of body fluid (lymph, serum,plasma, blood, or pus) within the upperlayers of the skin, typically caused byforceful rubbing (friction), burning,freezing, chemical exposure or infectionFree from abnormal findingsColor approaching black around theedgesFree from moisture or liquidDarkish in colorCleanDark maExcoriatedRedIntactLeakingNormal colorMaceratedMoistHealedPainfulScabbedClean, dry andintactDry dressingTender339008 Blister (morphologicabnormality)73112009 Dark color (finding)13880007 Dry (qualifier value)48786000 Bluish red color (finding)An area of discolored skin on the body302227002 Ecchymosis (finding)Excess of watery fluid collecting in thecavities or tissuesSuperficial reddening of the skinDamaged part of the surface of the skin267038008 Edema (finding)Not damaged or impaired in any wayLosing liquid through a crack or holeOversaturated skin from prolongedexposure to moistureSlightly wet or dampSite is sound and healthyAffected with painEncrusted or covered with a scab orscabsSite of device is free from abnormalfindings, moisture or liquid and notdamaged or impaired in any wayDevice dressing is free from moisture orliquid247441003 Erythema (finding)400048001 Excoriation(morphologicabnormality)11163003 Intact (qualifier value)87952002 Leaking (qualifier value)3644009 Macerated skin (finding)17461003 Wet (qualifier value)22253000 Pain (finding)69640009 Crust (morphologicabnormality)
GenitourinaryInterventionsDefinitions: Actions to improve ormaintain optum urinary eliminationUrinary EliminationManagementBladder trainingmanagementMaintenance of optimum urinaryelimination patternBladder training, also known asscheduled voiding and bladder reeducation is urinating at specific times ofthe day. It is used as a first line treatmentof overactive bladder or mixed urinaryincontinence.Provide care for the urinary systemdeviceCare of urinarysystem deviceCollection of urineand strain forcalculusEducation aboutbladder voidingtechniqueFluid intakeencouragementCollect and strain urine to examine forurinary calculi. May be random collectionor 24-hour collection.Education of patient/family regardingbladder training techniques.BriefsIncontinence/absorbent pad/garmentmanagementIrrigation of urinarybladderUse of incontinence/absorbent pad toprevent skin breakdown for incontinentepisodesPerineal carePositioningaccessible toiletingdeviceEncouraging increased intake of fluids.Injection of sterile fluid into bladder viaurinary catheter to flush or wash outclots, sediment, or other urinary content.Cleanse and dry the external genitaliaand anal area, and inspect forPlacing a toileting device close to thepateint so it is easily accessible385969003 Bladder trainingmanagement(procedure)737944006 Care of urinary catheter(regime/therapy)37020001 Collection of urine andstrain for calculus(procedure)704117005 Education aboutbladder voidingtechnique (procedure)113148007 Fluid intakeencouragement(regime/therapy)718250000 Absorbent underpad,non‐sterile (physicalobject)78533007 Irrigation of urinarybladder (procedure)385958001 Perineal care(regime/therapy)request a more generalterm than commode
Positioning forurinationPromotion of useof progressivemuscle relaxationtechniqueUltrasonography ofurinary bladder forpost-void residualvolumeUrinary infectionpreventioneducationUrine specimencareoptimizing bladder emptying bypositioning patient e.g. sitting on toiletingdeviceUse of muscle relaxation to promotebladder emptyingUltrasonography measurement ofresidual urine in bladder after voiding.Meaured in milliliters.710124007 Promotion of use ofprogressive musclerelaxation technique(procedure)Teaching patient/family about urinaryinfection prevention700387001 Ultrasonography ofurinary bladder for post‐void residual volume(procedure)request new code(more specific)Proper collection, storage and handlingof a urinary specimen385842003 Urine specimen care(regime/therapy)GU Interventionsfor Elimination ofRisk for FallingAmbulation therapymanagementDefinitions: Interventions associated withfall risk related to eliminationPositioningaccessible toiletingdeviceAttend patientwhen upProvision offootwearPositioning forurinationPlacing a toileting device close to thepateint so it is easily accessibleAssistance with mobility (match with FallRisk Management Interventions)Remaining with the patient when out ofbed to toilet to decrease the risk of fallingEnvironmental safety management forFall Riskoptimizing bladder emptying bypositioning patient e.g. sitting on toiletingdevice370873006 Ambulation therapymanagement(procedure)request term (seeabove)313420001 Assisting with toileting(regime/therapy)302807005 Provision of footwear(procedure)
Transfer assistivedevice useDevice used to help the patient transferfrom one position or location to anotherProvision oftoileting aidIncontinence/absorbent pad/garmentmanagementAssistive device to help the patient withtoileting is providedUse of incontinence/absorbent pad toprevent skin breakdown for incontinentepisodesUrinary ContinenceStrategiesProvision oftoileting aidBladder ControlMedicationInterventions to prevent or treat urinaryincontinenceAssistive device to help the patient withtoileting is providedMonitoring effects of bladder controlmedication(s), adherence to medication,side effectsExercise, drinking enough water andeating high-fiber foods can help preventconstipation which can damage the pelvicfloor by straining during bowelmovementsPlacing a toileting device close to thepateint so it is easily accessiblePrevention ofconstipationPositioningaccessible toiletingdeviceFluid intakemanagementBladder trainingmanagementPrevent excessive fluid intake e.g.Limiting fluid intake to decrease thelikelihood of an incontinent episodeHolding off on voiding to delay urinationafter getting the urge to go, with the goalof lengthening the time between trips tothe toilet and retraining the bladder tohold more urine705413009 Transfer/turningassistive device(physical object)736858000 Provision of toileting aid(procedure)736858000 Provision of toileting aid(procedure)18629005 Administration of drugor medicament(procedure)713115004 Prevention ofconstipation(procedure)717244008 Fluid intakemanagement(procedure)385969003 Bladder trainingmanagement(procedure)
Promotion ofbladder routineUrinaryincontinence careeducationKegel exercisesPerineal CareIncontinence/absorbent pad/garmentmanagementPerineal cleansingBathing patient insitz bathTimed voidingScheduling trips to the toilet to urinaterather than waiting until the bladder isfull, without waiting for the urge or needEducation about care for urinaryincontinence provided to the patientand/or family/caregiver, includingavoiding food irritants (i.e. caffiene) andregular exercisePelvic Muscle exercise Excercises designed to strengthen thepelvic floor and urinary sphincter m
catheter Condom catheter Catheter placed outside the body, typically for men. A device that looks like a condom covers the penis head and a tube leads from the condom device to a drainage bag. An external urinary catheter also exists for women. LA25314‐8 Condom Catheter 337636000 Incontinence sheath (physical object) Indwelling urinary catheter










